A Comparison of the Efficacy and Safety of Non-Steroidal Anti-Inflammatory Drugs versus Acetaminophen in Symptom Relief for the Common Cold: A Meta-Analysis of Randomized Controlled Trial Studies
Article information
Abstract
Background
Non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen are widely used for common cold symptom relief. The objective of this study was to evaluate and compare the efficacy and safety of acetaminophen and NSAIDs in common cold symptom relief using meta-analysis of randomized controlled trial.
Methods
We searched MEDLINE (PubMed), Cochrane, EMBASE, CINAHL, KMbase, KoreaMed, National Assembly Library, and Riss4u for studies released through June 2012. Two authors independently extracted the data. To assess the risk of bias, the Cochrane Collaborations risk of bias tool was used. The Review Manager ver. 5.1 (RevMan) was used for statistics.
Results
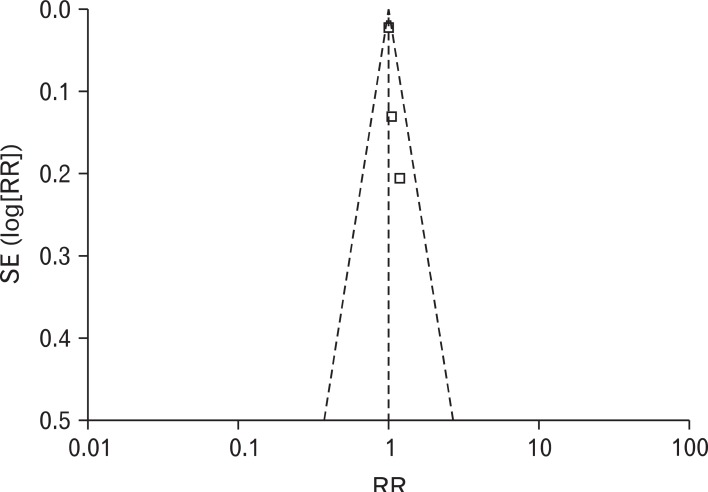
We identified 5 studies. The relative benefit for participants with pain relief was 1.00 (95% confidence interval [CI], 0.96 to 1.05) and I2 = 0%. The existence of the heterogeneity between studies was not important in this study, thus subgroup analysis was not implemented. The relative benefit for participants with rhinorrhea was 1.02 (95% CI, 0.77 to 1.35) and I2 = 0%, which also indicates the existence of heterogeneity was not important. The relative risk of adverse events was 1.14 (95% CI, 0.93 to 1.40), I2 = 0%. There was no apparent asymmetry in the funnel plot.
Conclusion
There was no difference between NSAIDs and acetaminophen in common cold symptom relief.
INTRODUCTION
The common cold is an acute respiratory tract infection and is a common and widespread disease in all ages. Typically, it shows mild symptoms but if it persists over a week, out-patient treatment may be needed.1) The common cold presents acute symptoms such as cough, runny nose, sneezing, sore throat, and hoarseness, accompanied by fever, chill, muscle pain, and headache. Among them, nasal symptoms are the most common.2)
Although in most cases, a virus is the cause of the common cold, anti-viral treatment is not appropriate in Korea, as antiviral medicine administration for the common cold is not approved by the Korea Food and Drug Administration and is not available in Korea.3-5) As the causal treatment of the common cold is difficult, the purpose of common cold treatment is relief of various symptoms. As symptoms are resolved in 7 to 10 days spontaneously, allopathy is usually adopted.6) Representative allopathic treatment includes prescription of non-steroidal antiinflammatory drugs (NSAIDs) and acetaminophen to resolve chills, muscle pain, headache, and fever.1)
A meta-analysis in 2009 reported that NSAIDs did not give much relief for other symptoms, although they were helpful for pains from the common cold,5) and there were reports that acetaminophen was effective against upper airway infections, especially symptoms such as sore throat,7) headache,8) and fever.9)
On the other hand, according to many studies, it is common for NSAIDs to have adverse effects such as peptic ulcer and gastrointestinal disorders, and a recent meta-analysis reported that they increase the risk of myocardial infarction and cardiac insufficiency, and adverse effects are dose proportional.10-12) On the other hand, not many adverse effects were reported with acetaminophen at normal dosage, and it was reported to have relatively less gastrointestinal adverse effects than NSAIDs.13) Until now, the choice between two medications to mitigate the symptoms of the common cold has been made according to the characteristics and preference of the doctor or the patient, and there has not been a meta-analysis of randomized controlled studies that comprehensively compared the effects of the two medications. Thus, the purpose of this study was to compare the effects and safety of NSAIDs and acetaminophen in the relief of symptoms of the common cold through a meta-analysis of randomized controlled trials.
