A Case of Scrub Typhus Complicated by Acute Calculous Cholecystitis
Article information
Abstract
We report a case of acute calculous cholecystitis through scrub typhus. A 69-year-old woman presented with a history of general myalgia, fever, and right abdominal pain. She referred to our hospital for surgical treatment of clinically suspected acute cholecystitis. Physicians concluded the cause of cholecystitis as gall bladder (GB) stone and proper antibiotics treatment of scrub typhus was started later. The patient developed acute respiratory distress syndrome and multi organ failure through scrub typhus. Five days after admission, the patient was treated with proper antibiotics and discharged on the 13th day after starting doxycycline treatment without any sequelae. In areas endemic for tsutsugamushi disease, even though a patient with GB stone presents with symptoms of acute cholecystitis, careful history and physical examination are required to reveal the existence of eschars or skin eruptions.
INTRODUCTION
Scrub typhus is clinically manifested by fever, generalized lymphadenopathy, diffuse myalgia, headache, maculopapular skin rash, and eschars at the site of chigger feedings.1) The clinical course is usually self-limited with spontaneous recovery occurring in a few days. However, severe infections may be complicated by pneumonitis, acute renal failure, acute respiratory distress syndrome (ARDS), myocarditis, and central nervous system dysfunction, including delirium and confusion.2-7) Few studies have reported the gastrointestinal manifestation of scrub typhus.8-11) Inaba and associates have reported a case of tsutsugamushi disease complicated with cholecystitis in Japan12); however, acute calculous cholecystitis with multiorgan failure has not been previously reported in scrub typhus. In this study, we report a case of patients with gall bladder (GB) stones who developed acute cholecystitis, ARDS, and multi organ failure after scrub typhus infection.
CASE REPORT
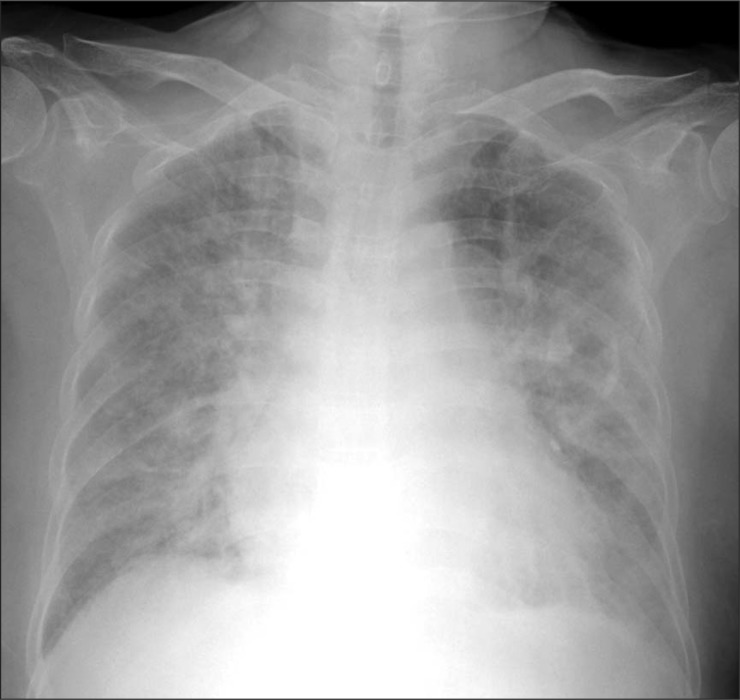
A healthy 69-year-old woman presented with a 3 day history of general myalgia, fever, and nausea. She resided in an urban area and had picked ginkgo nuts in the mountains 10 days before her symptoms appeared. She visited a local hospital because of right upper abdominal tenderness and was subsequently referred to our hospital for surgical treatment of clinically suspected acute cholecystitis. On admission, her vital signs were checked: blood pressure was 110/90 mm Hg; pulse rate, 78/min; respiratory rate, 24/min; and body temperature, 38.5℃. On physical examination, enlarged cervical lymph nodes and right upper abdominal tenderness with rebound tenderness was observed. No eschar was found on the trunk. According to laboratory test results, the white blood cell count was 4,510/mm3 with 70.6% segmented neutrophils; hemoglobin, 14.0 g/dL; platelet count, 57 × 103/mm3; C-reactive protein, 17.51 mg/dL; aspartate aminotransferase, 374 IU/L; alanine aminotransferase, 254 IU/L; alkaline phosphatase, 982 IU/L; lactate dehydrogenase, 1,141 IU/L; total protein, 7.0 g/dL; albumin, 3.8 g/dL; and total bilirubin, 1.2 mg/dL. Chest radiography and electrocardiogram revealed no abnormalities. Abdominal computed tomography (CT) showed edematous change in the GB wall with GB stones (Figure 1). Because acute calculous cholecystitis was suspected, intravenous ceftriaxone (2 g/d) was initiated, and percutaneous cholecystostomy was performed. However, the patient suffered from sustained symptoms, including nausea and abdominal pain.
Abdominal computed tomography showed thickened gall bladder (GB) wall and distension of GB with GB stone.
