|
 |
- Search
| Korean J Fam Med > Volume 34(6); 2013 > Article |
Abstract
Background
In this Study, we investigated the effects of lifestyle and metabolic syndrome on free oxygen radical levels in men and women in Korea.
Methods
A total of 254 adults were included in this study from February 2011 to June 2012 at a health promotion center. Information of the lifestyles and presence of metabolic syndrome factors was obtained. Biochemical markers were measured and free oxygen radicals test (FORT) was performed on the blood.
Results
Of the 254 subjects, 86 (33.9%) had metabolic syndrome, and 187 (73.6%) were men. Between the subjects with and without metabolic syndrome, there was a significant increase in alanine aminotransferase and serum FORT values in the subjects with metabolic syndrome. Multiple linear regression analysis showed that high-sensitivity C-reactive protein (hs-CRP) (P = 0.004), metabolic syndrome (P = 0.037), and female gender (P = 0.030) were independent predictors of serum FORT values. The subjects with high fasting blood sugar level or low high density lipoprotein cholesterol levels showed high serum FORT values.
The prevalence of metabolic syndrome has increased due to underactivity and overeating. The Korean National Health and Nutrition Examination Survey 2007-2010 reported that the prevalence rates of metabolic syndrome are 31.9% in Korean men and 25.6% in Korean women.1) Metabolic syndrome is associated with the development of cardiovascular disease, thus, the cardiovascular mortality in metabolic syndrome patients is 2 to 3 times higher than that of the general population.2,3) Oxidative stress, on the other hand, is an imbalance which occurs in the form of overproduced reactive oxygen or a shortage of antioxidants, and is associated with the development of metabolic syndrome.4)
Almost all metabolic syndrome patients suffer from abdominal obesity. An excessive accumulation of fat leads to enhanced production of oxidative stress. Increased oxidative stress in abdominal adipocytes may yield various pro-inflammatory adipocytokines and fatty acids.5) Thus, oxidative stress exacerbates metabolic syndrome factors such as insulin resistance, hypertriglyceridemia, decrement of high density lipoprotein (HDL) cholesterol, and hypertension.6-8)
