The Relationship between Obesity and the High Probability of Dementia Based on the Body Mass Index and Waist Circumference
Article information
Abstract
Background
For an early detection and prevention of dementia, there are growing concerns about the high-risk group for dementia and mild cognitive impairment. With an increase of obesity and its complications, obesity has become a major public health problem. Therefore, the aim of this study was to investigate the relationship between obesity and the high probability of dementia.
Methods
This study was done with subjects aged 60 to 89 years who visited a health promotion center, from April 1, 2008 to April 30, 2008. A total of 293 subjects (164 males and 129 females) were included in the evaluation of cognitive function using the Korean version of the Seven Minutes Screen test. Logistic regression models were used to analyze the association between obesity and the high-risk group for dementia.
Results
Among a total of 293 subjects, 71 subjects (29 males and 42 females) had a high probability of dementia. When compared to normal body mass index (BMI) group, overweight and obesity groups had about a 2.2-fold and 2.4-fold higher probability of dementia (95% confidence interval [CI], 0.97 to 4.99 and 95% CI, 1.07 to 5.46, respectively). When compared to non-obese and non-abdominal obesity group, non-obese and abdominal obesity group and obese and abdominal obesity group had about a 1.5-fold and 2.0-fold higher probability of dementia (95% CI, 0.59 to 3.95 and 95% CI, 1.09 to 3.84, respectively).
Conclusion
This study shows that as the BMI increased, subjects had a higher probability of dementia; additionally, it suggests that abdominal obesity could be related to a higher probability of dementia.
INTRODUCTION
Dementia, more specifically Alzheimer's disease, has increased in prevalence due to population aging and has become an important public health problem with an increase in the socio-economic burden.1) Dementia is a syndrome of acquired cognitive defects sufficient to interfere with social or occupational functioning that results from various central neurodegenerative and ischemic processes and affects memory, judgment, speech, comprehension, execution, orientation, and learning.2,3) On the other hand, mild cognitive impairment (MCI) is a state that has memory impairment beyond that expected for a particular age and educational background but is not considered dementia yet. Thus, subjects with MCI maintain overall cognitive function and normal activities of daily living.4)
In one study, about half of the patients with isolated memory loss progressed to dementia during 48 months of follow-up.5) According to the Braak stages, a patho-anatomical classification of Alzheimer' disease, stages V-VI correspond to clinical Alzheimer' s disease and stages I-IV correspond to the prodromal phase of Alzheimer's disease or MCI.6) The few aforementioned studies highly suggest that MCI could be a precursor to Alzheimer' s disease. Considering that Alzheimer's disease is particularly caused by irreversible damage to neurons and at present, there is no cure for dementia,7) there are growing concerns about MCI as the diagnostic and therapeutic turning point in which progression to dementia could be halted.4,8)
With an increase in obesity, studies about the relationships between obesity and dementia have increased. Haan and Wallace9) showed that obesity has emerged as an important influence on the risk of both vascular and Alzheimer's dementia, and Whitmer et al.10) reported that more than three decades later, central obesity in midlife increases the risk of dementia independent of diabetes and cardiovascular comorbidities. However, there are few studies on the relationship between obesity and dementia in Korea. Therefore, the aim of this study was to investigate the relationship between obesity and the high probability of dementia using the Korean version of the Seven Minute Screen test (7MSK),11) a useful tool for early dementia screening.
METHODS
1. Study Participants
This study was done with subjects who were 60 to 89 years of age and who visited a health promotion center in Seoul, Korea, from April 1, 2008 to April 30, 2008. A total of 343 subjects (192 males and 151 females) were interviewed with a questionnaire and examined by a medical doctor and a trained nurse using the 7MSK. A total of 293 subjects (164 males and 129 females) were finally included in this study, and 29 subjects were excluded for the following reasons: had a medical history of dementia, were suspected of having dementia based on the Diagnostic and Statistical Manual of Mental Disorders-IV criteria, or had a medical history which affected cognitive functions such as stroke, Parkinsonism, or brain injury; moreover, eighteen subjects whose results were 'RE, diagnosis deferred' by the 7MSK, one subject who did not have their waist circumference measured and two underweight subjects were excluded. The abovementioned 'RE, diagnosis deferred' means that there is insufficient data to make a judgment.