METHODS
In order to compare the efficacy and safety of NSAIDs and acetaminophen on common cold patients, a meta-analysis was performed on randomized controlled trials.
1. Inclusion Criteria
Published randomized controlled trials comparing the effects of oral NSAIDs versus acetaminophen on common cold symptom relief were included. The common cold was defined by symptoms of runny nose, nasal congestion and sneezing, regardless of symptoms of headache and coughs. Studies on patients diagnosed as other than common cold, such as acute sinusitis, exudative tonsilitis, acute laryngitis, tracheitis, acute laryngotracheobronchitis, epiglottitis, tympanitis lower airway infectious diseases (pneumonia, bronchitis and so on), chronic respiratory disease, or allergic rhinitis were excluded. Studies using oral NSAIDs and oral acetaminophen for the treatment of the common cold were included regardless of dosage form or amount, but single-dose studies were excluded. Studies reporting overall evaluation of relief of common cold symptoms, analgesic effects, and nonanalgesic effects such as runny nose or cough were included.
2. Searches
The final search was made in June, 2012. A professional librarian made the search. The key words were selected through discussion between authors and the librarian. There was no restriction on the language of published articles.
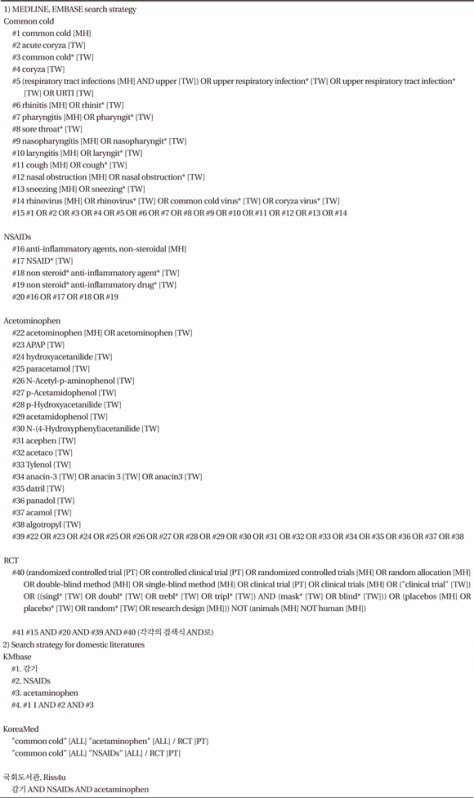
Searches were made on MEDLINE (PubMed), EMBASE, the Cochrane Central Register of Controlled Trials (CENTRAL), and CINAHL for studies released through June 2012. For domestic studies, KoreaMed, KMbase, National Assembly Library and Riss4u were searched. Keywords were selected to include common cold-related, NSAIDs-related, acetaminophen-related, and randomized controlled trial-related words. Detailed keywords are shown in Appendix 1. Additional searches were made for the references of the included articles.
3. Studies Selection
Two independent authors selected studies satisfying the inclusion criteria from the search results, and disagreement was settled by discussion and consensus between two authors. When agreement could not be made, final selection was made with the mediation of a third author.
