INTRODUCTION
Coronavirus disease 2019 (COVID-19) has been spreading rapidly across China and other countries since the end of 2019 and has become a pandemic. Globally, 85,091,012 confirmed cases of COVID-19, of which 1,861,005 died, were reported by the World Health Organization (WHO) [1]. Malaysia, a developing country with a population of 30 million people, is also affected by the COVID-19 pandemic and is at an increased risk since it is one of the most popular travel destinations worldwide and the center of a business hub. As of February 2021, a total of 245,552 cases were reported in Malaysia, with 896 deaths related to COVID-19 [2]. Aggressive public health and containment measures were instituted, drawing from the experience of handling the severe acute respiratory distress syndrome epidemic and the influenza (H1N1) pandemic several years ago.
Malaysia reported the first case of COVID-19 on January 25, 2020, an individual who had traveled from Wuhan, China [3]. In the middle of March 2020, a sudden surge in COVID-19 cases occurred in a state in the west coast of Peninsular Malaysia following a religious gathering. It then spread throughout the country, including a state in the east coast, Terengganu. The first case of COVID-19 in this state was reported in Besut, a semi-rural district, and the number of positive COVID-19 cases detected across the state increased rapidly over the next few weeks. Following the outbreak, the Movement Control Order (MCO) was enforced by the Malaysian Safety Council on March 18, 2020, which promulgated restriction on movement and activities throughout the country under the Malaysian Prevention and Control of Infectious Diseases Act 1988 and the 1967 Police Act. The following measures were implemented under the MCO: (1) prohibition of mass movements and religious, sports, social, and cultural activities; (2) closure of business premises except those providing daily necessities and necessary services; (3) self-quarantine and health check measures for those returning from abroad; (4) restrictions on tourists and visitors; (5) closure of schools, kindergartens, and higher institutions of learning; and (6) closure of all government and private premises except those providing essential services such as water, electricity, and telecommunication. Full lockdown was imposed in red zones with a high incidence of infections (≥40 cases) [4]. Such measures slowed the rate of local infections and reduced the number of deaths throughout the country from May 2020 to July 2020 until such time that only one new case was reported per day. Unfortunately, the third wave of COVID-19 infections occurred in September 2020, which caused a surge in cases due to mass gatherings and breaches in standard operating procedures (SOPs) during an election in one of the states in Malaysia.
BRIEF OVERVIEW OF THE MALAYSIAN PRIMARY HEALTHCARE SYSTEM
Public health, including primary care, plays a major role in the early containment of COVID-19 infections, active case detection, surveillance, public education, monitoring, and prevention of transmission to prevent the worsening of the outbreak and impact of the disease.
The primary healthcare system in Malaysia comprises a combination of 2,900 public and 7,000 private facilities involved in service provision. The public sector has an extensive network of health clinics that are scattered according to their geographical areas, community clinics in rural areas, and mobile clinics in remote areas [5]. Terengganu is one of the states in Peninsular Malaysia, and consists of eight districts with 51 primary health clinics under the management of the respective district health office supervised by family physicians. These health clinics bring healthcare closer to people’s homes and workplaces and are the first to provide continuing healthcare service.
EARLY CONTAINMENT MEASURES BY PRIMARY HEALTH CLINICS
1. Screening Protocol
Patient screening at the clinic entrance is a new strategy. Since the space in the health clinic is limited, two canopies were placed outside the clinic as a waiting area for patients undergoing screening and case assessment, which also served as an isolation area for COVID-19 testing. A health declaration form was filled out at the screening area, and body temperature was measured using an infrared thermometer. Patients were examined on an appointment basis. Non-urgent and stable cases were provided another appointment to avoid overcrowding in the clinic. Urgent or acute cases were immediately assessed in the emergency room.