2. Data Collection
Each subject participated in an interview with a medical doctor who collected answers to a questionnaire that included age, sex, education level, life habits such as smoking status, alcohol consumption and exercise, medications, and medical problems such as hypertension, diabetes, dyslipidemia, dementia, and stroke. A trained nurse measured the body mass index (BMI, weight kg/m2) and waist circumference of each subject. According to the World Health Organization guideline for waist circumference measurements, a measuring tape was placed around the trunk, at a point midway between the lower costal margin and the iliac crest, while the subject was standing with their feet about 25-30 cm apart. The measuring tape was placed snugly around the abdomen but without compressing the underlying soft tissues. Finally, during the last step, the waist circumference was recorded to the nearest 0.5 cm at the end of a normal expiration.
Education level was classified as under elementary dropout, after elementary graduation and under high school dropout, after high school graduation and under university dropout, and over university graduation. Smoking status was classified into current smokers, ex-smokers, and non-smokers. Alcohol consumption was divided into no drinking, drinking less than and equal to 58 g of alcohol (1 bottle of 20% soju) per week, and drinking more than 58 g of alcohol (1 bottle of 20% soju) per week. The frequency of sweating exercise was categorized into one or more times a week and less than once per week. Laboratory tests, which were done after the subjects had fasted for at least 12 hours, included fasting plasma glucose, total cholesterol, triglyceride (TG), high density lipoprotein cholesterol, low density lipoprotein (LDL) cholesterol (calculated value), and serum creatinine.
Blood pressure was measured in the right upper arm using an automatic sphygmomanometer after resting for at least 10 minutes. Hypertension, dyslipidemia, and diabetes mellitus were defined as follows: 1) hypertension, three times more the systolic blood pressure ≥ 140 mm Hg or a diastolic blood pressure ≥ 90 mm Hg,12) or the use of antihypertensive medication; 2) dyslipidemia, total cholesterol levels ≥ 240 mg/dL, LDL levels ≥ 160 mg/dL, or TG levels ≥ 200 mg/dL,13) or the use of lipid lowering medication; and 3) diabetes mellitus, fasting plasma glucose ≥ 126 mg/dL,14) or the use of anti-diabetic medication or insulin.
3. Evaluation of Cognitive Function
A medical doctor and trained nurse evaluated the subjects using the 7MSK15) after giving a sufficient explanation of its purposes and content. The 7-Minute Screen test was invented by Solomon et al.16) in 1997 and is not influenced by age and education level. It is a useful tool for early dementia screening in a primary care setting because it has a reasonable validity (sensitivity and specificity more than 90%) for MCI and can be administered in a brief period. The 7-Minute Screen test consists of four brief tests such as Benton temporal orientation (BTO), enhanced cued recall (ECR), clock drawing (CD), and category fluency (CF) and uses a logistic regression model, "log[P/(1-P)] = 35.59 - 1.303 × ECR - 1.378 × CF + 3.298 × BTO - 0.838 × CD", to estimate the probability of having dementia. The results of the 7-Minute Screen test are classified into three categories: Low (low probability of dementia) if P < 0.3, High (high probability of dementia) if P > 0.7, and RE (diagnosis deferred) if 0.3 ≤ P ≤ 0.7. 'High' means that the probability a subject has dementia characteristic of Alzheimer's disease is high and further diagnostic work-up is necessary. 'Low' means that the probability a subject has dementia characteristic of Alzheimer's disease is low and further diagnostic work-up is not necessary, except for cases in which dementia is clinically definite. 'RE' means that there is insufficient data to make a judgment and it would be advisable to rescreen in 6 to 9 months.17)
4. Surrogate Indices of Obesity
BMI was calculated after a trained nurse measured the height and weight of each subject using an automatic anthropometer. BMI was classified into four categories: < 18.5 kg/m2 for underweight, ≥ 18.5 kg/m2 and < 23.0 kg/m2 for normal weight, ≥ 23.0 kg/m2 and < 25.0 kg/m2 for overweight, and ≥ 25.0 kg/m2 for obesity.18) Abdominal obesity was defined as a waist circumference of ≥ 90 cm for men and ≥ 85 cm for women, which were recommended by the Korean Society for the Study of Obesity19) in 2006.
5. Statistical Analyses
To compare the socio-demographic factors and laboratory results between the high-risk and low-risk groups for dementia, the chi-square test and independent student t-test were used to analyze categorical and continuous variables, respectively.
To evaluate the association between increased BMI and a high probability of dementia, logistic regression models were used to adjust for age, sex, education level, smoking status, alcohol consumption, exercise level and comorbidities such as hypertension, diabetes, and dyslipidemia. Moreover, to evaluate the association between the presence or absence of obesity and abdominal obesity and a high probability of dementia, logistic regression models were also used. All analyses were done with SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Statistical significance was set at a P-value and confidence interval of < 0.05 and 95%, respectively.
