INTRODUCTION
The presence of left ventricular hypertrophy (LVH) is associated with an increased risk of sequelae from cardiovascular disease [
1]. Reports have documented risk factors for the development of LVH such as age, elevated blood pressure (BP), obesity, stature, and glucose intolerance. Cardiac valve disease and chronic heart disease also cause LVH [
2]. Regression or prevention of LVH are known to be associated with the reversal of an adverse cardiovascular prognosis [
1]; thus, understanding of the development of LVH and suggesting individualized strategies are important. In this regard, LVH in hypertensive patients is relatively easy to interpret as it is evidence of hypertensive target organ damage [
3], but the clinical significance or interpretation of LVH found incidentally in normotensives is uncertain [
4]. Furthermore, to investigate determinants of LVH, most studies [
1,
3,
5-
7], except for a few [
4,
8], have been performed in hypertensive patient populations.
On the other hand, although LVH can be diagnosed either by electrocardiography (ECG) or by echocardiography (ECHO), owing to its low cost and non-invasiveness, ECG is more available in primary health care assessment and for the health screening of asymptomatic visitors. Thus, the issue of a correct interpretation of LVH found incidentally in normotensives will arise mainly after the observation of electrocardiographic LVH (ECG-LVH) rather than by echocardiographic LVH (ECHO-LVH).
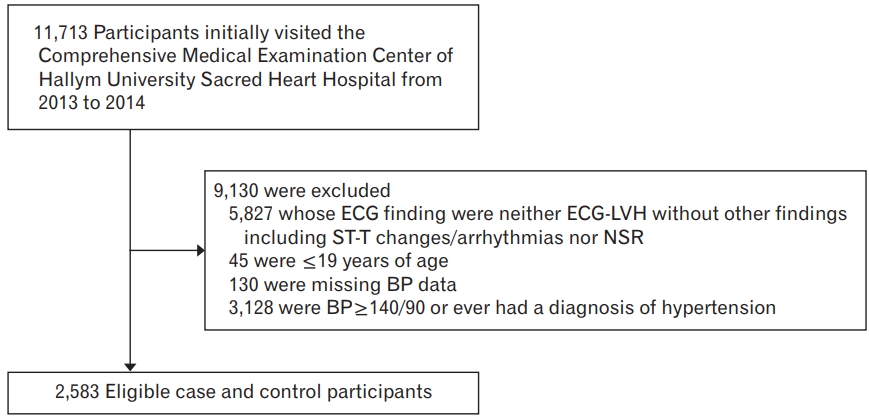
Therefore, we investigated factors independently associated with ECG-LVH determined by commonly used Sokolow-Lyon or Cornell criteria [
9] in participants who were normotensives on clinical measurement and who had never received a diagnosis of hypertension, in the context of exploring the clinical implications of ECG-LVH in such population.
DISCUSSION
The presence of LVH is associated with a significantly increased risk of cardiovascular complications, irrespective of whether it is determined by ECG or ECHO [
1,
2]. In fact, ECHO is the gold standard for assessing anatomical LVH. While ECG shows a high specificity in diagnosing anatomical LVH, its sensitivity is relatively low [
1]. However, considering that ECG-LVH may predict cardiovascular mortality and morbidity independently of ECHO-LVH and ECG provides information not available from ECHO (i.e., ECG-LVH may not depend solely on left ventricular mass suggesting that anatomical ECHO and electrical ECG versions might reflect different pathogeneses) [
1], the interpretation of the clinical significance of ECG-LVH once discovered, rather than questioning whether or not to exclude the LVH diagnosis may differ in importance. The present study is, as far as we know, the first to investigate factors associated with ECG-LVH in both sexes by targeting only clinical normotensives with no prior history of hypertension from the Korean population. This information is clinically relevant as it may improve the usefulness of ECG because it facilitates clinical decisions associated with ECG-LVH.
For all participants, male sex, age, and SBP were independently and positively associated with the presence of ECG-LVH. Although it was found attenuated after adjustment for potential confounding factors, the association remained significant for most outcomes. These findings are consistent with those of previous studies. The prevalence of ECG-LVH increases with age [
1,
2,
5]. In ECG-LVH according to Sokolow-Lyon criteria, there is a male predominance [
1,
5]. Furthermore, the incidence of ECG-LVH is closely associated with BP levels [
1,
2,
5]. With respect to SBP, there are some possible mechanisms through which BP may influence left ventricular growth in our study of clinical normotensives with no prior history of hypertension. First, the association of SBP with an increased risk of ECG-LVH may be explained by responses to high normal BP. SBP levels within the normal limits have been shown to influence the increasing prevalence of LVH [
16]. Second, it can be hypothesized that the association of ECG-LVH with male sex, older age, and relatively higher clinical SBP is a result of masked hypertension (MH) playing a significant role in the genesis of hypertrophy. MH is defined as normal BP on measurement in the clinic but a hypertensive BP level on ambulatory measurements [
17]. The risk of cardiovascular morbidity and mortality in patients with MH is close to that of patients with uncontrolled hypertension [
18]. A relatively higher SBP in the clinic is associated with MH in several studies [
19-
21], while other associated factors of ECG-LVH in our study, such as male sex and older age have also been shown to be factors associated with MH in previous studies [
21]. Moreover, this explanation is in accordance with a previous report in which ECG-LVH was shown to be an independent determinant of MH [
22].