4. Assessment of Risk of Bias in Included Studies
For the methodological quality evaluation of the included studies, two independent authors made assessment using the Cochrane Collaboration's tool for assessing risk of bias.14) Each item was classified as low risk, high risk, or unclear; low risk for low risk of bias, high risk for high risk of bias, and unclear for difficult to decide. We resolved disagreements by discussion.
5. Data Extraction
Two independent authors independently carried out data extraction using standard data extraction forms. When authors did not agree, two authors tried to find consensus through discussion.
6. Statistics Analysis
Relative benefit (RB) or relative risk (RR) was proposed with 95% confidence interval (CI). To analyze the study results, Review Manager ver. 5.0 (RevMan; Cochrane Collaboration, Oxford, UK),15) a statistics program was used. The results were summarized in a table through forest plot, and funnel plot was applied to check for publication bias.
To identify heterogeneity, the I2 test was used. I2 statistics are the form of statistics quantifying inconsistency. I2 ranges from 0% to 100%. Here, values between 0% and 40% can be interpreted as unimportant heterogeneity, up to 60% as moderate heterogeneity, and over 60% as considerable heterogeneity.16) When heterogeneity did not exist, it was analyzed as a fixed-effect model. When heterogeneity existed, the group was divided into subgroups with similar characteristics to investigate reasons for heterogeneity. If the heterogeneity could not be resolved, a random effect model was applied. When heterogeneity was not significant, subgroup analysis was not performed.
RESULTS
1. Description of Studies
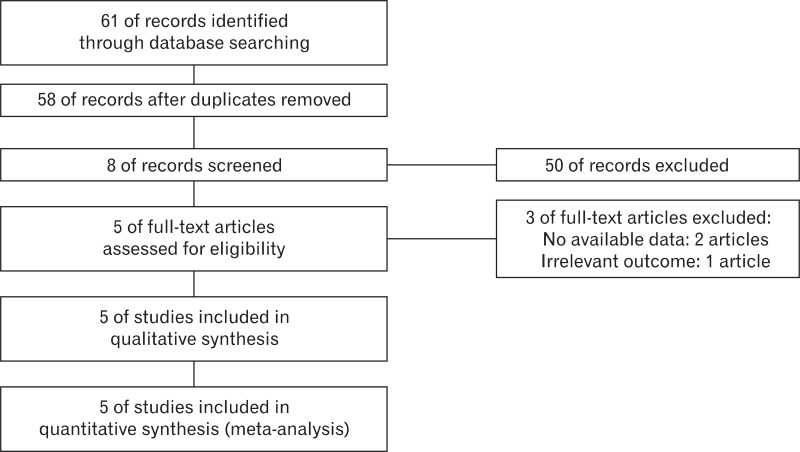
Sixty-one articles were retrieved through an electronic search, 35 articles in MEDLINE (PubMed), 4 articles in Cochrane, 15 articles in EMBASE, and 7 articles in CINAHL. There were no domestic articles. Fifty-eight abstracts excluding redundant studies were screened. Of these, 5 studies met the inclusion criteria: Moore et al.,17) Ulukol et al.,18) Ugazio et al.,19) Graham et al.,20) and Phadke et al.21) (Figure 1).
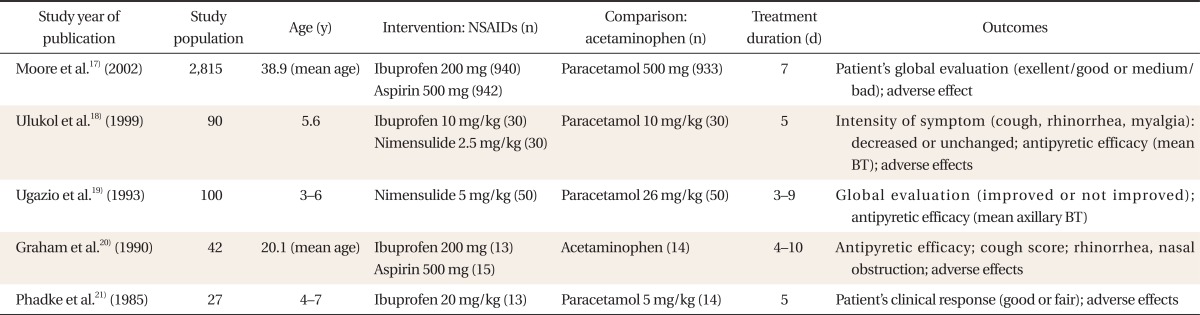
A total of 3,074 participants were included. The NSAIDs group included 2,033 participants and the acetaminophen group included 1,041. In all studies, the patients showed clinical symptoms of the common cold, and the gender ratio was similar. Symptom relief effects and adverse effects of medications were reported from the third day to the 14th day of administration (Table 1).