However, there have been domestic studies on the relationship between oxidative stress and metabolic syndrome. Therefore, this study examined the relationship between factors of metabolic syndrome and oxidative stress in the Korean adult population. This study also examined whether metabolic syndrome makes a difference in oxidative stress values.
This study was performed in accordance with ethical and safety guidelines upon the approval of the institutional review board in The Catholic University of Korea St. Vincent's Hospital (VC12 RISI0080).
A total of 254 adults (control group 168 and metabolic syndrome group 86) participated in this study at a health promotion center located in Gyeonggi province, from February 2011 to June 2012.
This study used self-report questionnaires and interviews with healthcare providers to assess lifestyle, disease history, medication history, alcohol and smoking history, amount and frequency of exercise, eating habits, emotional stress, pollution exposure, and electromagnetic exposure.
Body weight and height was measured when standing barefoot, up to 0.1 kg and 0.1 cm, respectively. Waist circumference was measured in standing position, expiratory state. Waist circumference was measured on the middle area between the lower rib margin and the upper illiac bone margin.9) Blood pressure was measured using an automatic sphygmomanometer while sitting.
Blood samples were collected after at least 8 hours of fasting to examine the total amount of cholesterol, HDL, triglycerides, low density lipoprotein (LDL), high-sensitivity C-reactive protein (hs-CRP), insulin, total protein, albumin, aspartate transaminase, alanine transaminase (ALT), gamma-glutamyl transpeptidase, blood urea nitrogen, creatinine, uric acid, glycated hemoglobin, lipoprotein A, thyroid stimulating hormone, free T4, total number of white blood cells, hemoglobin, and hematocrit.
Free oxygen radicals (FORT) was evaluated by using the FORT test (FORM Plus; free oxygen radicals monitor, Callegri, Italy). Peripheral blood samples were collected from the tip of a finger and assessed to measure the FORT values by assessing hydrogen peroxide levels. Analyzed results were presented with FORT units. One FORT unit is equal to 0.26 mg/L H2O2. Reliability, reproduction and validity of FORT have been approved in many studies. In this way, the test has been used to analyze oxidative stress levels widely.10-12)
