INTRODUCTION
As the obese population increases, the incidence of metabolic syndrome is also increasing. There has been a recent report
1-4) on the relationship between the diagnostic criteria of metabolic syndrome or changes in the pulmonary function and cardiovascular mortality and total mortality. As such, there is increasing interest in changes in metabolic syndrome associated with changes in pulmonary function.
In a number of recent studies, it was reported that among the changes in pulmonary function, pulmonary function, deterioration is related to hypertension, type 2 diabetes, low-density lipoprotein cholesterol, overall obesity, abdominal obesity and insulin resistance.
5-9) Among the above listed factors, hypertension, diabetes, and abdominal obesity are included as diagnostic criteria for metabolic syndrome, hence it can be inferred that identifying the relationship between metabolic syndrome and pulmonary function deterioration is meaningful.
In a study on the relationship between pulmonary function deterioration and metabolic syndrome, pulmonary function deterioration was detected where there is metabolic syndrome. Even when gender, age, smoking status, alcohol drinking and physical activity factors were reflected, limited pulmonary function deterioration showed independent relevance to increased risk of metabolic syndrome.
8)
Obese people have shown signs of pulmonary function deterioration,
8-9) hence, a simple pulmonary function test during health examination can be used as a predictive factor for metabolic syndrome in obese people.
As such, this study will look into the relationship based on the changes in metabolic syndrome diagnostic criteria and pulmonary function indices, like forced expiratory volume for 1 second (FEV1), forced vital capacity (FVC), and FEV1/FVC ratio.
DISCUSSION
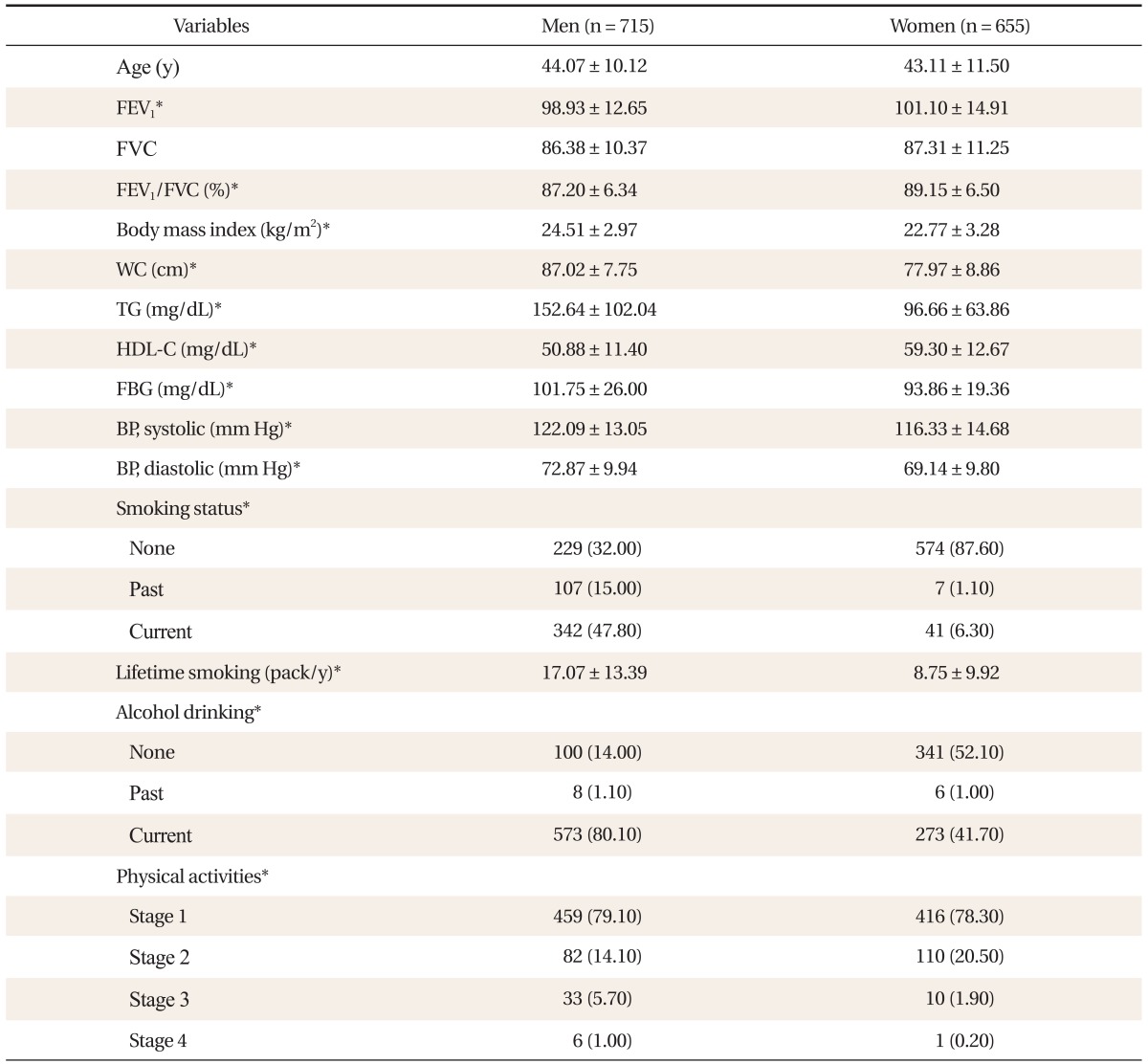
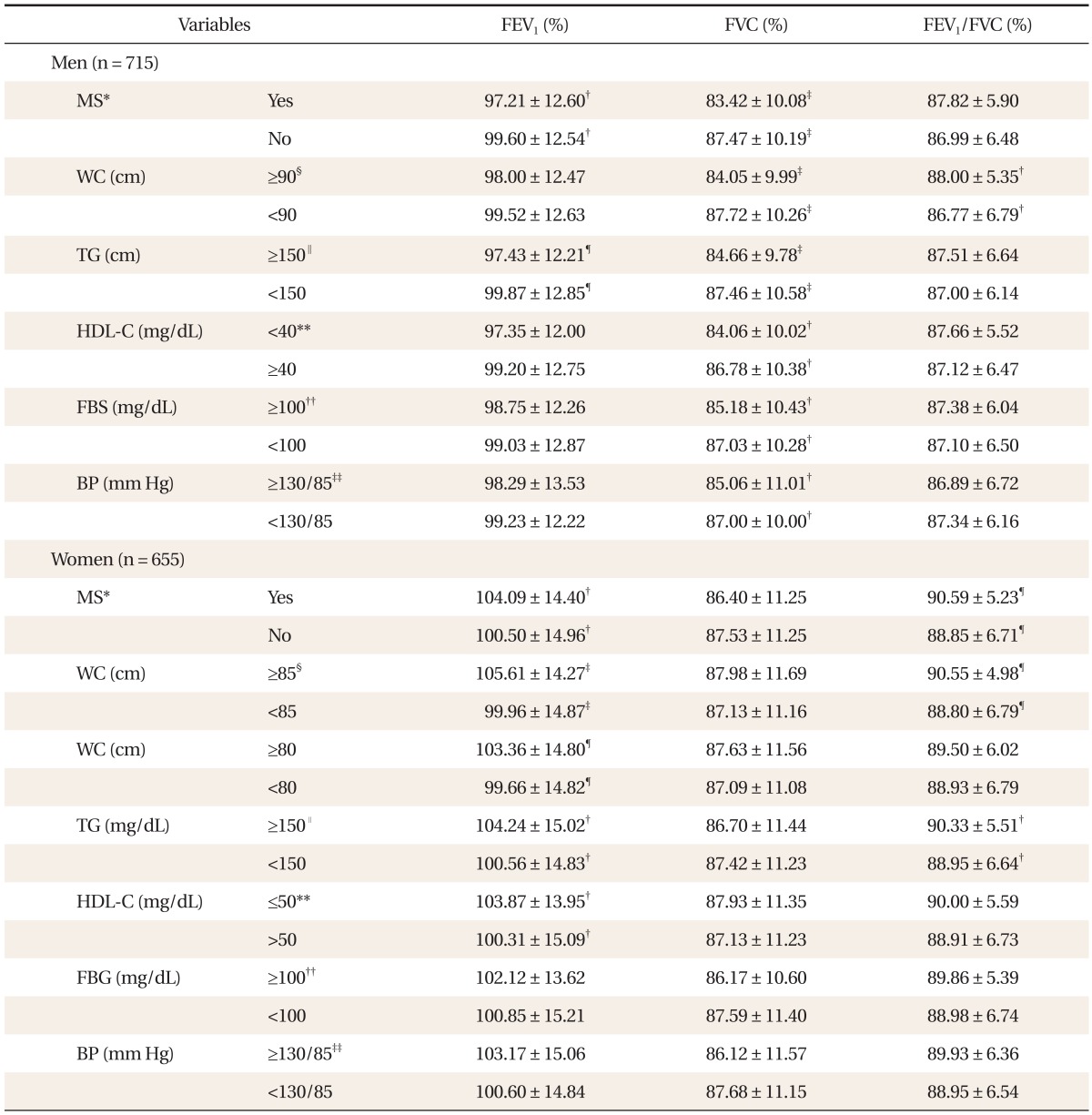
This study aimed to find relevance between components that serve as the criteria for diagnosing metabolic syndrome and poor performing pulmonary function. Among males, every diagnostic component of metabolic syndrome had significant correlation with poor pulmonary function. On the other hand, among females, FVC had a tendency of poor pulmonary function but with no significant relevance.