2. Risk of Bias in Included Studies
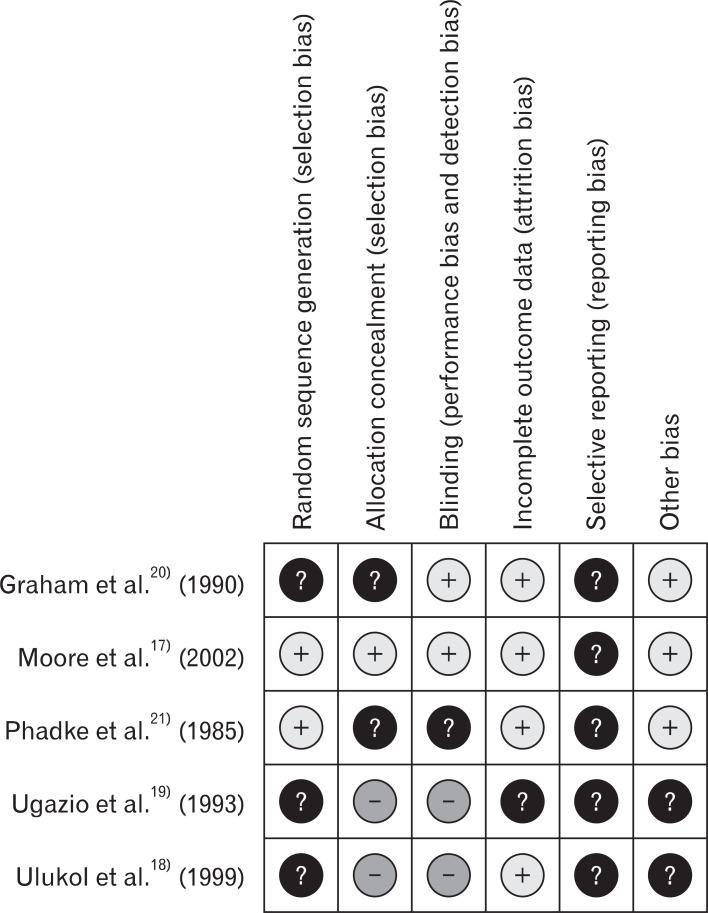
When assessing the risk of bias using Cochrane Collaboration's tool for assessing risk of bias,14) it was found that two studies performed adequate sequence generation. Only one study showed a low risk of bias in allocation concealment, two studies uncertain, and the remaining two studies a high risk of bias. Whether blinding was appropriate in two studies, two other studies did not perform blinding properly. Regarding incomplete outcome data reporting, all the studies except 1 study were uncertain, because they did not report enough to be judged as satisfying the criteria. Selective reporting could not be determined as all of the studies did not report the protocol. For other biases, two studies were evaluated as unclear because they did not provide accurate data for each group (Figure 2).
3. Effects of Intervention
1) Analgesic effects
Three trials reported the analgesic effect of NSAIDs and acetaminophen in the common cold.17,19,21) RB of the NSAIDs group versus the acetaminophen group in analgesic effect in the common cold was 1.00 (95% CI, 0.96 to 1.05), and I2 was 0% (Figure 3). As there was no heterogeneity among studies, subgroup analysis was not performed.