Metabolic syndrome as defined by the National Cholesterol Education Program,13) is characterized by at least three of the following: (1) Abdominal obesity, waist circumference ≥ 90 cm (in men), ≥ 85 cm (in women); (2) serum triglyceride ≥ 150 mg/dL (1.69 mmol/L); (3) serum HDL cholesterol < 40 mg/dL (1.04 mmol/L) (in men), < 50 mg/dL (1.29 mmol/L) (in women); (4) blood pressure ≥ 130/85 mm Hg or medication; (5) fasting plasma glucose ≥ 100 mg/dL (6.1 mmol/L) or medication. Abdominal obesity is defined by the reference, redefining obesity in Asia-Pacific.14)
Data were analyzed by using the SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Analysis of variance and t-test were used to examine the relationships between FORT and lifestyle, eating habits and presence of disease of the subjects. Pearson's correlation analyses were used to examine the relationships between biochemical markers and FORT. Multiple linear regression analysis was used to analyze the effects of various independent variables on the FORT. P-values were considered statistically significant if they were less than 0.05.
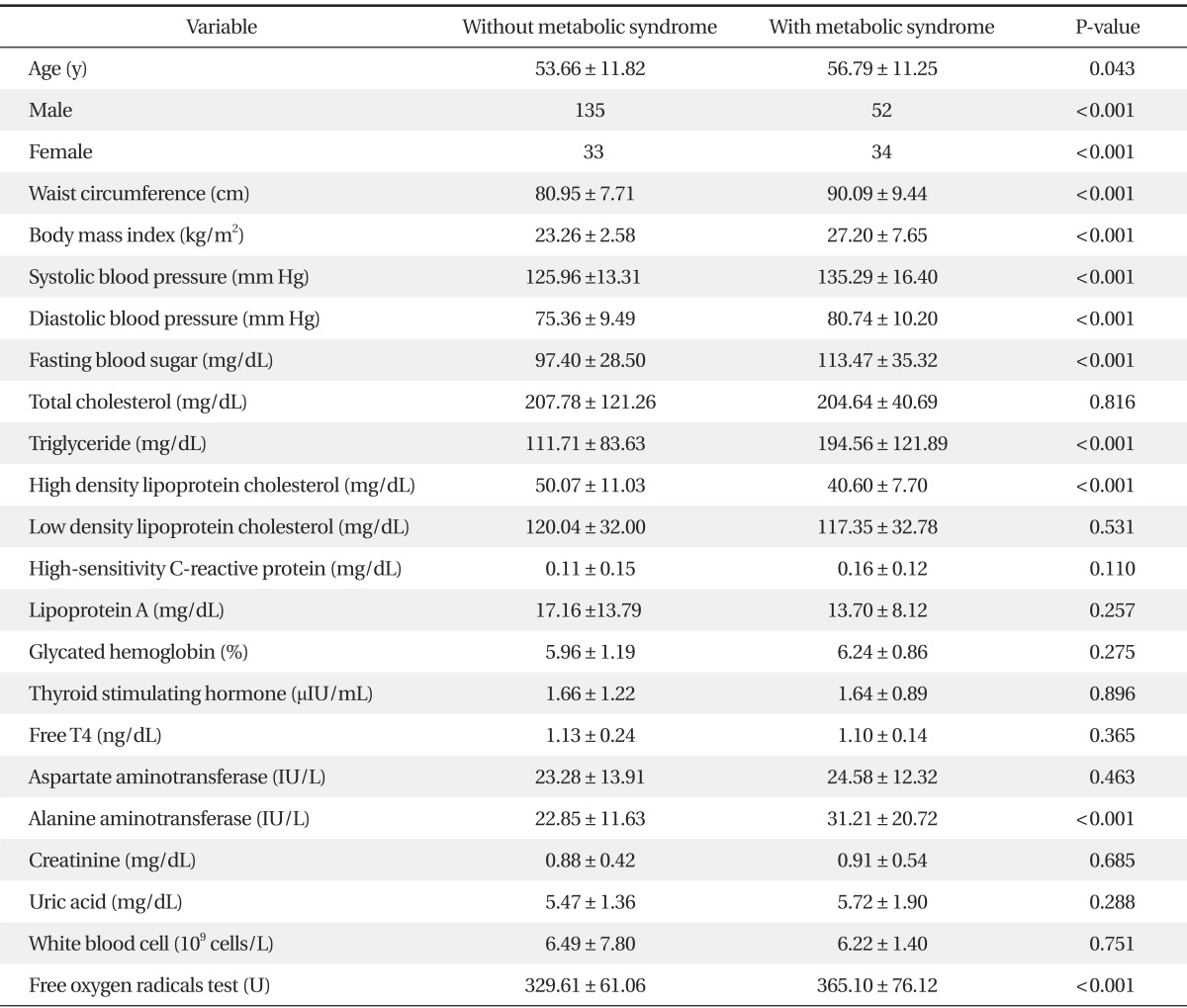
The total number of subjects was 254. There were 86 metabolic syndrome patients (33.9%) and 168 healthy controls (66.1%). There were 187 males (73.6%). ALT levels were significantly higher in the metabolic syndrome group (P < 0.05), however there was no significant difference in other factors between the metabolic syndrome group and the control group, except metabolic syndrome diagnosis factors.
The FORT values were 365.10 ± 76.12 FORT units in the metabolic syndrome group, and 329.61 ± 61.06 FORT units in the control group. A significantly higher FORT value was shown in the metabolic syndrome group (P < 0.001) (Table 1).
The FORT values in the non-smoking group were 357.72 ± 74.92 FORT units, in the past smoking group were 327.46 ± 61.36 FORT units, and in the present smoking group were 327.24 ± 59.77 FORT units. A significantly higher FORT value was shown in the past smoking group (P = 0.002). The FORT value in the group that consumed alcohol no more than once a month was significantly higher than the FORT value in the group consuming alcohol once or more a month (P = 0.003). Males showed a significantly higher FORT value than females (P < 0.001). However, the FORT values showed no significant difference when compared with other exogenous factors such as pollution exposure, sun exposure, amount and frequency of exercise, electromagnetic exposure, emotional stress, or eating habits (Table 2).