RESULTS
1. Characteristics of the Study Subjects
A total of 293 subjects consisting of 164 males (56.0%) and 129 females (44.0%) were included in this study. From the results of the 7MSK, the subjects were classified into two groups: a low-risk group (n = 222, 75.8%) and a high-risk group (n = 71, 24.2%) for dementia. The mean age of the high-risk group for dementia (73.9 years) was higher than that of the low-risk group for dementia (68.5 years; P < 0.001). The mean BMI was higher in the high-risk group (24.4 kg/m2) than that of the low-risk group (23.5 kg/m2; P < 0.05). The mean waist circumference was longer in the high-risk group (85.5 cm) than that of the low-risk group (82.5 cm; P = 0.005).
Female subjects had a higher probability of dementia than that of male subjects (P < 0.05). Subjects with lower levels of education were associated with a high probability of dementia (P < 0.001). Subjects, who exercised more than once per week, were associated with a low probability of dementia (P < 0.05). There was a significant difference in the past medical history for dyslipidemia between the high-risk and low-risk group for dementia (P < 0.05).
There was no significant difference in classic cardiovascular risk factors, such as smoking, alcohol consumption, and a past medical history of hypertension or diabetes between the high-risk and low-risk group for dementia (P > 0.05) (Table 1).
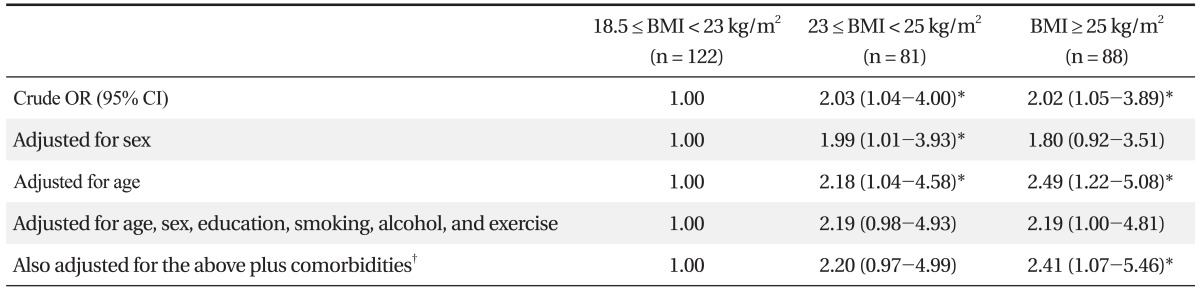
2. The Association between BMI and a High Probability of Dementia
When compared to the normal BMI group, the overweight and obesity groups had about a 2-fold higher probability of dementia (crude odds ratio [OR], 2.03; 95% confidence interval [CI], 1.04 to 4.00 and crude OR, 2.02; 95% CI, 1.05 to 3.89, respectively) and when adjusted for age, had about a 2.2-fold and 2.5-fold higher probability of dementia (95% CI, 0.97 to 4.99 and 95% CI, 1.07 to 5.46, respectively). These findings were statistically significant (P < 0.05).
Multiple logistic regression analysis was done to adjust for age, sex, education level, smoking status, alcohol consumption, exercise level, and medical history of hypertension, diabetes, and dyslipidemia and showed that when compared to the normal BMI group, the overweight and obesity groups had about a 2.2-fold and 2.4-fold higher probability of dementia (95% CI, 0.97 to 4.99; P = 0.06 and 95% CI, 1.07 to 5.46; P < 0.05, respectively) (Table 2).
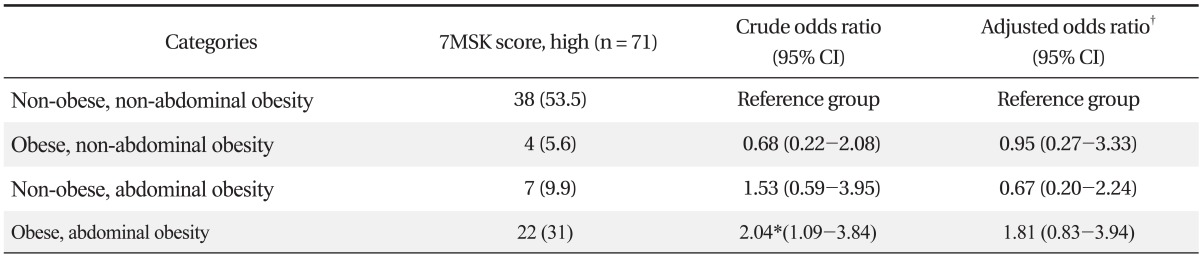
3. The Association between the Presence or Absence of Obesity and Abdominal Obesity and a High Probability of Dementia
When compared to the non-obese and non-abdominal obesity group, non-obese and abdominal obesity group and obese and abdominal obesity group had about a 1.5-fold and 2.0-fold higher probability of dementia (95% CI, 0.59 to 3.95; P = 0.38 and 95% CI, 1.09 to 3.84; P < 0.05, respectively). Multiple logistic regression analysis was done to adjust for age, sex, education level, smoking status, alcohol consumption, exercise level, and medical history of hypertension, diabetes, and dyslipidemia and showed that when compared to the non-obese and non-abdominal obesity group, the obese and abdominal obesity group had about a 1.8-fold higher probability of dementia (95% CI, 0.83 to 3.94; P = 0.13), but the obese and non-abdominal obesity group and the non-obese and abdominal obesity group had about a 0.05-fold and 0.33-fold lower probability of dementia (P = 0.94 and P = 0.51, respectively) (Table 3).
