Multiple Cavitary Pulmonary Nodules Caused by Mycobacterium intracellulare
Article information
Abstract
Nontuberculous mycobacteria (NTM) have been increasingly recognized as an important cause of chronic pulmonary infections. The Mycobacterium avium complex (MAC), which is composed of two species, Mycobacterium avium and Mycobacterium intracelluare, is the most commonly encountered pathogen associated with NTM lung disease. MAC pulmonary infection typically presents in a fibrocavitary form or a nodular bronchiectatic form. However, there have been atypical presentations of MAC pulmonary infections, including solitary pulmonary nodules (SPN). There have been several previous reports of SPN due to MAC infection in the United States, Japan, and Korea. In 2009, Sekine and colleagues reported a case of MAC pulmonary infection presenting with multiple nodules. To date, however, there have been no cases of NTM lung infection with multiple cavitary pulmonary nodules, and neither a fibrotic change nor nodular bronchiectasis. The present case showed a multiple cavitating nodular lung infection due to MAC, which is very rare and different from the typical presentation of MAC pulmonary infections. We also showed that percutaneous transthoracic needle aspiration can be a useful diagnostic tool to evaluate a case of multiple cavitary nodules.
INTRODUCTION
Nontuberculous mycobacteria (NTM) have emerged as an increasingly important pathogen in the last two decades. Unlike other environmental pathogens that are largely opportunistic in patients with malignancy and immunodeficiency, as well as transplant recipients, NTM can cause significant disease in otherwise healthy individuals. The NTM most commonly associated with pulmonary infection is the Mycobacterium avium complex (MAC), which is a microbial complex of Mycobacterium avium and Mycobacterium intracellulare. There have been many reports concerning its radiologic findings.123)
Although uncommon, several cases of solitary pulmonary nodules (SPN) caused by MAC pulmonary infections have been reported,456) which is different from the typical presentation of MAC. However, a case of a multiple cavitating nodular infection with neither a fibrotic change nor nodular bronchiectasis associated with M. intracellulare has not been reported. We present the case of a 67-year-old Asian woman who had a M. intracellulare infection presenting with multiple cavitating pulmonary nodules, which was differentiated from metastatic lung disease by percutaneous transthoracic needle aspiration (PCNA).
CASE REPORT
The patient was a 67-year-old woman who was referred to Daejeon St. Mary's Hospital because of an abnormal chest computed tomography (CT) scan. She presented to a local clinic after a single occurrence of hemoptysis 10 days prior. The color of the hemoptysis was scarlet and the amount was 1/2 cup of soju, Korean distilled spirits. There were no other symptoms except an intermittent non-productive cough. She was a housewife and a nonsmoker. She had been diagnosed with type 2 diabetes mellitus (DM) 2 years prior at a local clinic, and had since been taking metformin 500 mg after breakfast and dinner. There were no complications associated with the type 2 DM. Glycosylated hemoglobin was 6.7%, and she had good control of her blood sugar levels during hospitalization. After a chest CT was obtained at the local clinic, she was transferred to our hospital to investigate the multiple cavitary pulmonary nodules that were found on the CT scan.
When the patient visited our hospital, her initial vital signs showed a blood pressure of 110/70 mm Hg, heart rate of 80 beats/min, respiratory rate of 16 breaths/min, and body temperature of 36.8℃. Both pupil responses to light were normal and there was no abnormality in the conjunctivae and sclerae. On auscultation, neither crackles nor wheezing was heard in both lung fields, and the heart sound was regular without murmur. There were no signs of hepatomegaly or splenomegaly on palpation of the abdomen. At the first visit to our hospital, the patient did not have any symptoms. There were several round nodules in both the upper lung zone and right middle lung zone, and patch consolidation in the left lower lung zone on the chest radiography, which is suggestive of Mycobacterium tuberculosis (MTB) or metastatic lung disease (Figure 1). Similarly, the chest CT showed centrilobular nodules with a tree-in-bud appearance and three round cavitary nodules in the left apex, the right upper lobe posterior segment, and the right lower lobe superior segment, suggestive of MTB or metastatic lung disease (Figure 2). We isolated the patient because we could not exclude the possibility of MTB along with metastatic lung disease.