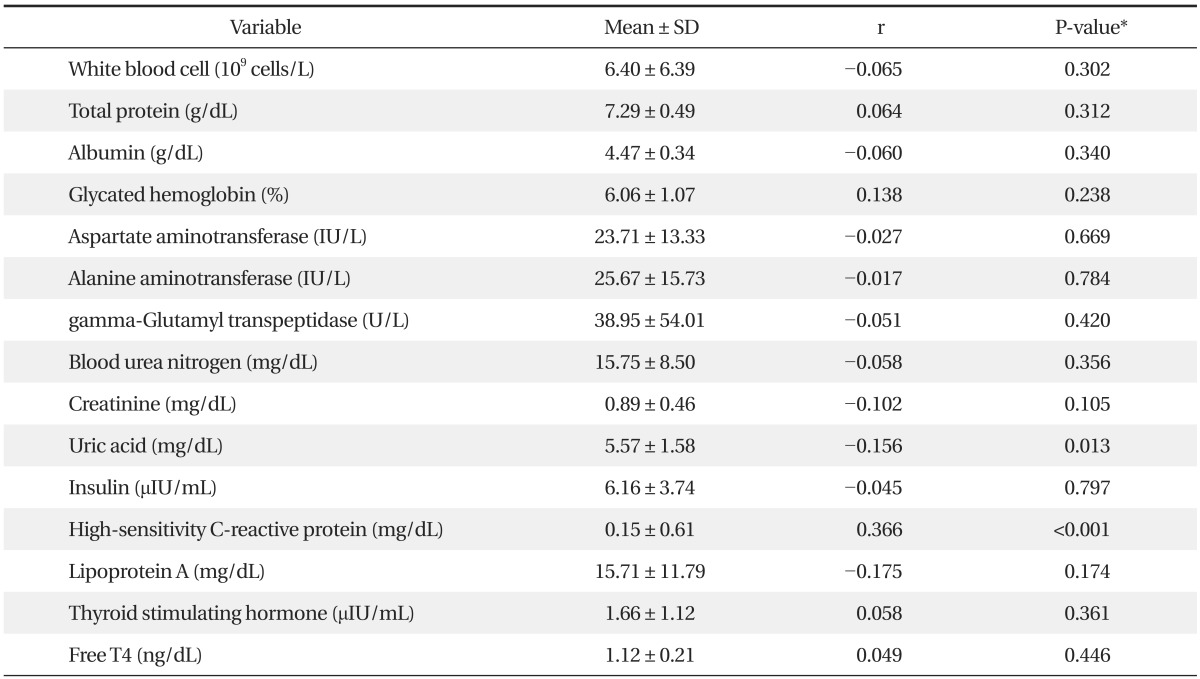
The FORT value showed a positive correlation with hs-CRP (P < 0.001). In contrast, the FORT value showed a negative correlation with uric acid (P = 0.013). No other biochemical markers showed a statistically significant relationship with the FORT values (Table 3).
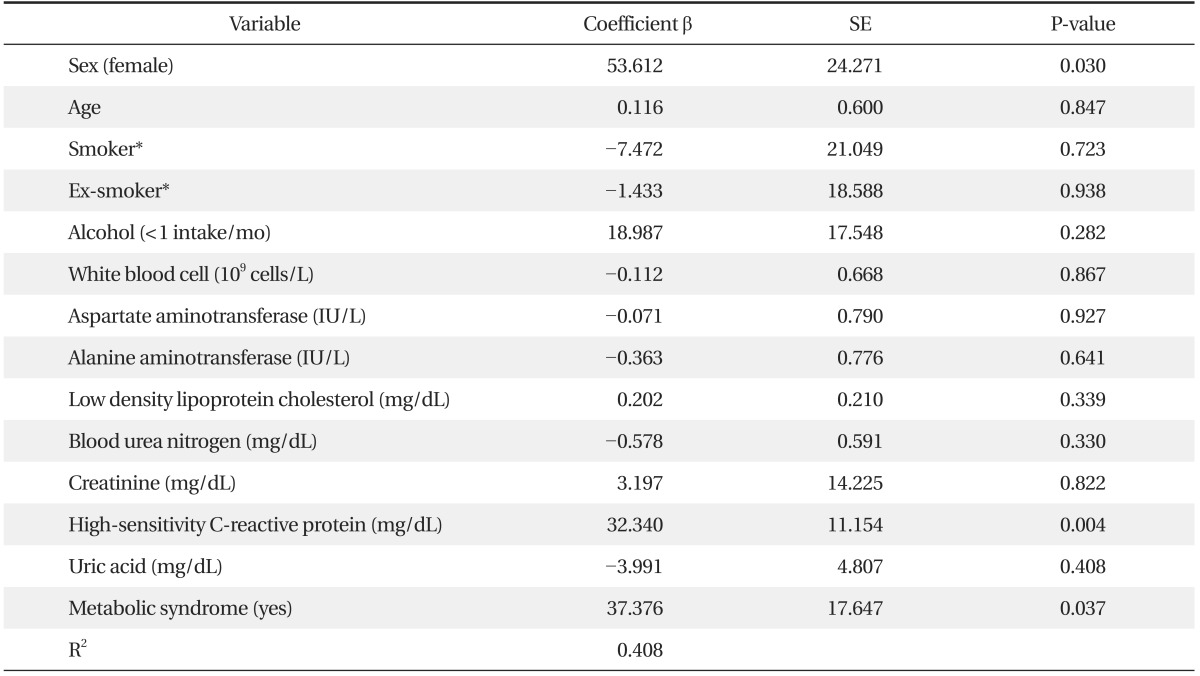
Multiple linear regression analysis was performed to analyze the effects of statistically significant variables between the metabolic syndrome group and the control group in univariate analysis. The analysis showed hs-CRP (P = 0.004), metabolic syndrome (P = 0.037), and gender (P = 0.030) were an independent predictor of FORT values (Table 4).
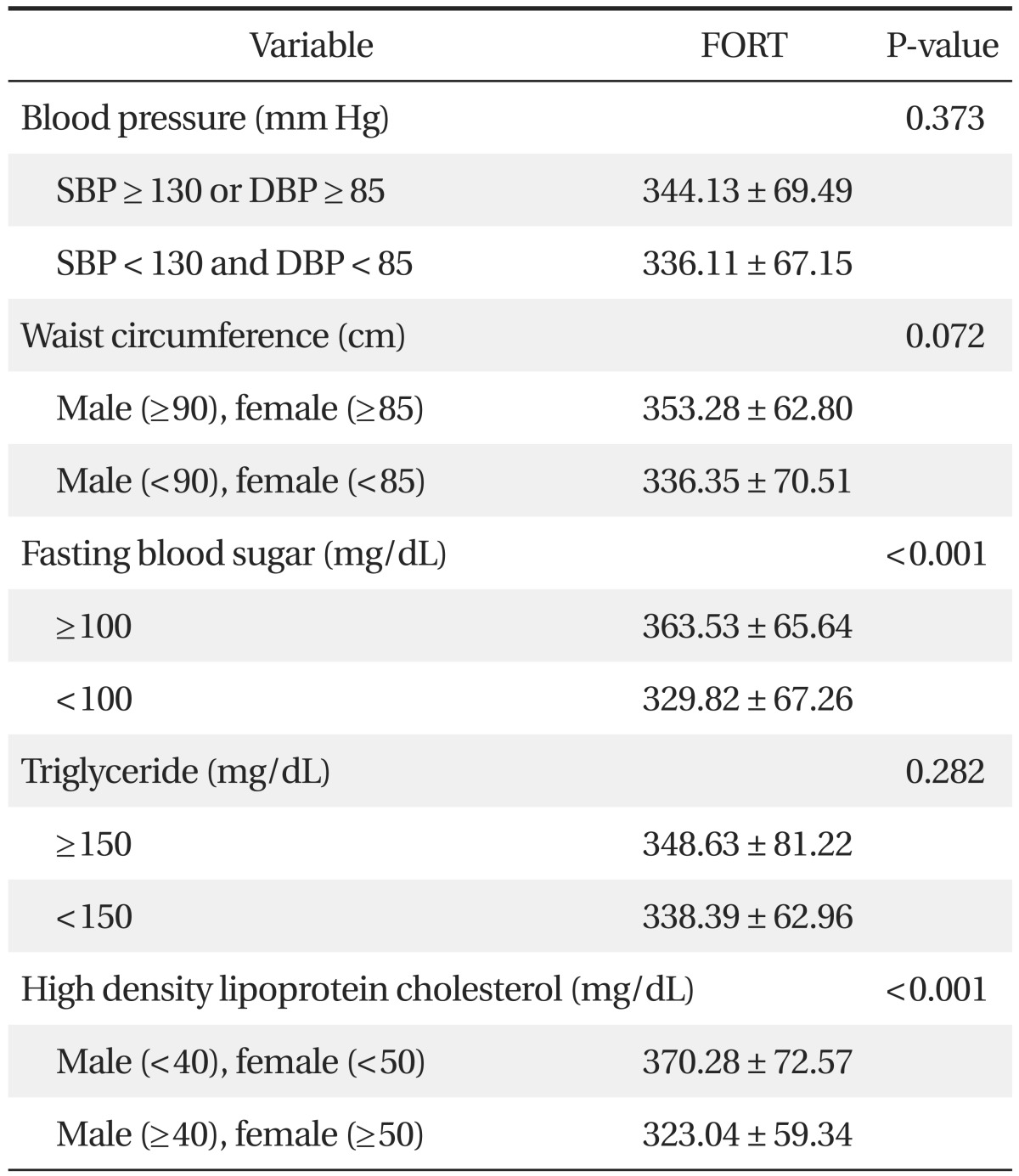
The FORT values in the subjects who had higher fasting plasma glucose or lower HDL cholesterol were significantly higher (P < 0.001). However, according to blood pressure level, waist circumference, and triglyceride level, there were no significant differences in the FORT value (Table 5).
Oxidative stress damages DNA and proteins by inducing oxidation reactions, contributing to aging, atherosclerosis, autoimmune disease, Parkinson's disease, Alzheimer's dementia, cancer, and cardiovascular disease. Overproduction and reduction of antioxidant capacity is determined by various lifestyle factors, especially non-smoking, vitamin and mineral supplements, fruit eating, and regular exercise. Male gender and aging showed negative correlations with antioxidant capacity.15)
In this study, the FORT values were significantly higher in the non-smoking group, non-drinking group, and females. The FORT value showed positive correlation with hs-CRP, and showed negative correlation with uric acid. Multiple linear regression analysis was performed to analyze the effects of these statistically significant variables. As a result, alcohol, smoking, and uric acid showed no significant effects. In contrast, female gender, higher hs-CRP, and metabolic syndrome showed significant relationships with higher FORT values.