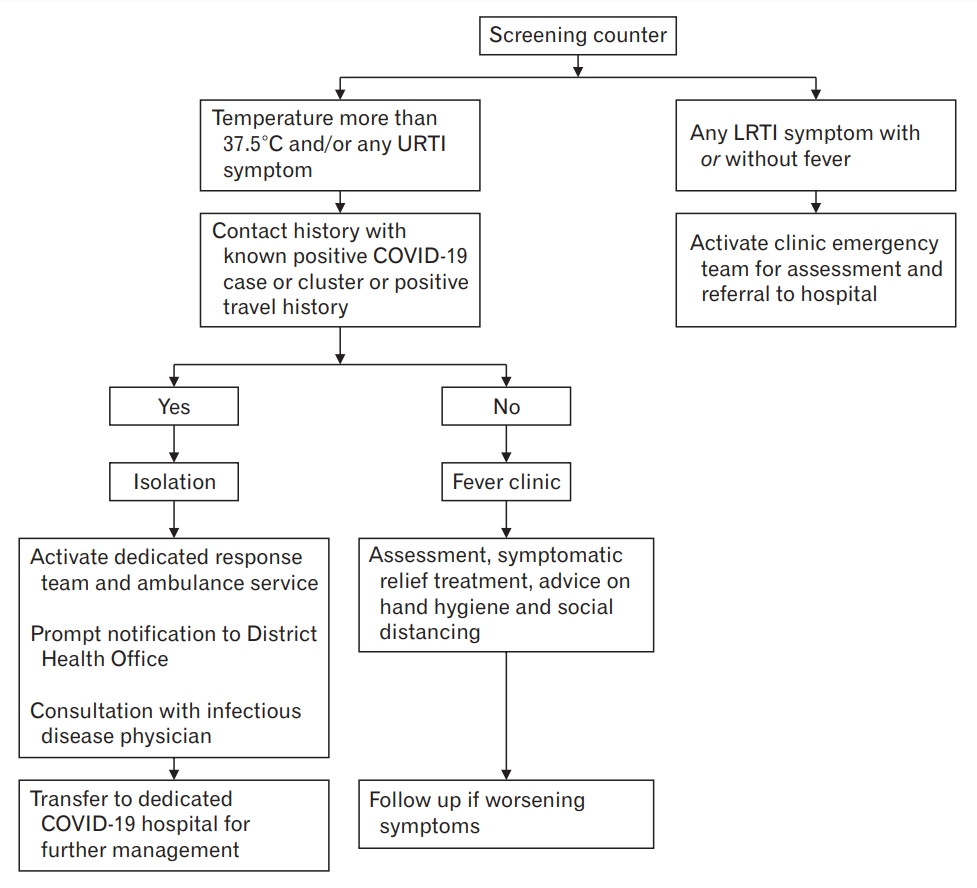
Those with temperatures higher than 37.5°C or any symptoms of upper respiratory tract infection were evaluated at a fever clinic located near the screening area where the patients were reassessed for COVID-19 and examined. Those at low risk for COVID-19 infection were managed accordingly (Figure 1). All patients were required to wear a facemask at all times, sanitize their hands frequently, and enforce physical distancing of at least 1 meter between each patient. Although a high volume of patients was reviewed each day, only 30 patients were allowed to stay inside the clinic area at any time.
2. Isolation Area for COVID-19 Testing
The isolation area was located about 3 meters away from the main clinic entrance to reduce patient movement, thereby reducing unnecessary exposure to other patients and healthcare workers (HCWs). The HCWs involved in the sampling were a medical officer, an assistant medical officer, and a medical laboratory worker. All of them were adequately trained and wore full personal protective equipment (PPE) in accordance with the infection control protocol.
3. High-Risk COVID-19 Case Management
Patients at high risk for COVID-19, those who were in close contact with an individual who tested positive for COVID-19, or those who had travelled from a high-risk area were directed to the isolation area for further assessment and sampling, after which a notification was promptly sent to the district health office. Patients who fulfilled the case definition of COVID-19 were transferred to a dedicated COVID-19 hospital, while those with suspected infections or who had close contact with an individual who tested positive for COVID-19 were quarantined in specialized quarantine centers. Patients with lower respiratory tract infections were managed in the emergency room. If the patient was diagnosed with severe acute respiratory tract infection, the patient was admitted to either a district or general hospital depending on the severity (Figure 1).