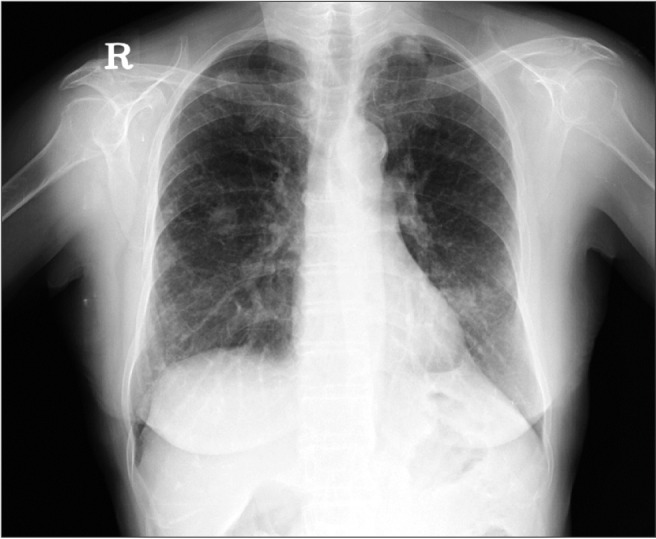
Chest radiography showing several round nodules in both the upper lung zone, and the right middle lung zone, and patch consolidation was observed in the left lower lung zone, suggestive of Mycobacterium tuberculosis lung infection or metastatic lung disease.

Chest computed tomography scan showing diffuse centrilobular nodules with a tree-in-bud appearance and three round cavitary nodules in the left apex, the right upper lobe posterior segment, and the right lower lobe superior segment, suggestive of active pulmonary tuberculosis or metastatic lung disease. (A) Nodule in the right upper lobe posterior segment. (B) Nodule in the right lower lobe superior segment. (C) Nodule in the left apex. (D) Centrilobular nodules with a tree-in-bud appearance.
The initial laboratory parameters were as follows: total leukocyte count 7,500/mm3 (neutrophil 64.6%, lymphocyte 21.1%, monocyte 0.44%); hemoglobin level 12.8 g/dL; and platelet count 217,000/mm3. The level of C-reactive protein was 0.03 mg/dL and other parameters were within the normal limit on the blood chemistry tests. Additionally, the coagulation profile was checked, and the prothrombin time was 11.1 seconds (international normalized ratio 1.35). The basic cardiac rhythm on the electrocardiogram was a regular sinus rhythm.
For further evaluation, we planned to perform a bronchoscopy and PCNA, and the additional imaging examinations were not performed because chest imaging was obtained on the day of the initial hospital visit. A sputum examination was performed. The results of three smears for acid-fast bacilli, and a nucleic acid amplification test for MTB and NTM in sputum were all negative. For further evaluation, a bronchoscopy was performed on the left upper lobe apical segmental bronchus, the right upper lobe posterior segmental bronchus, and the right lower lobe superior segmental bronchus. The smear test of the bronchoscopic washing fluid was positive for acid-fast bacilli. The result of nucleic acid amplification was negative for MTB, but positive for NTM. Therefore, the patient was diagnosed with NTM, so the patient's quarantine was lifted. After 7 days, heavy colonies with confluent growth in Ogawa's egg medium were detected in the bronchial washing fluid culture. After 2 weeks, several colonies with confluent growth in the Mycobacterium Growth Indicator Tube's egg medium were detected in the bronchial washing fluid culture. The precise species was identified using a polymerase chain reaction-restriction fragment length polymorphism-based method that identified differences in the rpoB gene.7) The colonies were subsequently identified as M. intracellulare.