Many studies conclude that pulmonary function drops among obese people.
12,13) Previously, studies have used BMI, waist circumference, waist/hip circumference ratio, abdominal thickness (height) and skin thickness test as the markers that show obesity.
14-16) However, as of recent, studies focus on abdominal obesity as indicative of overall level of obesity. As such, this study tried to examine the waist circumference that demonstrates abdominal obesity as well as the relationship between metabolic syndrome components that are easily found among obese people and effects these factors have on pulmonary function.
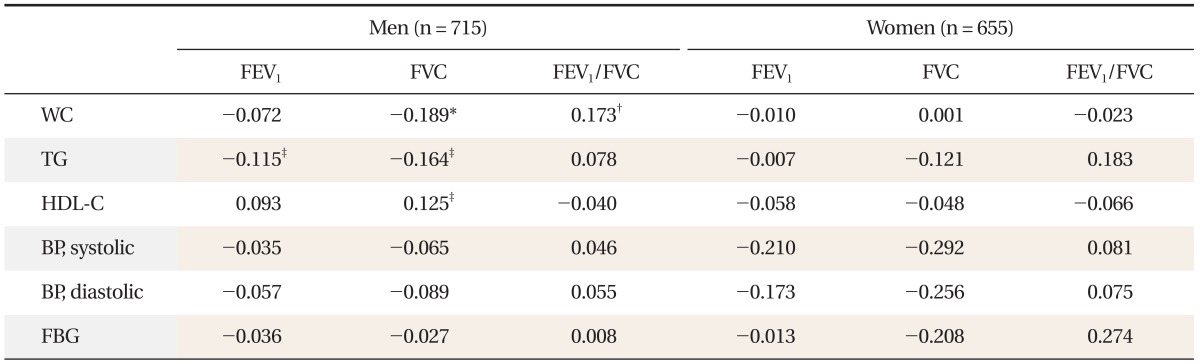
According to the study, reverse-correlation was found between diagnostic components of metabolic syndrome and pulmonary function. Among males, while there were significant differences in FVC according to whether or not there were any diagnostics components for metabolic syndrome, there were no FVC differences found among females. However, for both males and females, pulmonary function differed significantly according to waist circumference. For males, there was a significant statistical difference in FVC and FEV1/FVC. In the case of females, for waist circumference of 85 cm, both FEV1 and FEV1/FVC had a significant statistical difference, while waist circumference of 80 cm only showed a significant statistical difference in FEV1. In particular, among males, the partial correlation coefficient of waist circumference was FVC -0.189, FEV1/FVC 0.173.
According to a study conducted by Leone et al.,
17) both males and females showed reverse-correlation between all diagnostic components of metabolic syndrome and pulmonary function. As in this study, abdominal obesity was reported as the most powerful predictor of poor pulmonary function.
17) In addition, Chen et al.
18) found out that both males and females showed negative correlation between FEV
1/FVC and waist circumference even after age, height, weight, workload, energy consumption, and smoking were factored in. Thus, the bigger the waist circumference becomes, the greater its impact on pulmonary function, eventually having partial impact on the movements of diaphragm and chest.
18) Canoy et al.
16) took the waist/hip circumference ratio as the indicator of abdominal obesity to verify that both FEV
1 and FVC show reverse correlation both among males and females.
In Australia, Lazarus et al.
14) showed that FVC has negative correlation with males' waist circumference and that no relationship was found among females.