INFECTION CONTROL MEASURES
1. Healthcare Workers’ Education and Practice
Besides the containment measures mentioned earlier, educating the HCWs on information and infection control procedures was also crucial [6]. These measures included wearing a surgical facemask, eye protection (either goggles or a face shield), long-sleeved medical gown, and disposable gloves. A physical distance of 1 meter at minimum was maintained, and frequent hand washing was practiced [6]. In the isolation area where patients with suspected COVID-19 cases or previous close contact were managed, wearing an N95 mask, isolation gown, plastic apron, gloves, eye protection (either goggles or a face shield), head cover, and boot or shoe covers was required [7]. These PPEs were worn as per regulations to ensure the safety of the HCWs and avoid COVID-19 transmission in our center.
2. Role of the Infection Control Unit
The infection control team at our clinic consists of a family medicine specialist, chief medical officer, chief nurse, and assistant medical officer. This team monitors and ensures that the infection control protocol is followed by all HCWs. An infection control audit was also conducted regularly by the district team in part to ensure an adequate supply of PPEs for HCWs. Meetings were held regularly to update information and discuss any issues arising at the clinic.
3. Patient Education
Improving knowledge of patients and the community plays an important role to reduce the transmission of COVID-19 infection. Most patients in the community had a low literacy level and poor socioeconomic status. Therefore, educating them to adapt to the new clinic system and new norms in the long run are extremely challenging. Continuous health education regarding COVID-19 was provided via awareness talks, educational videos, pamphlets, banners, and information sheets. This was also implemented in the ‘Orang Asli’ community who live in remote areas. In line with modern technology, we also used our official social media page as a medium to provide education and correct any misconceptions or wrong information being disseminated through the Internet. With these efforts, we believe that we have effectively reduced the rate of COVID-19 infection and transmission among HCWs and patients in our center, although no specific data supporting this claim are available.
DELIVERING SERVICES IN THE NEW NORM
1. Use of Telemedicine and Staggered Appointment
To ensure continuous delivery of healthcare services, we practiced telemedicine, which involved telephone consultations and use of chatting applications for selected cases, for example, reviewing the blood sugar profile of a diabetic patient, monitoring the blood pressure of a hypertensive patient from their home, and reviewing the patients’ investigation results. Telemedicine is defined as the delivery of healthcare services using information communication technology when distance is a critical factor [8]. The clinic systems were also improved by using a staggered appointment system and triaging cases at the main entrance. This not only prevents overcrowding in the clinic, but also develops the patients’ self-empowerment. Although the implementation was quite challenging and the outcome could not be assessed instantly, we received positive feedback from patients after its implementation. This system was perceived as time saving and improved health awareness among patients and caregivers.
2. “Drive-Through” Pharmacy
The pharmacy unit has developed some strategies to cope with the COVID-19 crisis as a part of pandemic preparedness, which includes “drive-through” pharmacy. This service improves access to medication while ensuring that preventive measures recommended by the WHO are followed [9]. In the “drive-through pharmacy,” the patient pre-ordered the medications via telephone and receives them at the “drive-through” window. The medicine is pre-checked, labeled, packed in advance, and then dispensed without having the patients exit their vehicle. This new medication dispensing system has been shown to reduce waiting time and unnecessary exposure in the clinic. An effective two-way communication between the pharmacist and patient was key to its success. Medication compliance was also assessed over the phone, which further improved the patient’s awareness and empowerment towards their health.
ROLE OF PSYCHOLOGICAL FIRST AID DURING THE PANDEMIC
Some HCWs were physically and mentally exhausted while responding to the outbreak. Various conflicts occurred during the initial phase of the pandemic. The fear of contracting the infection and transmitting the virus to their loved ones in addition to the increased work burden undeniably affected the mental health of HCWs. Therefore, the State Health Department implemented an initiative to screen all HCWs involved in the COVID-19 pandemic to determine their mental health status and arranged psychological first aid (PFA) sessions not only for the HCWs but also for quarantined persons under investigation.