DISCUSSION
The reason why obesity is associated with dementia is not yet known exactly. However, it is believed that obesity has a harmful influence on the brain long before the symptoms of dementia manifest. A variety of bio-available metabolites that adipose tissues secrete affect the brain directly through the blood brain barrier, of which leptin, an key factor in the development of obesity, is known to be involved in the deposition of amyloid-β protein.20-23) The deposition of amyloid-β protein provokes extensive brain damage and causes Alzheimer's disease.20)
Indirectly, hyperleptinemia, a major causative factor for obesity, activates the sympathetic nervous system22,24) and causes shrinkage of the brain architecture and cerebrovascular diseases.25,26) Even though there is no evidence that cerebrovascular diseases play a direct role on the deposition of amyloid protein, it is believed that an increase in body fat tissue, an important factor in vascular diseases causes dementia indirectly through cerebrovascular diseases since a study using brain autopsies of individuals with cerebrovascular diseases showed an increased frequency of amyloid-β protein.27,28)
This study investigated the association between the high-risk group for dementia and obesity based on the BMI and waist circumference. When compared to the normal BMI group, the overweight and obesity groups had about a 2-fold higher probability of dementia (P < 0.05) and even after adjusting for age, sex, education level, smoking status, alcohol consumption, exercise level, and medical history of hypertension, diabetes, and dyslipidemia, the obesity group had about a 2.4-fold higher probability of dementia (P < 0.05).
When compared to the non-obese and non-abdominal obesity group, the obese and abdominal obesity group had about a 2.0-fold higher probability of dementia (P < 0.05), but after adjusting for age, sex, education level, smoking status, alcohol consumption, exercise level, and medical history of hypertension, diabetes, and dyslipidemia, there was no statistical significance (P = 0.13); however, this finding corresponds with a report by Jeong et al.29) that general obesity (BMI ≥ 25 kg/m2) and poor cognition were strongly associated in the presence of abdominal obesity.
The aim of this study was to investigate the association between obesity and subjects with a high risk for dementia, but not considered dementia yet. It was a cross-sectional study that suggests obesity could be related to a high probability of dementia, based on the BMI and waist circumference. Further large-scale prospective studies are needed because there are only a few studies on the relationship between obesity and the high-risk group for dementia in South Korea.
Since prevention of degenerative dementia including Alzheimer's disease is not yet promising, further studies are needed to determine if weight reduction and appropriate weight control could halt the progression of dementia in subjects with a high probability of dementia, especially for MCI.
This study has the following limitations. First, the reliability of the data decreases since the information on smoking status, alcohol consumption, exercise level, education level, and comorbidities were collected through a self-reporting questionnaire. However, data collection was completed under the guidance of a medical doctor to maintain consistency. Second, individuals that were diagnosed as having dementia or suspected of having dementia were excluded in this study; however, during the exclusion process, they were not examined by a dementia specialist or given any additional neurophysiologic tests. Thus, there is a possibility not to exclude the demented individuals entirely. Third, it was reported that the subtests of the 7MSK are influenced by education level, but this study used a calculation method invented by Solomon et al.16) in 1997. Therefore, the bias induced by the education level was not corrected for during the test process.
Fourth, this study may not be generalized to the entire population since the study participants were enrolled only in one general hospital. Fifth, this study is a cross-sectional study and had too small of a sample size to avoid a type II error completely. Sixth, obese and non-abdominal obesity group and non-obese and abdominal obesity group had too small a number of subjects with a high probability of dementia to have enough statistical power (number size, 4 and 7, respectively).
In conclusion, this study shows that as the BMI increased, subjects had a higher probability of dementia characteristic of Alzheimer's disease; additionally, it suggests that abdominal obesity could be related to a higher probability of dementia.
Notes
No potential conflict of interest relevant to this article was reported.