However, when other variables were controlled through regression analysis, there was no significant relationship between smoking habits with FORT. Other studies such as Lorgis et al.16) and Lee et al.17) reported similar results. But Moller et al.18) reported smoking was associated with higher oxidative stress, Vassalle et al.19) reported females and smokers showed a significant relationship with increment of oxidative stress. In addition, Lesgards et al.15) reported that non-smokers showed a positive relationship with antioxidant capacity.
Since tobacco has many oxidating agents such as nicotine, FORT and other oxidating agents, it can contribute to atherosclerosis.20) However, many studies reported varied results. Thus, additional studies are necessary to test the relationship under control.
The FORT values showed a positive correlation with hs-CRP (P ≤ 0.001). In contrast, they showed a negative correlation with uric acid (P = 0.013). However, other biochemical markers showed no significant relationship with the FORT values. Only hs-CRP was truly related to the FORT value when the analyses of the effects of various independent variables on the FORT values were examined. Hs-CRP is an inflammatory marker and it has been examined in many studies. It has been considered as a potential marker of risk of cardiovascular disease.21,22)
Other studies reported oxidative stress as an oxidative stress marker,23-25) and Lee et al.17) reported that hs-CRP exhibited a positive correlation with the FORT value. Many other studies reported a relationship between hs-CRP and oxidative stress under controlled environments, thus, utilization of hs-CRP as an oxidative stress predictable factor could be taken into consideration. Fujita et al.26) reported that systemic oxidative stress, as measured by urinary 8-epi-PGF2, is strongly associated with visceral fat accumulation and metabolic syndrome. Kotani and Taniguchi27) reported that subjects with metabolic syndrome (n = 37) exhibited significantly higher reactive oxygen metabolites levels than those without metabolic syndrome (n = 37) in Japanese males aged under 60 years. Jialal et al.28) reported that nascent metabolic syndrome was associated with increased oxidative stress as demonstrated by both circulating and cellular biomarkers, which could contribute to the risk for both diabetes and cardiovascular disease. Similarly, in this study, metabolic syndrome patients exhibited significantly higher