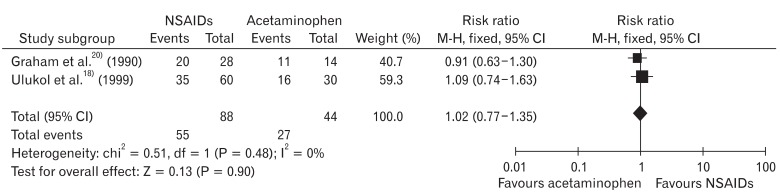
2) Non-analgesic effects (decrease of rhinorrhea)
Two studies18,20) measured outcomes other than the analgesic effect. All reported rhinorrhea decrease effect of acetaminophen and NSAIDs. Among patients who experienced relief of symptoms other than pains, the RB of the NSAIDs group of patients who experienced rhinorrhea symptom relief to the acetaminophen group was 1.02 (95% CI, 0.77 to 1.35), and I2 = 0%, which means there was no heterogeneity (Figure 4).
3) Adverse effects
Adverse effects were reported in 4 studies in total, but in two studies there were no patients who experienced adverse effects. Therefore, two studies17,20) reported adverse effects. Most of adverse effects were trivial and the most frequent adverse effect was digestive system dysfunction. One study reported rectal hemorrhage in the NSAIDs group and hematemesis in the acetaminophen group. There was no statistically significant difference in adverse effects between the two medications but the NSAIDs group tended to experience more adverse effects. This is consistent with previous studies reporting relatively higher adverse effect cases in NSAIDs. RR of patients experiencing adverse effects was 1.14 (95% CI, 0.93 to 1.40), and I2 = 0% (Figure 5).
DISCUSSION
According to meta-analysis of five studies, there was no statistically significant difference in common cold symptom relief between acetaminophen and NSAIDs. As there was no heterogeneity, subgroup analysis was not made.
When the methodological quality of the included studies was evaluated using the Cochrane Collaboration's tool for assessing risk of bias,14) the overall quality of studies was mixed, largely due to missing information regarding randomization procedures and selective reporting. We assessed one study17) as being of high quality. Our outcomes were mainly subjective and blinding of participants may be critical. But the risk of bias regarding blinding was mixed.
In the literature review, the number of clinical studies regarding the comparison of interventions was not sufficient. Out of 3,074 patients included in this meta-analysis, 2,815 subjects were the participants of a study,17) while the other 4 studies were relatively smaller in size. Among them, three studies18,19,21) were on children and the other two studies17,20) on adults. Accordingly the kinds and dose of medications used in the studies were various. No studies used an objective evaluation tool for outcome measure. Most of the studies judged mitigation effects according to subjective symptom reports of the patients. Although relief effects of individual symptoms varied by studies, overall judgment was made to determine the improvement. Accordingly, an article including more patients and using objective outcome measurement tools may be necessary in order to discover if the study results would be different according to subject group, intervention method or intervention results.
Although the two studies included in this meta-analysis judged that NSAIDs were more effective than acetaminophen in pain control, according to meta-analysis results there was no statistically significant difference in effects on common cold symptoms or adverse effects. Based on previous studies, high does NSAIDs could be relatively more effective for pain control.22) However, more adverse effects on the gastrointestinal system were reported in NSAIDs. Therefore, the most appropriate medication should be selected considering that adverse effects of NSAIDs are proportional to dosage and there were less adverse effects from acetaminophen if they were used at the proper dose.
Therefore, when using NSAIDs rather than acetaminophen, care should be taken considering underlying conditions of the patient such as digestive troubles and cardiovascular disease. A large scale cohort randomized controlled clinical experiment is needed to identify the relationship between adverse effects and dosage, an important foundation for comparative selection between two medications.
Notes
No potential conflict of interest relevant to this article was reported.
Appendices
Appendix 1
MEDLINE (PubMed), EMBASE search strategy and search strategy for domestic literatures