Effects of Brief Advice from Family Physicians on the Readiness to Change of Korean Male At-risk Drinkers
Article information
Abstract
Background
This study examined the effects of the method of delivery of brief advice on the readiness to change in at-risk drinkers.
Methods
The participants were 103 at-risk male drinkers who visited Chungnam National University Hospital for general health examinations. Baseline data on drinking behavior, readiness to change drinking behavior, and sociodemographic characteristics were obtained from a questionnaire. Family physicians gave two minutes of advice by telephone or in-person. The brief advice comprised a simple statement that the patient's drinking exceeded the recommended limits and could lead to alcohol-related problems. It also included advice to moderate one's drinking. One month later, the readiness to change was assessed again by telephone. The improvement in the readiness to change according to each method of delivery was investigated.
Results
Initially, among the 58-patient in-person advice group, 12 patients were in the precontemplation stage, 38 in the contemplation stage, and 8 in the action stage. One month after the advice was given to the patients, the distribution had changed significantly (P < 0.001) to 1, 21, and 36 patients, respectively. Among the 45-patient telephone advice group, 7 patients were in the precontemplation stage, 32 patients were in the contemplation stage, and 6 patients were in the action stage before the advice. The distribution had changed significantly (P < 0.001) to 1, 17, and 27 patients, respectively, 1 month after the advice.
Conclusion
These results suggest that brief advice by family physicians is effective in improving the readiness to change of at-risk drinkers, regardless of the delivery method.
INTRODUCTION
The word "motive" originates from "movere," a Latin word referring to "move." In a psychological context, motive means the fundamental power that leads a person to move and refers to a tendency or attitude determining the direction of a subject's behavior.1) Motive is the driving force that leads to changes in behavior. Motivation is the process by which a subject moves toward a goal. Motivation plays an important role in inducing patients with alcohol-related problems to change their behavior and maintain the change. According to De Leon et al.,2) enhancing motivation is an important element in caring for patients with problems related to alcohol, as well as abuse of other substances. Cox and Klinger3) also perceived the patients' level of motivation as a fundamental component in caring for patients with such problems.
Brief intervention has been used to motivate at-risk drinkers and enforce their willingness to undergo treatment. Fleming4) explained that there are three forms of brief interventions that can be applied according to the patient's drinking level: simple advice, regular counseling, and intensive intervention requiring 15 to 20 minutes. In terms of effectiveness, he also mentioned that the effect of brief outpatient counseling is not inferior to that of an intensive alcohol treatment program.
It has been indicated that a brief educational program on drinking can improve an at-risk drinker's readiness to change.5) Brief intervention is also an effective tool in improving problems related to drinking.6,7) However, the medical circumstances of Korea may limit the ability of physicians to perform such time-consuming interventions in their office. Another possible problem is that primary care physicians may lack the confidence and training to deal with drinking-related problems. Hence, if shorter, simpler advice was offered by a majority of physicians, the motivational state of a patient to change their drinking behavior could be improved. Such methods would be valuable in primary care practice.
Brown et al.8) suggested brief interventions by telephone as a method of treating patients. Counseling by telephone is an intervention method used to induce changes in a patient's behavior and is utilized to correct problematic habits, including smoking, improper meals, and deficient exercise. Various studies9,10) have reported the excellent effect of telephone intervention, which is not inferior to that of personal counseling. However, no studies have reported the effect of telephone counseling on improving problems related to drinking in Korea.
Problem drinking includes at-risk drinking, alcohol abuse, and alcohol dependence. The present study was conducted on patients identified as at-risk drinkers to investigate whether simple advice from family physicians could improve a patient's readiness to change their drinking behavior. Furthermore, this study investigated the effect of telephone advice on a patient's readiness to change in comparison with that of in-person advice.
