|
 |
- Search
| Korean J Fam Med > Volume 34(1); 2013 > Article |
A 62-year-old female patient with hypertension presents to her general practitioner (GP) for her annual review. She is taking indapamide 2.5 mg once a day, and has just returned from holiday in the Canary islands. Blood tests show a hematocrit percentage of 56%, and the patient asks her GP if a high hematocrit count is a serious problem.
Polycythemia refers to a condition of multi-factorial etiology in which the hematocrit percentage is greater than 51% in men and greater than 48% in women. A thorough anamnesis and physical examination is essential, coupled to specific laboratorial analysis to reach the correct diagnosis.
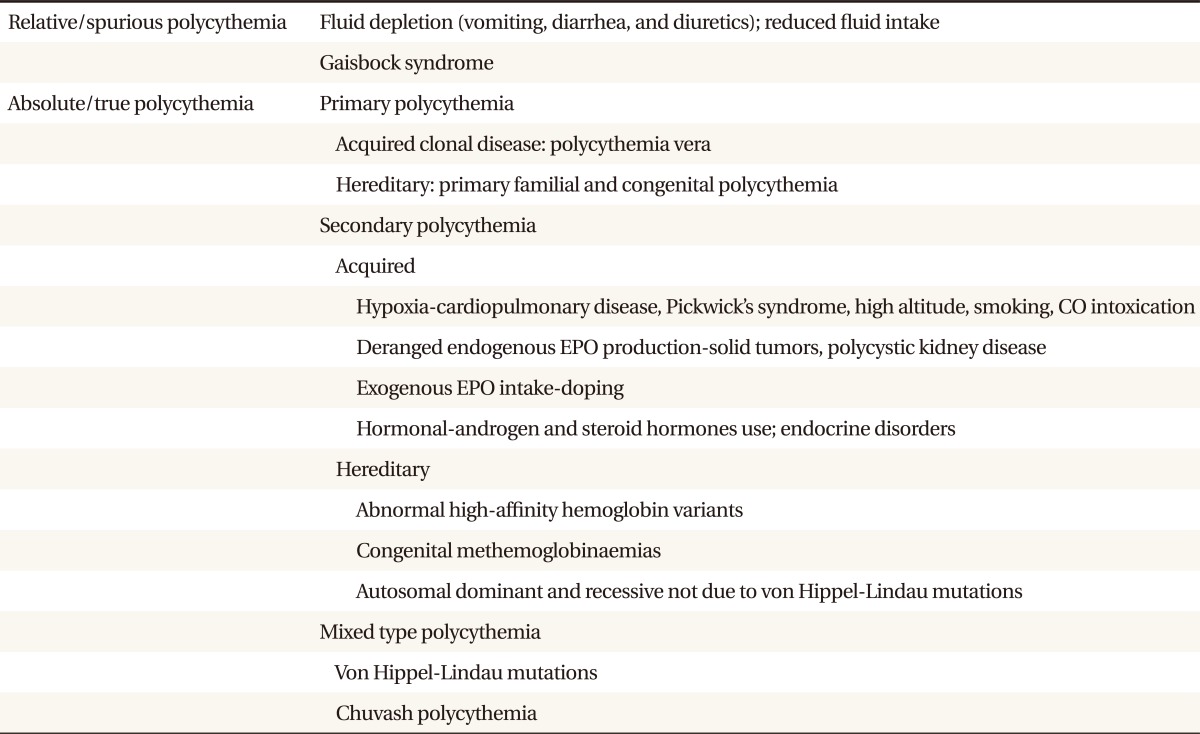
First and foremost, it should be ascertained if it is a relative/spurious polycythemia or an absolute/true polycythemia. In this regard, the blood counts should be repeated to see if the high hematocrit is due to a transient decrease of plasma volume (dehydration and diuretics use), Gaisbock syndrome (pseudopolycythemia/apparent polycythemia), or if the hematocrit and hence the red cell mass is persistently elevated. After ruling out the presence of spurious polycythemia, attention should be focused on the causes of true polycythemia, namely primary and secondary polycythemias. Primary polycythemias are disorders in which the erythroid progenitors are hypersensitive to very low levels of erythropoietin while secondary polycythaemias are characterized by an increased red cell production owing to a physiologic response to hypoxia or to a deranged and exaggerated production of erythropoietin (Table 1).