In men, ex-smokers were associated with increased risk of ECG-LVH compared with never-smokers. Although the relationship was not statistically significant, current-smokers were also associated with increased risk of ECG-LVH. In agreement with our observation, hypertensive patients with ECG-LVH according to the Sokolow-Lyon criteria in other studies were more likely to be current smokers than participants without ECG-LVH [
6]; and ever smokers in men [
1]. Meanwhile, a significant effect of smoking on ECG-LVH was observed exclusively in men, but not in women. The fewer number of ex-smokers and currentsmokers in women compared to men might hinder an accurate estimation of the effects of smoking on ECG-LVH in women.
In women, uric acid was inversely associated with the presence of ECG-LVH. Unlike our results, previous studies have found that uric acid is independently and positively associated with ECG-LVH [
6,
23]. These contradictory results could be a result of confounders. Considering that the complex metabolic changes associated with menopause have been found to be linked to serum uric acid levels, and women taking HRT have been shown to have significantly lower serum uric acid concentration than those who did not take HRT [
24]; we also assessed the relationship between uric acid levels and ECG-LVH after adjustments for menopause or HRT (
Supplementary Table 6). Adjustment for HRT attenuated the association between uric acid and the presence of ECG-LVH (
Supplementary Table 6, models B and D). However, information on HRT in the present study was available for only about one tenth of the female participants. The analysis with HRT as covariate was limited by the small sample size and was not adequately powered to definitely determine whether HRT may moderate the effects of uric acid on ECG-LVH. On the other hand, we identified an association between uric acid levels and ECG-LVH status in women, but not in men. The association of uric acid with menopause and HRT outlined above might also explain sex differences.
With respect to physiologic LVH which is a functional and structural adaptation of the heart to vigorous physical training and differs fundamentally from pathologic LVH [
25], we further examined factors associated with ECG-LVH in regular exercise-stratified analyses setting a limit to age and diagnosis histories. Analyses were performed only in relatively healthy young men, because among women who exercised regularly, none exhibited ECG-LVH, which might be related to previous report that in comparison to men, athletic training in women athletes was not a stimulus for substantial increase in left ventricular wall thickness [
26]. In the non-regular exercise group, older age and higher SBP were associated with an increased risk of ECG-LVH, while obesity was associated with a decreased risk of ECG-LVH. In the regular exercise group, only PR showed a statistically significant (inverse) association with the presence of ECG-LVH. Neither age nor SBP was significantly associated with the presence of ECG-LVH. In that specific cardiovascular risk factors such as higher BP and older age were not associated - in terms of direction, even showing inverse relations of age and SBP to the presence of ECG-LVH – ECG-LVH in the regular exercise group might be fundamentally different from ECG-LVH in the non-regular group in the context of physiological versus pathological LVH. The inverse relationship of PR with the presence of ECG-LVH in the regular exercise group is in accordance with other studies which revealed that resting sinus bradycardia was the most frequent ECG finding of well-conditioned athletes [
27].
