|
 |
- Search
| Korean J Fam Med > Volume 44(4); 2023 > Article |
|
Abstract
Herein, we report a rare case of Tolosa-Hunt syndrome (THS) following coronavirus disease 2019 (COVID-19) vaccine administration. A 64-year-old patient presented with recurrent horizontal diplopia and ipsilateral orbital pain, 2 weeks after being administered the COVID-19 vaccination. A diagnosis of THS was based on the relevant criteria after ruling out the differential diagnoses. The clinical presentation improved with corticosteroid administration. THS must be recognized as a complication of COVID-19 vaccination. This association can be explained by an autoimmune response.
Tolosa-Hunt Syndrome (THS) is one of the several neuro-ophthalmological complications described after coronavirus disease 2019 (COVID-19) vaccine administration [1]. It is a rare disease characterized by severe and unilateral periorbital headache and painful restriction of eye movements [1,2]. Furthermore, it is often associated with the granulomatous inflammation of the cavernous sinus [3]. Herein, we have reported the second ever case of THS following COVID-19 vaccination.
A 64-year-old patient was hospitalized in January 2015 for painful diplopia which completely resolved with corticosteroid therapy. In August of the same year, long-term aspirin administration was initiated for a transient ischemic vascular accident. Fifteen days before the current episode, he had received the third dose of the COVID-19 vaccine, with nucleoside-modified messenger RNA encoding the viral spike glycoprotein of severe acute respiratory syndrome coronavirus 2.
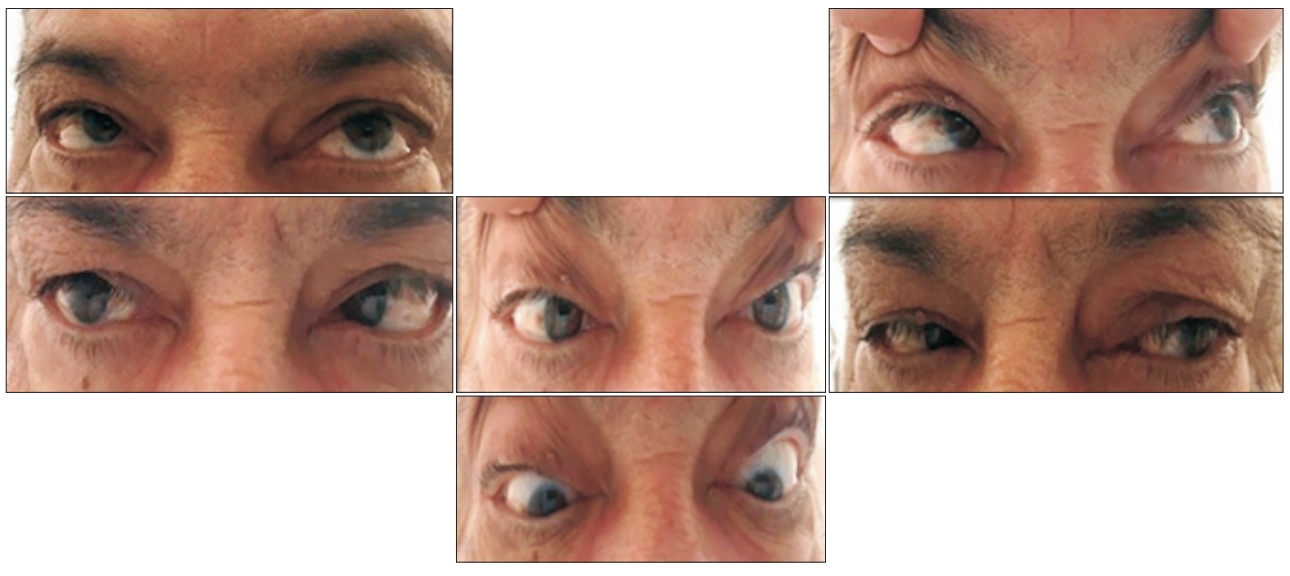
He presented with binocular diplopia which was preceded by recurrent unilateral retro-orbital pain. Ocular mobility examination confirmed horizontal diplopia with a more pronounced limitation of abduction in the right side (Figure 1). Informed consent was obtained from the patient before his hospitalization.
Ophthalmological examination revealed preserved visual acuity, symmetrical pupillary reflex, and a normal fundus. A neurological examination revealed right trigeminal neuralgia and facial paresis. The cardiovascular examination findings were unremarkable. Complete blood count, erythrocyte sedimentation rate, and C-reactive protein levels were normal. His fasting blood sugar level was 5.6 mmol/L and glycated hemoglobin level was 6.7%.
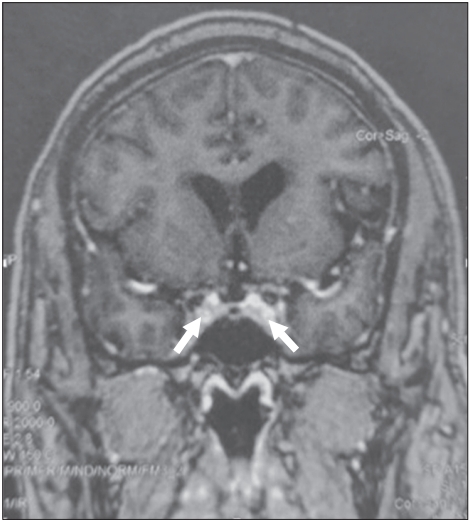
Cerebral magnetic resonance imaging (MRI) did not reveal an intracranial expansive process, intracranial hypertension, and hemorrhagic or ischemic lesions. However, it revealed an enhancement in the cavernous sinus, suggesting either a granulomatous lesion or a THS (Figure 2). Sarcoidosis was ruled out owing to the absence of characteristic clinical and paraclinical signs. Infectious origin was ruled out, based on the negative serological tests for herpes simplex virus, cytomegalovirus, syphilis, human immunodeficiency virus, and West Nile virus. Cerebrospinal fluid composition was normal.
In view of the isolated painful right lateral rectus palsy, recurrence of symptoms, cerebral MRI findings, and the absence of any other etiology, a diagnosis of THS was made. Corticosteroid therapy was initiated with 1 g of intravenous methylprednisolone for 3 days. Thereafter, 1 mg/kg/d of oral methylprednisolone was administered for 2 months. His pain completely resolved within the first week of treatment, and the abduction in both eyes had significantly improved by 1 month (Figure 3). Corticosteroid therapy was gradually tapered. At the last examination, 3 months after corticosteroid therapy discontinuation, normal ocular mobility was observed.
The individual provided written informed consent for the publication of the clinical data and images.