METHODS
1. Subjects
This study was conducted on 103 male at-risk drinkers who visited a health promotion center in a university hospital in Daejeon from June to September of 2009. All subjects agreed to participate in the research. In this study, patients who drank 14 standard drinks (7 standard drinks for those ≥ 65 years old) in 1 week or 5 standard drinks (4 standard drinks for those ≥ 65 years old) in 1 day, considering 14 g of alcohol as a standard drink, were defined as at-risk drinkers, according to the recommendation of the National Institute on Alcohol Abuse and Alcoholism.11) During the research period, 162 patients were identified as at-risk drinkers. Among them, 59 patients did not complete the follow-up telephone interview because of contact failures or non-responses to the questionnaire.
2. Data Collection
The patients' basic information was collected using a questionnaire and from their medical records. The initial questionnaires were sent to the patients before visiting the health promotion center and were collected on the day of the visit. The initial questionnaire contained questions regarding intention to participate in the research, drinking frequency, and average and maximum number of drinks in one day. It also included questions on spouse, occupation, religion, economic state, and academic level. The state of a patient's motivation to drink was investigated using a readiness-to-change questionnaire. To investigate the factors that influenced the readiness to change of a patient, five questions from the family APGAR and questions from the Brief Encounter Psychosocial Instrument into Korean (BEPSI-K) were included to evaluate and measure family function and stress level.
3. Brief Advice on Drinking
One week after the initial visit, patients were given simple two-minute advice by family physicians during the review of the results of the health check-up. The brief advice comprised a simple statement that the patient's drinking exceeded the recommended limits and could lead to alcohol-related problems. In addition, it included a statement recommending that the patient moderate their drinking. Feedback based on the results of the health check-up was given. The brief advice was performed in-person (n = 58) or by telephone (n = 45). One month later, the score of a patient's readiness to change was examined again by telephone.
4. Questionnaires Used in the Study
1) Readiness to change questionnaire
The Readiness to Change Questionnaire was suggested by Heather et al.12) to evaluate the readiness to change of a patient with drinking problems. Reflecting the transtheoretical model developed by Diclemente and Prochaska,13) the questionnaire classifies the state of readiness to change in a patient with drinking problems into precontemplation, contemplation, and action stages. The questionnaire can be used easily in the primary care setting. The questionnaire includes 12 questions in total, including those regarding precontemplation (1, 5, 10, and 12), contemplation (3, 4, 8, and 9) and action (2, 6, 7, and 11) stages. According to the research carried out by Rollnick et al.,14) Cronbach's alpha reliability coefficient was 0.73 for the questions regarding precontemplation, 0.80 for contemplation, and 0.85 for action. Kim15) translated the questionnaire into Korean and reported that the Cronbach's alpha of the Korean version was 0.6 for the questions regarding precontemplation, 0.7 for contemplation, and 0.64 for action. The present study used the Korean version as translated by Kim.15)
2) Family APGAR questionnaire
Smilkstein16) developed a questionnaire to evaluate family function. This questionnaire comprises five questions on the family's adaptability, partnership, growth, affection, and resolve. It measures the level of personal satisfaction in the interrelationships among family members. The total score is 10 points. Zero to 3 points indicate "severe family dysfunction," 4 to 6 indicate "moderate family dysfunction," and 7 to 10 indicate "healthy family function." The reliability and validity of the questionnaire in Korea has been reported.17)
3) Brief encounter psychosocial instrument
Frank and Zyzanski18) developed the Brief Encounter Psychosocial Instrument (BEPSI) questionnaire to measure the degree of stress. In 1992, Bae et al.19) translated the five questions of the BEPSI-K. Yim et al.20) suggested a score of < 1.3 points as "low stress," 1.3 to 2.39 as "moderate stress," and ≥ 2.4 as "severe stress," and reported its reliability and validity. The questionnaire reflects external demand, internal demand, differences in external and internal demand, uncertainty of demand, and combinations of demands. The questionnaire reportedly had strong correlations with previous methods of measuring levels of stress, anxiety, depression, and life changes. The level of stress in this study was classified according to the suggestions of Yim et al.20)
5. Data Analysis
The patients were divided into in-person advice and telephone advice groups. To compare the demographic characteristics of the two groups, a chi-square test and independent t-test were performed for nominal and continuous variables, respectively. The changes in the distributions of patients in terms of readiness to change one month after the advice were evaluated by the McNemar test. Drinking behavior before and one month after the advice was given was compared using paired t-tests. The differences in the changes in drinking behavior between the two groups were compared using an independent t-test. To investigate the effect of the method of advice on the improvement in readiness to change, a multiple logistic regression analysis was performed with adjustment for covariates such as patient age, whether living with a spouse, occupational state, religious state, monthly income, residency, family function score, stress score, and drinks per week. SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis, and statistical significance was accepted at values of P < 0.05.