PFA forms part of the Mental Health and Psychological Support Program initiated by the Ministry of Health (MOH) Malaysia that provides any type of local or external support to protect or promote psychosocial well-being as well as prevent and treat mental disorders. Support may include health interventions, education, counseling, and community-based activities. An online questionnaire (the Depression Anxiety Stress Scales questionnaire) was filled out by the participants to screen for depression, anxiety, and stress. The responses were then reviewed by the state PFA team. Those with moderate to severe depression, anxiety, or stress were scheduled for further counseling sessions with the PFA team, which consisted of a family medicine specialist, a trained medical officer, an occupational therapist, and a psychiatrist via telephone. The DASS screening was then repeated after 2 weeks; a significant improvement in the patients’ DASS scores and emotional well-being was observed. None of the participants were diagnosed with psychiatric disorders. PFA also effectively supported the HCW emotionally to allow them to continue fighting against the pandemic while maintaining good mental health.
CHALLENGES: TECHNOLOGY LITERACY, HUMAN RESOURCE, AND FINANCIAL CONSTRAIN
1. Technology Literacy, Training, and Education Issues
The MOH Malaysia continuously monitors and updates the public regarding the status of the pandemic. COVID-19 information is constantly delivered to all divisions of the Malaysian healthcare system. The guidelines for COVID-19 management were provided in detail by the MOH to increase the country’s level of preparedness. Various webinars, courses, and clinical discussions were conducted to update the knowledge of the HCWs via Webex, Zoom, and Facebook.
The MOH provided sufficient up-to-date information with regard to public education through three major platforms: the official portal of the MOH, Facebook pages called the Crisis Preparedness and Response Center (CRPC) and Kementerian Kesihatan Malaysia (KKM), and the CRPC and KKM pages on Telegram. The MOH has also conducted daily press briefings and conferences, and published relevant news regarding the status of the COVID-19 pandemic to increase public engagement, ensure public awareness, and provide access to accurate information [10]. This has helped overcome the spread of false information and rumors through the Internet.
2. Human Resource
Human resources and financial budgets were among the major challenges faced at the height of COVID-19 pandemic. The Malaysian government has put in a lot of effort to overcome these problems. In addition to providing a sufficient number of additional HCWs via contractual bases in all public health facilities throughout the country, a group effort was made by public and private hospitals to accommodate the growing numbers of COVID-19 cases, including the involvement of university hospitals and hospitals affiliated with the Ministry of Defence [10]. In addition, HCWs from all over the country were recruited, and allocated to other states with a high burden of cases, thus accommodating the need for services in quarantine centers.
3. Financial Constraints
RM 20.0 billion (USD 4.56 billion) financial stimulus package was announced by the Malaysian government to mitigate the impact of COVID-19 based on three major strategies: (1) lessening the effect of COVID-19, (2) ensuring people-based economic growth, and (3) encouraging quality investments. A special fund known as the COVID-19 Fund was also set up, in which the money collected was channeled to patients, particularly those affected financially due to the quarantine procedure to cover medical expenses. NGOs and individuals were also welcomed to direct their contributions accordingly [10]. The MOH and the National Electricity Company established an action coalition to obtain financial aid from corporate companies, government-linked companies, and various organizations in Malaysia to fight the outbreak. The collected funds were used to procure medical supplies and other necessary healthcare equipment. Several NGOs, public figures, prison inmates, and volunteers also helped to prepare the PPE for medical frontliners to overcome the shortage of PPE [10].
CONCLUSION
Health clinics play an important role in the implementation of public health containment measures and management of COVID-19 in the community. Adaptation with the new clinical systems, implementation of infection control measures within a small facility, delivery of educational awareness to the rural community, shortage of human resources, and financial constraints were among the challenges. However, the primary care roles in facing this pandemic were enhanced by the tremendous support from higher government authorities, non-government organizations, and collaborative networks with the private sector, as well as the HCWs’ commitment. This experience is expected to be a reference source and will inspire other healthcare systems to overcome the challenges during the COVID-19 pandemic.