1) Presence of family members with polycythemia and low levels of serum erythropoietin (<5 UI/L) are more suggestive of a diagnosis of primary familial and congenital polycythemia, while in the face of a history of thrombosis (stroke and transient ischemic attack), peptic ulcer, high blood pressure, complaints of pruritus, burning sensation of the hands and feet, dizziness, headache, physical examination showing splenomegaly, blood tests showing thrombocytosis and/or leukocytosis, elevated uric acid and vitamin B12 levels, or low ferritin, an acquired clonal disorder such as polycythemia vera is highly likely.
2) Cyanosis and high serum erythropoietin (>5 UI/L) indicates heavy smoking, high altitude dwellers, congenital right-to-left cardiac shunts, chronic lung disease, sleep apnea, or methemoglobinemia. On the other hand, if cyanosis is absent, search for other cardiopulmonary diseases, an underlying mass/tumor secreting erythropoietin autonomously (hepatocellular carcinoma, cerebellar hemangioblastoma, pheochromocytoma, parathyroid carcinoma, meningioma, uterine leiomyoma, and renal cell carcinoma), renal abnormalities (polycystic kidney disease and post-renal transplant), and endocrine disorders (Cushing's syndrome and primary aldosteronism) is warranted. Screening for doping (exogenous erythropoietin administration and androgen/anabolic steroids) is also required.1,2)
1) Relative/spurious polycythemia requires only hydration. Gaisbock syndrome is usually associated with obese, hypertensive, male smokers. Therefore, its recognition and correction of its cardiovascular risk factors by the primary care physician is of paramount importance.
2) Several causes of secondary polycythemia can be handled in primary care, and treatment strategies include smoking cessation, avoidance of high altitudes, doping control, and use of drugs that suppress the renal-angiotensin system in order to reverse post-renal transplant polycythaemia.
3) Other secondary etiologies are best treated by referring patients to other specialists, since elimination of the underlying cause (i.e., neoplasm, congenital heart disease, methemoglobinemia, etc.) usually results in disappearance of the polycythemia.
4) Primary polycythemias should always be referred to a hematologist, particularly in patients with a presumptive diagnosis of polycythemia vera, since confirmation of this diagnosis by molecular techniques (i.e., detection of JAK2V617F mutation) and prompt treatment with phlebotomies plus cytoreductive therapy (hydroxiurea) and aspirin in high-risk patients (age > 60 and previous history of thrombosis) is life-saving.
5) Polycythemic patients presenting with hyperviscosity symptoms (headache, mental clouding, blurred vision, and tinnitus) demand immediate referral to and evaluation by a hematologist, and prompt empirical phlebotomy treatment before determining the exact cause of polycythemia.
The GP considered that the patient's elevated hematocrit values could be due to ongoing diuretic therapy and dehydration from spending time in a warm location. She was advised to reinforce her hydration and return for review. In the follow-up visit at 1 month, blood parameters were normalized.
References
1. Kaushansky K, Lichtman MA, Beutler E, Kipps TJ, Seligsohn U, Prchal JT. Williams hematology. 2010. 8th ed. New York: McGraw-Hill.
2. Hoffman R, Benz EJ, Shattil SJ, Furie B, Cohen HJ, Silberstein LE, et al. Hematology: basic principles and practice. 2008. 5th ed. Edinburgh: Churchill Livingstone.
- TOOLS
-
METRICS

-
- 0 Crossref
- 1 Scopus
- 2,852 View
- 37 Download
- Related articles in KJFM
-
WomenŌĆÖs Health and Primary Care2024 January;45(1)
Management of Sarcopenia in Primary Care Settings2023 March;44(2)
Avascular Necrosis of the Hip in Primary Care2021 January;42(1)
Life Change Events of Adolescent Patients in Primary Care.1996 August;17(8)
Mass screening for glaucoma in primary care.1994 September;15(9)