RESULTS
1. Characteristics of the Research Subjects
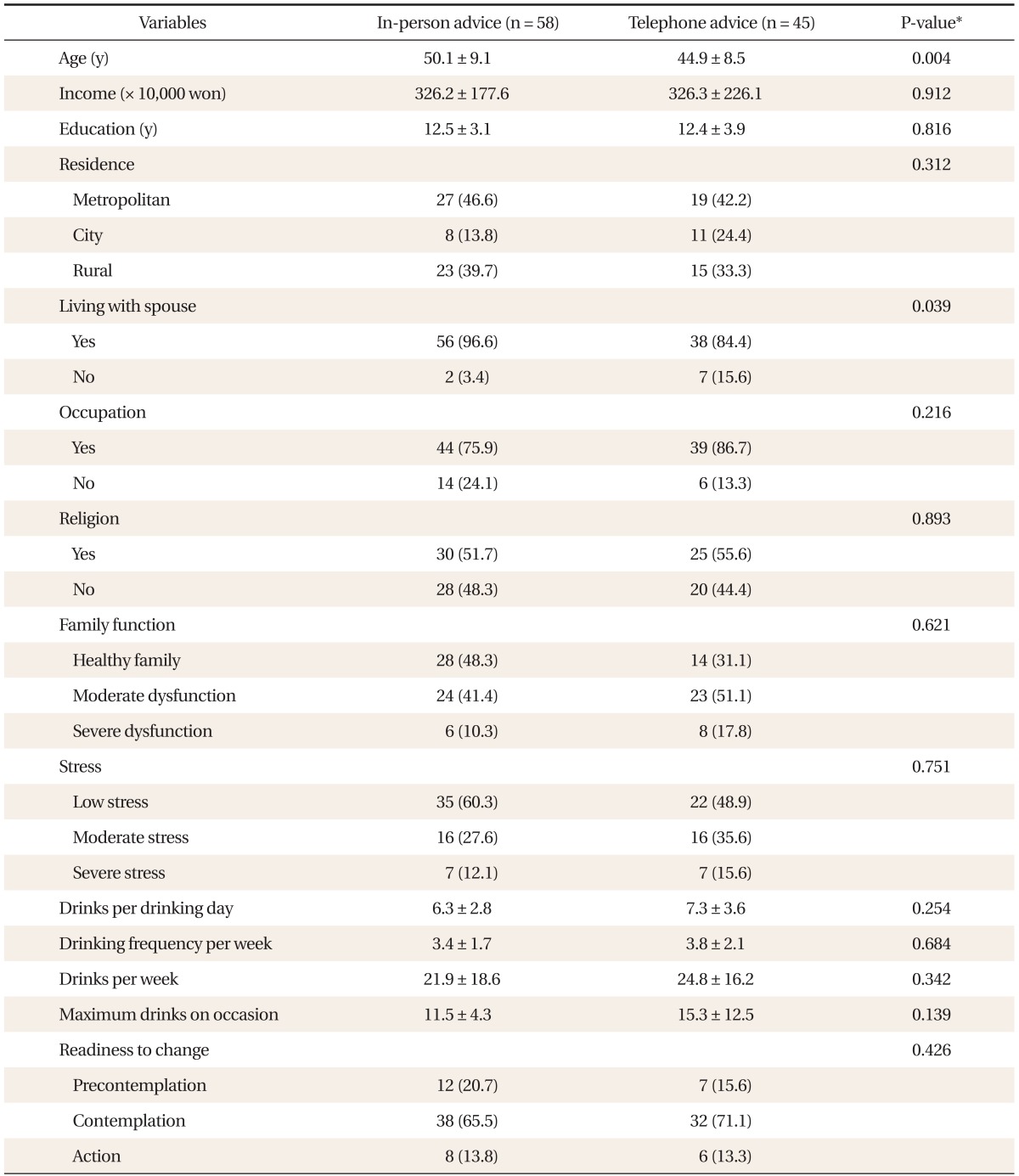
The mean ± SD age of the 58 patients in the in-person advice group was 50.1 ± 9.1 years, while that of the 45 patients in the telephone advice group was 44.9 ± 8.5 years. The mean age of the in-person advice group was significantly (P = 0.004) greater than that of the telephone advice group. Two patients (3.4%) in the in-person advice group, were not living with a spouse, compared to 7 (15.6%) in the telephone advice group this difference was significant (P = 0.039). There were no significant differences in monthly income, academic level, residential area, occupational state, religious state, family function score, or stress score between the two groups. There were no significant differences in drinking-related characteristics such as mean and maximum number of drinks in one day, number of drinking days per week, and drinks per week between the two groups. The initial distributions of readiness to change were not significantly different between the two groups (Table 1).