14) Moreover, according to a study conducted by Ochs-Balcom et al.,
19) males' FEV
1 and FVC showed negative correlation in all obesity markers (weight and level of obesity) as well as markers for abdominal obesity (waist circumference, ratio of waist/hip circumference, abdominal height). However, among females, only the abdominal height and waist circumference showed negative correlation with FEV
1, while all markers of obesity showed negative correlation with FVC. In particular, the reverse relationship between FEV
1 and abdominal height was evident only among those obese people with BMI of over 25 kg/m
2.
19)
According to this study, in men, correlation between waist circumference and FVC, FEV
1/FVC ratio was statistically significant in terms of partial correlation coefficient where age, height and total smoking amount was reflected. For women, the correlation was not statistically significant across all respiratory indexes. The results were similar to the research conducted by Harik-Khan et al.,
20) which showed that FVC and FEV
1 and waist circumference and hip circumference had negative correlation for men, whereas for women, only FVC had correlation and FEV
1 showed no correlation. To explain such differences by gender, it could be assumed that fat distribution could affect diaphragm and thoracic movements of women more than men and that waist circumference and hip circumference ratio does not affect pulmonary function.
20)
Carey et al.
21) said that changes in weight and obesity are related to FEV
1 and in particular, weight increase of the group with the highest obesity level showed greater FEV
1 reduction. Such results demonstrated a wider gap in men because male abdominal fat accumulated relatively more during the 7-year research period and in women, hip circumference tended to increase more. Thus, their increase in waist/hip circumference ratio was lower than men. Results of this study were also different by sex since males showed a higher level of obesity than women, with a higher ratio of men having abdominal fat.
Nakajima et al.
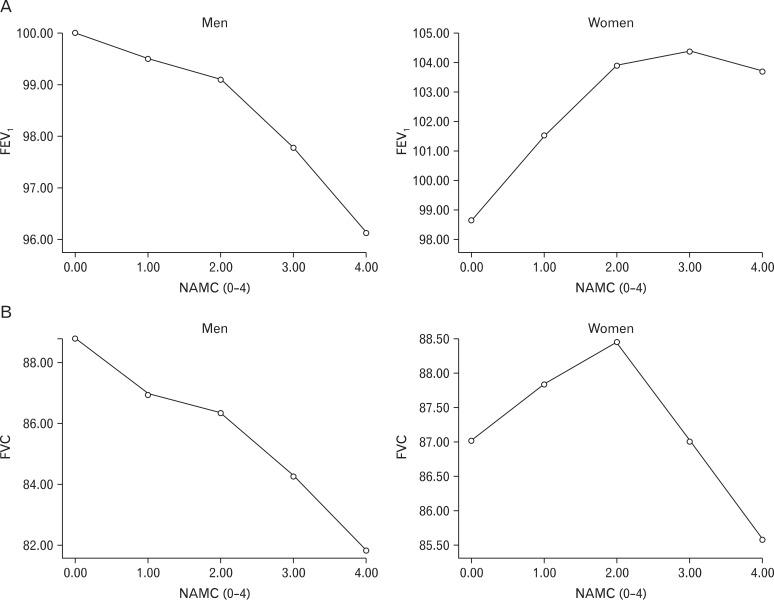
22) showed correlation between FVC and metabolic syndrome level, such as an increase in the sum of metabolic syndrome diagnostics factors. The research demonstrated that an increase in the severity of metabolic syndrome impairs lung function in men but not in women. The results indicate that in addition to the relationship between each metabolic syndrome factor and weaker pulmonary function, people with more metabolic syndrome factors are more vulnerable to pulmonary function impairment. Therefore, additional studies on how to control these metabolic factors to influence pulmonary function in metabolic patients is necessary.
Not much research has been conducted on the association between metabolic syndrome components and lung function impairment. Since such studies were almost non-existent in Korea, this research regarding pulmonary function impairment in Asians is very significant. It is also meaningful in showing the relationship between pulmonary function, metabolic syndrome, and sex, as such studies had never previously been performed.
However, given that the analysis was conducted on Koreans coming from a certain region and health examinees, it is hard to generalize the outcome of the research to all ethnic groups. Also, since women were not classified into groups before and after menopause, the results may not be statistically significant and should be validated further through additional research. The research had some constraints as a cross-sectional study with not many morbidly obese patients included in the analysis. Further research should be conducted, and in particular, studies on morbidly obese patients are also necessary.