On the other hand, ECG-LVH according to the Cornell criteria has been found to be positively related to obesity, consistent with the known relationship of anatomic LVH to obesity [
2,
6,
8]. In contrast, ECG-LVH according to the Sokolow–Lyon criteria has been found to be negatively associated with obesity in hypertensive patients as previously described in the literature. This suggests that the Sokolow–Lyon criteria identifies ECG-LVH in which obesity does not play a significant role in the genesis of hypertrophy and, in addition, reflects the negative influence of obesity on precordial voltage amplitudes in hypertensives and subsequent a lower sensitivity of the Sokolow-Lyon criteria for LVH in obese patients [
1,
6]. In this study, to increase the sensitivity for detecting ECG-LVH, both the Cornell and the Sokolow-Lyon criteria were accepted for defining ECG-LVH, because the Cornell criteria have been shown to be less dependent on body status also in the Korean population [
11]. However, of the total 76 participants with ECG-LVH who were normotensives on clinical measurement and did not have a prior diagnosis of hypertension, only three participants fulfilled both the Sokolow–Lyon criteria and the Cornell criteria, and only one participant fulfilled the Cornell criteria alone. Consequently, the presence of ECG-LVH in our study was defined mostly by the Sokolow–Lyon criteria, and although not statistically significant except for the four models that adjusted for monthly household income, a history of stroke, PR, or AST in all participants, the inverse effects of obesity in our study were in accordance with the results of other studies on hypertensive patients [
1,
6]. Regarding statistical significance, men with ECG-LVH were more likely to do regular exercise than those with NSR (
Table 1), and this might attenuate the association of obesity with the presence of ECG-LVH. Because the relationship between obesity and ECG-LVH in past investigations was observed in hypertensive patients [
1,
6], the ECG-LVH in hypertensive patients was a manifestation of heart disease, and physiologic LVH is different from pathologic LVH in nature [
25]; including men who did regular exercise – who were more likely to have physiologic LVH rather than pathologic LVH compared with those who did not regular exercise - in analyses might attenuate the effects of obesity on ECG-LVH. Further regular exercise-stratified multivariable logistic regression analyses suggested that in the non-regular exercise group, obesity was independently and negatively associated with the presence of ECG-LVH, while in the regular exercise group, obesity showed no statistical significance, possibly providing an explanation for the non-significant association found on multivariable analyses in all participants. Meanwhile, in the non-regular exercise group, the presence of ECG-LVH was also defined mostly by the Sokolow-Lyon criteria (n for total ECG-LVH=16; n for fulfilling the Sokolow–Lyon criteria alone=15; n for fulfilling both the Sokolow–Lyon criteria and the Cornell criteria=1; n for fulfilling the Cornell criteria alone=0). As indicated above, it must be admitted that the inverse relationship of obesity with the presence of ECG-LVH in the non-regular exercise group may be an artifact of the ECG-LVH measurement by the Sokolow-Lyon criteria, since obesity of the chest wall will have a negative influence on precordial voltage amplitudes. Moreover, previous investigators have found a positive association of obesity with ECHO-LVH [
2,
6,
8] or the ECG-LVH defined by the Cornell criteria [
1,
6], as described above.
Our study has some limitations. Owing to the relatively small number of case participants, it is possible that the statistical power for assessment was insufficient especially in analyzing the data in men and women separately.
Indeed, analysing the data in men and women separately, the statistical significance of relation of age to the presence of ECG-LVH was observed only in women, and the statistical significance of relation of SBP to the presence of ECG-LVH was observed only in men besides two models of female analysis. However, when we analyzed participants who did not exercise regularly in the regular exercise-stratified analyses [
28], the relations of age and SBP to the presence of ECG-LVH remained virtually the same for all participants, as noted. It is possible that the sex difference observed when we analyzed the data in men and women separately, could be explained by sex-specific, relatively close or weak relationships between ECG-LVH and other cardiovascular risk factors [
3].
The study was cross-sectional in design; therefore, we could not identify the causal relationships between ECG-LVH and several factors. In this context, ECG-LVH in the regular exercise group might not have been a consequence of exercise, nor representative of physiologic LVH, although our observations showed significant differences between the regular exercise group and the non-regular exercise group. Further longitudinal studies will be needed in the future.
In addition, we had intended to apply the two most widely used ECG-LVH criteria—the Sokolow-Lyon and the Cornell criteria. In recent guidelines, detection of ECG-LVH defined according to the Sokolow-Lyon and Cornell criteria appears in the list of routine tests to determine target organ damage in hypertension [
9]. However, the presence of ECG-LVH in our study was defined mostly by the Sokolow–Lyon criteria as mentioned above, and thus, we were unable to determine whether combining the two ECG-LVH criteria would produce the same results. Furthermore, eligible case participants included those with only ECG-LVH defined according to the Sokolow-Lyon and Cornell criteria without other ECG findings including ST-T changes and arrhythmias, and although this restriction could reduce any potential confounding factors, participants selected on the basis of isolated voltage ECG-LVH might not be common patients with ECG-LVH. Thus, caution must be exercised when our results are extrapolated and applied to the general population and other specific subgroups.
In conclusion, male sex, older age, and higher SBP were associated with ECG-LVH in participants who were normotensives on clinical measurement with no prior diagnosis of hypertension. The positive relation of smoking and regular exercise; inverse relation of PR to the presence of ECG-LVH were found only in men. The inverse relation of uric acid level was found only in women. Detailed analyses of relatively healthy young men according to whether or not they exercise regularly showed that in the non-regular exercise group, age and SBP to be positively related to the presence of ECG-LVH, while obesity to be negatively related. However, in the regular exercise group, neither age nor SBP was significantly associated with the presence of ECG-LVH, and only PR showed a statistically significant (inverse) association. The varying risk factor profiles associated with ECG-LVH based on sex and whether or not to exercise in our study may help to elucidate the ECG-LVH in clinical normotensives with no prior history of hypertension. Further longitudinal studies in general populations will be needed to better understand the development of ECG-LVH.