2. Changes in Readiness to Change One Month after Brief Advice
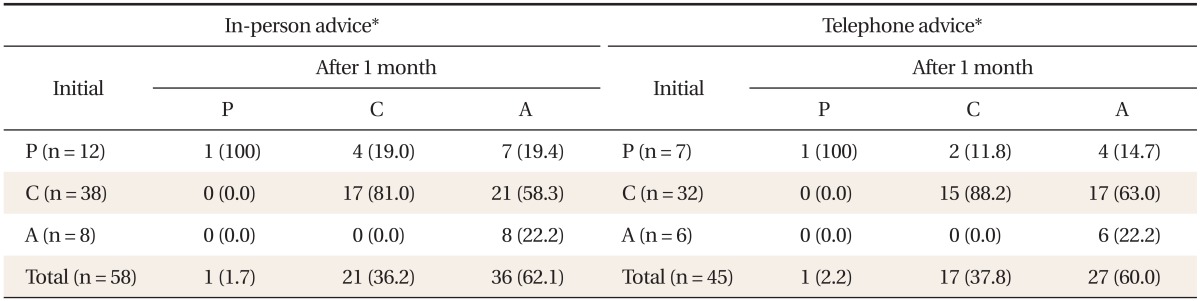
Initially, among the 58 in-person advice patients, 12 (20.7%) were in the precontemplation stage, 38 (65.5%) in the contemplation stage, and 8 (13.8%) in the action stage. One month after advice was given, the distribution had changed significantly (P < 0.001) to 1 (1.7%), 21 (36.2%), and 36 (62.1%), respectively. Regarding the 45 telephone advice patients, 7 (15.6%) were in the precontemplation stage, 32 (71.1%) in the contemplation stage, and 6 (13.3%) in the action stage before the advice. The distribution of patients changed significantly (P < 0.001) to 1 (2.2%), 17 (37.8%), and 27 (60.0%), respectively, 1 month after the advice was given (Table 2).