FORT values under controlled environments. In particular, higher fasting plasma glucose and higher LDL cholesterol levels exhibited significant relationships with the FORT values. Reactive oxygen species regenerate endogenous antioxidants, interrupt glucose absorption in muscles and fat cells, decrease the secretion of insulin in beta cells, and increase insulin resistance and fasting plasma glucose levels.29) Atherosclerosis and cardiomyopathy in type 2 diabetes are caused by insulin resistance.30) In addition, low HDL cholesterol levels are an important risk factor for cardiovascular disease. HDL cholesterol has many cardiovascular protection effects, such as anti-inflammatory effects, anti-oxidant capacity, anti-coagulation, and anti-thrombotic capacity.31)
Almost all females answered that they were non-smokers in self-reporting questionnaires. However, there was a report that only 7.1% of female subjects reported they are smokers but actually 13.9% of female subjects were proven to be smokers by examination of nicotine in their urine.32) According to this, self-reporting questionnaires on smoking habits have low reliability. Therefore, collection of urine to check nicotine levels or examination of expiratory CO2 levels is one possible solution.
Second, in women, oxidative stress can be altered by menopausal state. However, this study had too few female subjects to analyze the effects of menopausal state on the FORT value. Additional large-scale studies should be conducted to examine the relationship between oxidative stress and menopausal state in Korean women.
In this study, women, individuals who had high levels of hs-CRP, and metabolic syndrome patients exhibited higher oxidative stress. There have been few domestic studies on metabolic syndrome and oxidative stress in Korea. This study provides evidence that metabolic patients have higher oxidative stress than healthy individuals. Additional prospective intervention studies should be conducted to examine whether cured metabolic syndrome patients show reduction of the FORT values.
References
1. Korea Centers for Disease Control and Prevention. Korean National Health and Nutrition Examination Survey 2007-2010. Cheongwon: Korea Centers for Disease Control and Prevention; 2012.
2. Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001;24:683-689. PMID: 11315831.


3. Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002;288:2709-2716. PMID: 12460094.


4. Ando K, Fujita T. Metabolic syndrome and oxidative stress. Free Radic Biol Med 2009;47:213-218. PMID: 19409982.


5. Onat A. Metabolic syndrome: nature, therapeutic solutions and options. Expert Opin Pharmacother 2011;12:1887-1900. PMID: 21756201.


6. Vincent HK, Taylor AG. Biomarkers and potential mechanisms of obesity-induced oxidant stress in humans. Int J Obes (Lond) 2006;30:400-418. PMID: 16302012.


7. Fujita T. Aldosterone in salt-sensitive hypertension and metabolic syndrome. J Mol Med (Berl) 2008;86:729-734. PMID: 18437332.


8. Funder JW. Is aldosterone bad for the heart? Trends Endocrinol Metab 2004;15:139-142. PMID: 15109610.


9. Obesity: preventing and managing the global epidemic: report of a WHO consultation. World Health Organ Tech Rep Ser 2000;894:i-xii. 1-253. PMID: 11234459.

10. Pavlatou MG, Papastamataki M, Apostolakou F, Papassotiriou I, Tentolouris N. FORT and FORD: two simple and rapid assays in the evaluation of oxidative stress in patients with type 2 diabetes mellitus. Metabolism 2009;58:1657-1662. PMID: 19604518.


11. Abramson JL, Hooper WC, Jones DP, Ashfaq S, Rhodes SD, Weintraub WS, et al. Association between novel oxidative stress markers and C-reactive protein among adults without clinical coronary heart disease. Atherosclerosis 2005;178:115-121. PMID: 15585208.


12. Mantovani G, Madeddu C, Maccio A, Gramignano G, Lusso MR, Massa E, et al. Cancer-related anorexia/cachexia syndrome and oxidative stress: an innovative approach beyond current treatment. Cancer Epidemiol Biomarkers Prev 2004;13:1651-1659. PMID: 15466983.



13. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement: executive summary. Crit Pathw Cardiol 2005;4:198-203. PMID: 18340209.


14. International Obesity Taskforce. Asia-Pacific regional obesity guidelines. Sydney: International Association for the Study of Obesity; 1999.
15. Lesgards JF, Durand P, Lassarre M, Stocker P, Lesgards G, Lanteaume A, et al. Assessment of lifestyle effects on the overall antioxidant capacity of healthy subjects. Environ Health Perspect 2002;110:479-486. PMID: 12003751.