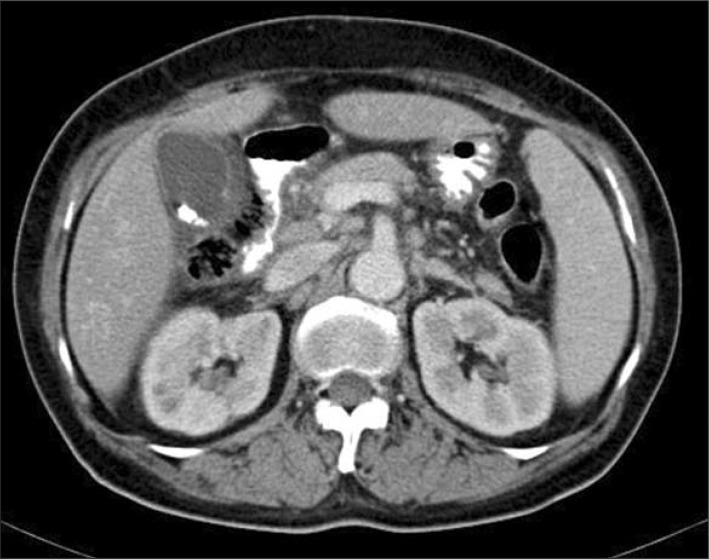
Four days after admission, the patient developed progressive shortness of breath, increasing sputum production, hypoxemia, and confusion, which necessitated the delivery of oxygen at 5 L/min via nasal cannula. Arterial blood gas analysis revealed a pH of 7.45; PaCO2, 36 mm Hg; PaO2, 67 mm Hg; and HCO3-, 25. Follow-up chest radiography showed extensive airspace consolidation in both lungs (Figure 2). An endotracheal intubation was performed and the patient was admitted to the intensive care unit (ICU). The next day, she developed a maculopapular rash on her trunk and face. Sputum and blood cultures were negative; however, based on a suspicion of scrub typhus with acute cholecystitis and ARDS, the patient was treated with oral doxycycline (200 mg/d) and intravenous piperacillin (4.5 g/d). Serologic test for Orientia tsutsugamushi (O. tsutsugamushi) were positive with a titer of 1:5,120. On the ninth day after doxycycline treatment, multi-organ function appeared to return to a normal state. The patient' s mental alertness had improved and follow-up chest radiography showed that all previous abnormalities had resolved. The patient was discharged on the thirteenth day after starting doxycycline treatment; complete blood count and biochemistry results had returned to normal range, and the patient had completely recovered. The percutaneous cholecystostomy catheter was removed at outpatient clinic after discharge, and she underwent elective cholecystectomy without complications. The number of stones was three and all were black pigment stones.
DISCUSSION
Scrub typhus is a mite-borne infectious disease caused by O. tsutsugamushi, intracellular microorganism. Eschars at the site of chigger feeding, lymphadenopathy, and maculopapular rash are typical signs. Fever, headache, anorexia, nausea, headache, diffuse myalgias, abdominal pain, and relative bradycardia may also be present. With proper medication (doxycycline) recovery is prompt and uneventful. Without proper treatment, fever generally lasts for 2 weeks. The fatality rate depends on the area, strain of rickettsia, and treatment, but is consistently higher in elderly patients.13) Reported severe complications of scrub typhus include pneumonia, myocarditis, meningoencephalitis, acute renal failure, hepatitis, gastrointestinal bleeding, and septic shock.4-7,14,15) A diagnosis can be made in the presence of a fourfold or greater rise in antibody titer to O. tsutsugamushi antigen by indirect immunofluorescence or Weil-Felix slide agglutination.16)
Scrub typhus produces disseminated multi-organ vasculitis and perivasculitis of the small vessels via destruction of endothelial cells and the perivascular infiltration of leukocytes.17,18) The mechanism responsible for the development of acute cholecystitis may be related to the vasculitis.
Inaba and associates reported tsutsugamushi disease complicated with cholecystitis,12) but this complication is rare in the patient with solitary scrub typhus. Wang et al.19) reported a patient with concomitant leptospirosis and scrub typhus complicated with acute acalculous cholecystitis.
Because our patient had symptoms that included fever, right upper quadrant pain, and the result of abdominal CT-revealed GB wall edema with GB stones, early treatment was focused on acute calculous cholecystitis without considering other possible options, such as scrub typhus. In our case, additional symptoms included ARDS and confusion necessitating mechanical respiration, which were processed in the ICU. Scrub typhus in elderly patients is known for its tendency for severe complications; our patients were elderly and experienced severe complications. More case studies are needed to assess the association of acute cholecystitis in patients infected with scrub typhus and pre-existing GB stones.
In our case, the patient showed relative bradycardia: an unexpectedly low heart rate response for a given increase in body temperature despite signs of infection. A study of 100 febrile patients infected with O. tsutsugamushi reported a prevalence of relative bradycardia of 53%.20) The existence of pulse-temperature dissociation may help physicians identify tsutsugamushi disease in patients with acute calculous cholecystitis.
Scrub typhus can be diagnosed by assessing the patient's history of exposure, symptoms, clinical signs, and lab results, so it is important for clinicians to be cognizant of the disease. In areas endemic for tsutsugamushi disease, even though a patient with GB stone presents with symptoms of acute cholecystitis, careful history and physical examination are required to reveal the existence of eschars or skin eruptions. In addition, if a patient's heart rate is below 100 beats/min with pyrexia, the physician should be aware of the possibility of scrub typhus. Prompt treatment with doxycycline can shorten clinical illness and reduce mortality.
ACKNOWLEDGMENTS
This study was supported by a 2012 research grant from Pusan National University Yangsan Hospital.
Notes
No potential conflict of interest relevant to this article was reported.