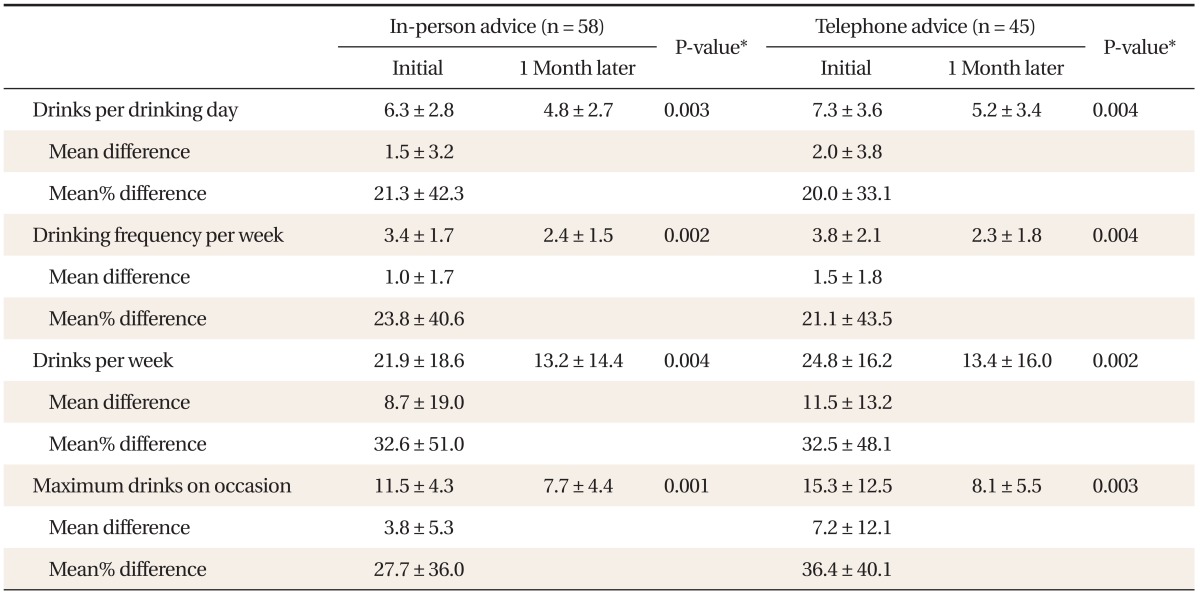
3. Changes in Drinking Habits One Month after Brief Advice
The mean ± SD drinks per week in the in-person advice group was 21.9 ± 18.6 before the brief advice, and decreased significantly (P < 0.005) to 13.2 ± 14.4 after. The maximum number of drinks in 1 day decreased significantly (P < 0.005) from 11.5 ± 4.3 to 7.7 ± 4.4 drinks. In the telephone advice group, the mean ± SD drinks per week decreased significantly (P < 0.005) from 24.8 ± 16.2 to 13.4 ± 16.0, and the maximum number of drinks ± SD in 1 day decreased significantly (P < 0.005) from 15.3 ± 12.5 to 8.1 ± 5.5 after the brief advice.
The mean ± SD decrease in weekly drinking level was 8.7 ± 19.0 drinks in the in-person advice group and 11.5 ± 13.2 drinks in the telephone advice group. There was no significant difference in the decrease in weekly drinking level between the two groups. The mean decrease in the maximum number of drinks in 1 day was 3.8 ± 5.3 in the in-person advice group and 7.2 ± 12.1 in the telephone advice group. The difference in the decrease in the maximum number of drinks in 1 day was not statistically significant (P > 0.05) between the two groups (Table 3).
4. Factors Related to Improvement in Readiness to Change
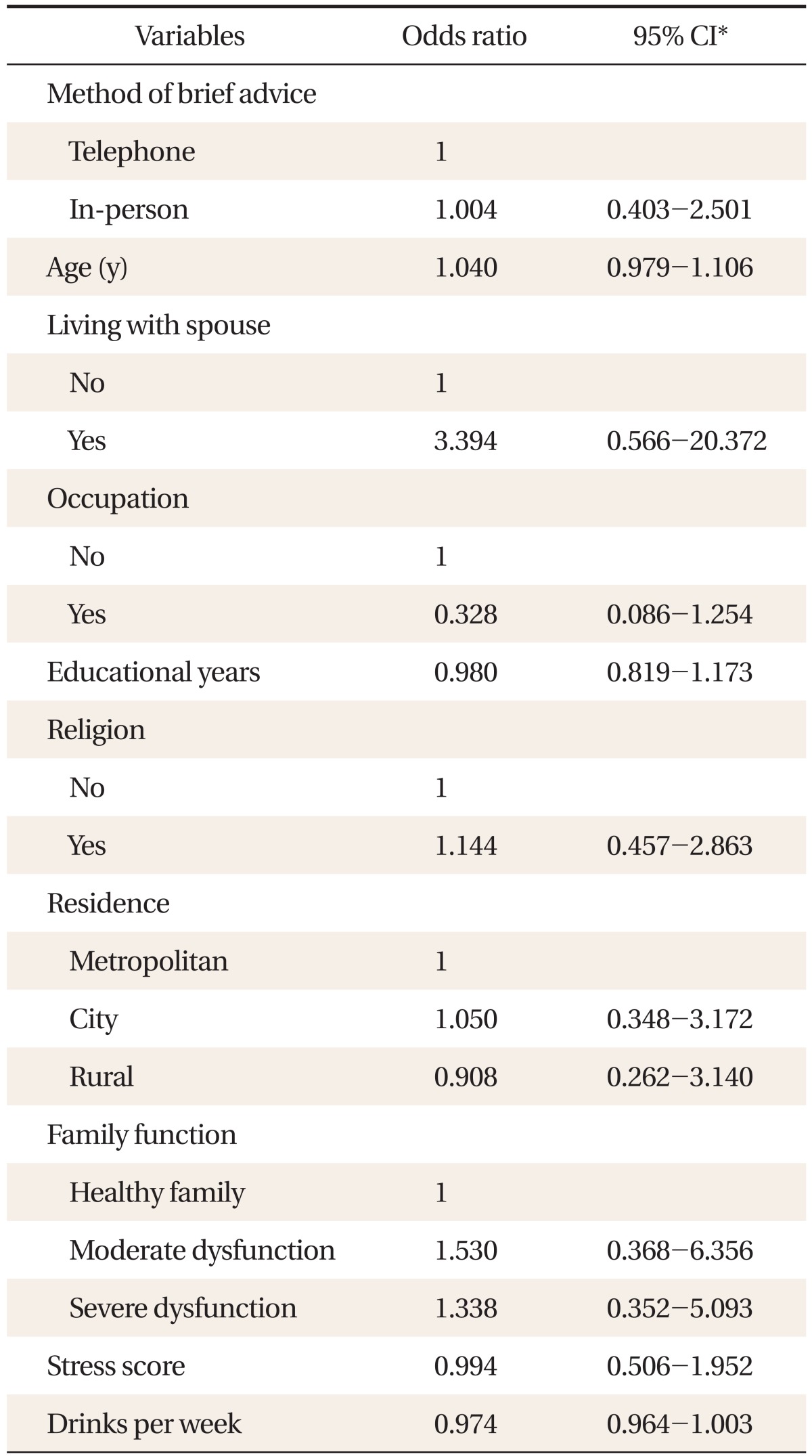
According to the multiple logistic regression analysis, the effect of in-person advice on improvement in readiness to change was not significantly different from that of telephone advice (odds ratio, 1.004; 95% confidence interval, 0.403 to 2.501). In addition, none of the covariates, such as patient age, whether living with a spouse, occupational state, religious state, monthly income, residency, family function score, stress score, or drinks per week, showed a significant effect on improvement in the readiness to change (Table 4).
DISCUSSION
The purpose of this study was to investigate the effect of brief advice on the readiness to change of at-risk drinkers, who are commonly encountered in primary care. Our study showed an improvement in the readiness to change of a patient after receiving brief advice. A previous study by Pal et al.21) also investigated the effect of five minutes of advice on the readiness to change of patients with alcohol use disorders, and reported that the patient distribution pattern of 6 (13.3%) in the precontemplation stage, 32 (71.1%) in the contemplation stage, and 7 (15.6%) in the action stage before the brief advice was changed into 2 (4.5%), 23 (52.3%), and 19 (43.2%), respectively, 1 month after the brief advice. The results of our study, that two minutes of brief advice led to a significant change in the readiness to change one month after the advice was given, is in agreement with the previous study.
Various difficulties in managing drinking problems have been reported. An accurate diagnosis may be difficult, and treatment may take longer than that for general physical problems. Alcohol abuse may be perceived as a lack of morality rather than a medical condition. In addition, the treatment outcome of patients with drinking problems may be viewed negatively.22) However, the results of our study encourage clinicians not to give up on patients with drinking problems. In addition, our study suggests the need for changes in clinicians' negative perception that it is difficult to treat patients with drinking problems.