THS was first described by Tolosa [2], in 1954 as recurrent painful ophthalmoplegia caused by granulomatous inflammation of the cavernous sinus. The diagnostic criteria established by Hunt were recently revised by the International Classification of Headache Disorders [4]. In the third edition in 2018, THS was associated with unilateral orbital or frontal headaches preceded by or concomitantly observed with lateral paresis of one or more oculomotor nerves (III, IV, and/or VI) and MRIor biopsy-confirmed granulomatous inflammation of the cavernous sinus without a recognized etiology [2,4]. Our patient met all the revised criteria with a normal workup. Therefore, several differential diagnoses, including carotid-cavernous fistula, carotid dissection, aneurysm, primary cavernous sinus thrombosis, lymphoma, infection, vasculitis, and sarcoidosis, had to be ruled out [5,6]. MRI brain is crucial for the diagnosis because it shows an enlarged cavernous sinus or convex lateral wall [2], which were seen in our patient. THS is a non-specific, chronic, granulomatous inflammation of the septa and wall of the cavernous sinus, which is characterized by lymphocytic and plasmacytic infiltration to a variable extent into the superior orbital fissure or/and orbital apex, causing pressure upon the penetrating nerves [2]. Although the physiopathology remains unknown, traumatic injury, tumors, and aneurysms are plausible etiologies [2,7]. Recently, the COVID-19 vaccination was identified to induce THS [5] and has been implicated in various THS-associated autoimmune phenomena [5] such as systemic lupus erythematous and Wegener’s granulomatosis [2]. To the best of our knowledge, this is the second case to be reported after COVID-19 vaccination. Hajjar al. [7] reported a case of post-COVID-19 infection THS. Recently, THS was reported 23 days after COVID-19 vaccination and 14 days after COVID-19 infection. The patient presented with multiple neurological symptoms such as ischemic stroke, meningitis, infectious vasculitis, and hemorrhagic encephalitis [8]. The authors questioned whether it was an adverse reaction to the vaccine or an associated infection. The response appears to have a dual mechanism: COVID-19– related immune dysregulation and its association with an infectious disease.
THS can spontaneously regress [5]. High-dose glucocorticoids, which also serve as a therapeutic test by the rapid resolution of orbital pain, is used to treat THS [2,6,7]. This was improvement was seen in our patient. Immunosuppressants should be added to the treatment regimen for children with recurrent THS [6].
In conclusion, THS is a non-specific granulomatous inflammation of the cavernous sinus which can occur as an autoimmune response after COVID-19 infection or vaccination. THS should be recognized by physicians and may present as painful ophthalmoplegia and unilateral headaches. Although it quickly respond to corticosteroids, it can also frequently recur.
Figure. 1.
Images showing limited abduction in both eyes. Written informed consent for the publication of this image was obtained from the patient.
REFERENCES
1. Lotan I, Lydston M, Levy M. Neuro-ophthalmological complications of the COVID-19 vaccines: a systematic review. J Neuroophthalmol 2022;42:154-62.


2. Amrutkar C, Burton EV. Tolosa-Hunt syndrome. Treasure Island (FL): StatPearls Publishing; 2023.
3. Dutta P, Anand K. Tolosa-Hunt syndrome: a review of diagnostic criteria and unresolved issues. J Curr Ophthalmol 2021;33:104-11.



4. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018;38:1-211.


5. Chuang TY, Burda K, Teklemariam E, Athar K. Tolosa-Hunt syndrome presenting after COVID-19 vaccination. Cureus 2021;13:e16791.