16. Lorgis L, Zeller M, Dentan G, Sicard P, Richard C, Buffet P, et al. The free oxygen radicals test (FORT) to assess circulating oxidative stress in patients with acute myocardial infarction. Atherosclerosis 2010;213:616-621. PMID: 20947086.


17. Lee YA, Kang SG, Kim SH, Park SJ, Kim HN, Song IS, et al. Assessment of lifestyle effects on the levels of free oxygen radicals in the Korean population. Korean J Fam Med 2012;33:296-304. PMID: 23115704.



18. Møller P, Wallin H, Knudsen LE. Oxidative stress associated with exercise, psychological stress and life-style factors. Chem Biol Interact 1996;102:17-36. PMID: 8827060.


19. Vassalle C, Novembrino C, Maffei S, Sciarrino R, De Giuseppe R, Vigna L, et al. Determinants of oxidative stress related to gender: relevance of age and smoking habit. Clin Chem Lab Med 2011;49:1509-1513. PMID: 21679134.


20. Yamaguchi Y, Matsuno S, Kagota S, Haginaka J, Kunitomo M. Oxidants in cigarette smoke extract modify low-density lipoprotein in the plasma and facilitate atherogenesis in the aorta of Watanabe heritable hyperlipidemic rabbits. Atherosclerosis 2001;156:109-117. PMID: 11369003.


21. Ridker PM, Brown NJ, Vaughan DE, Harrison DG, Mehta JL. Established and emerging plasma biomarkers in the prediction of first atherothrombotic events. Circulation 2004;109(25 Suppl 1):IV6-IV19. PMID: 15226246.


22. Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 2003;107:363-369. PMID: 12551853.


23. Dohi Y, Takase H, Sato K, Ueda R. Association among C-reactive protein, oxidative stress, and traditional risk factors in healthy Japanese subjects. Int J Cardiol 2007;115:63-66. PMID: 16759717.


24. Hirose H, Kawabe H, Komiya N, Saito I. Relations between serum reactive oxygen metabolites (ROMs) and various inflammatory and metabolic parameters in a Japanese population. J Atheroscler Thromb 2009;16:77-82. PMID: 19403985.


25. Sakano N, Wang DH, Takahashi N, Wang B, Sauriasari R, Kanbara S, et al. Oxidative stress biomarkers and lifestyles in Japanese healthy people. J Clin Biochem Nutr 2009;44:185-195. PMID: 19308273.



26. Fujita K, Nishizawa H, Funahashi T, Shimomura I, Shimabukuro M. Systemic oxidative stress is associated with visceral fat accumulation and the metabolic syndrome. Circ J 2006;70:1437-1442. PMID: 17062967.


27. Kotani K, Taniguchi N. The association between reactive oxygen metabolites and metabolic syndrome in asymptomatic Japanese men. J Clin Med Res 2011;3:247-251. PMID: 22383912.



28. Jialal I, Devaraj S, Adams-Huet B, Chen X, Kaur H. Increased cellular and circulating biomarkers of oxidative stress in nascent metabolic syndrome. J Clin Endocrinol Metab 2012;97:E1844-E1850. PMID: 22872691.


29. Maddux BA, See W, Lawrence JC Jr, Goldfine AL, Goldfine ID, Evans JL. Protection against oxidative stress-induced insulin resistance in rat L6 muscle cells by mircomolar concentrations of alpha-lipoic acid. Diabetes 2001;50:404-410. PMID: 11272154.


30. Giacco F, Brownlee M. Oxidative stress and diabetic complications. Circ Res 2010;107:1058-1070. PMID: 21030723.



31. Chung IM. HDL cholesterol and cardiovascular disease. Cardiovasc Update 2004;6:19-24.
32. Kim HJ. Quarter of Korean adult women smoke. YTN 2011;11 16.
Table 2
Relationship between gender and exogenous factors of the subjects and levels of reactive oxygen species measured by the FORT

Table 3
Relationship between biological factors of the subjects and reactive oxygen species levels measured by the free oxygen radicals test
- TOOLS