Pal et al.21) reported that the effect of brief advice on the improvement in readiness to change of a patient did not last three months. The distributions of patients changed to 13 (29.5%) in the precontemplation stage, 26 (59.1%) in the contemplation stage, and 5 (11.4%) in the action stage three months after the advice. In contrast, another study23) reported that the effect of group education on readiness to change of at-risk drinkers lasted for > 1 year. Before participating in the group education, there were 11 (32.4%) patients in the precontemplation stage, 23 (67.6%) in the contemplation stage, and 0 (0.0%) in the action stage, these changed to 2 (5.9%), 16 (47.1%), and 16 (47.1%), respectively, one year after the education. However, our research is limited in its scope because it does not examine whether the effect on the readiness to change of a patient lasts for > 3 months.
The majority of previous studies on telephone intervention dealt only with the effect on the change in a patient's drinking behavior, not with their motivation, which is an important component for improving drinking behavior. In the present study, short and simple advice appeared to be effective in improving the motivational state of a patient. Furthermore, the effect of telephone advice appeared to be the same as in-person advice, even after adjustment for the severity of drinking behavior, family function, stress level, and the demographic characteristics of a patient, including age, whether living with a spouse, monthly income, occupation, religion, and residency. In other words, the effect on the improvement of the motivational state of a patient is not affected by the method used to deliver the brief advice. However, it is difficult to conclude from our results that brief advice is effective in improving the motivation of patients, because our study was performed without a control group that did not receive the simple advice. This would be difficult from a methodological perspective because for medical ethical reasons, a doctor must recommend that any at-risk drinkers moderate their drinking when visiting the office.
Bischof et al.24) compared the effect of a brief telephone intervention on at-risk drinkers with that based on outpatient treatment. The results showed a decrease in daily alcohol intake by 12.2 ± 38.3 g in the telephone intervention group and 13.0 ± 37.2 g in the outpatient intervention group, however, these differences were not significant. Research by Oslin et al.25) also showed that the weekly drinking level of at-risk drinkers in old age decreased significantly from 26.1 ± 20.1 to 17.4 ± 12.3 drinks four months after the telephone intervention. These results suggest that brief intervention by telephone leads to time- and cost-saving results when managing at-risk drinkers compared with interventions focused on hospital treatment. Our study showed no significant difference between the two groups in terms of the improvements in both weekly drinking level and the maximum number of drinks in one day, which is in agreement with previous studies. Accordingly, it seems that telephone advice is a useful method of intervention in patients with drinking-related behavior. The strength of telephone intervention is that it is easier to focus on the problem at a low cost in both money and time. This method may also ensure inclusion of patients with treatment limitations due to personal circumstances.
Regarding the demographic characteristics of the subjects, the mean age of the patients in the in-person advice group was 50.1 years, which was significantly higher than the 44.9 years in the telephone advice group. It seems that younger patients are more likely to have jobs, which makes them less likely to have spare time. There were also more patients not living with a spouse in the telephone advice group compared with those in the in-person advice group. This may be because the patients in the telephone advice group were younger and thus less likely to be married.
There were many dropouts during the follow-up telephone interview because respondents' level of focus decreased as they were asked to answer increasing numbers of questions on drinking behavior during the last month and on their readiness to change. For convenience, the Short Form Stages of Change questionnaire developed by Rollnick et al.14) was considered as a more appropriate tool. However, the reliability and validity of the questionnaire has not yet been proven in Korea.
Some limitations of this study in terms of generalizing the results should be addressed. The subjects were all male. Therefore, the results may not apply to females. In addition, the patients were not classified randomly into in-person or telephone advice groups because of methodological difficulties. Moreover, the results of self-reports were used as observational variables without tracking the biological markers related to drinking. This study used a filling-up questionnaire before and telephone questioning after the brief advice. The differences in the method of questioning should be taken into consideration when interpreting the results. Finally, this study investigated the effect of simple advice on a patient's readiness to change only one month after the advice. Therefore, further long-term studies are needed to investigate the effect of simple advice on an at-risk drinker's readiness to change.
Notes
No potential conflict of interest relevant to this article was reported.