To rule out metastatic lung disease, PCNA was performed on the nodule of the right upper lobe posterior segment. The lung tissue from the biospy showed chronic granulomatous inflammation with caseating necrosis (Figure 3A, B). For further evaluation, a nucleic acid amplification for MTB and NTM with a stain for acid-fast bacilli was conducted using tissue from the PCNA. The additional report showed that both the nucleic acid amplication for NTM and the stain for acid-fast bacilli were positive (Figure 3C), and there were no malignant cells. This finding was consistent with NTM infection, and we could exclude metastatic lung disease. In conclusion, the lung tissue from the biospy confirmed the diagnosis obtained from the bronchial washing fluid culture.
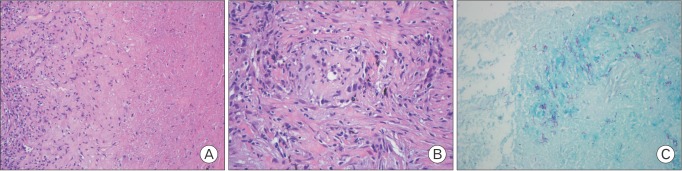
Microscopic findings of the percutaneous transthoracic needle aspiration specimens. (A) Diffuse caseous necrosis with the collection of several epithelioid cells and some lymphocytes (H&E, ×200). (B) The collection of several epithelioid cells and some lymphocytes (H&E, ×200). (C) A positive acid-fast bacilli stain was observed. Caseous necrosis with lymphocyte infiltration and positive acid-fast bacilli stain from tissue is suggestive of mycobacterial infection. The positive nucleic acid amplication for non-tuberculosis mycobacterium showed non-tuberculous mycobacteria pulmonary infection. This finding is not seen in this figure.
With the diagnosis of NTM infection, we planned to treat after differentiating the mycobacterial species. The patient was discharged after 5 days of hospitalization. The species was identified as M. intracellulare. In our outpatient clinic, the patient was prescribed a medication regimen that included rifampin (450 mg), ethambutol (800 mg), and clarithromycin (1,000 mg). A drug susceptibility test for clarithromycin was performed, and the result showed that the M. intracellulare was sensitive to clarithromycin. The patient started to complain of nausea and vomiting, and had poor oral intake 7 days after taking the medication for NTM. We changed the time for taking the medication from before meals to before bed, after which her symptoms improved. There were no other complications such as an abnormal liver function test or optic neuritis. After taking the medication, the patient has remained in good condition. We have performed blood tests and chest radiography to monitor the side effects and the disease progression.
DISCUSSION
MAC includes at least two mycobacterial species, M. avium and M. intracellulare. M. avium is the more important pathogen in a disseminated disease, whereas M. intracellulare is the more common respiratory pathogen. The chest radiography and CT scans showed abnormalities typical of the two forms of MAC lung disease. The traditionally recognized presentation of MAC lung disease is as an apical fibrocavitary lung disease with large cavities, located in the upper lobe. This form of the disease usually occurs in men with a history of cigarette smoking, excessive alcohol use, and underlying lung disease in their late 40s and early 50s. If not treated, this form of MAC is rapidly progressive within a relatively short time period, 1 to 2 years. Eventually it can cause extensive cavitary lung destruction leading to respiratory failure.
MAC lung disease also presents with bronchiectatic nodular infiltrates, usually involving the right middle lobe or the lingula segment, predominantly in postmenopausal and non-smoking women. This form of the disease has a tendency to progress much slower than the fibrocavitary disease, therefore long-term follow-ups lasting from months to years may be necessary to determine clinical or radiographic changes. In this indolent form of the disease, death may be caused by disease progression.
Fibrocavitary and bronchiectatic nodular disease are the most common types of MAC lung disease. However, other forms of MAC have been reported. SPN is identified as focal, round, or oval areas of increased opacity in the lung that measure ≤3 cm in diameter. These nodules are frequently discovered incidently on chest radiography or chest CT.8) SPN is often assumed to be attributable to MTB infection.9) However, it has been shown in case reports that SPN can be attributable to MAC lung infection.456) In 2009, Sekine et al.10) reported a case of a MAC pulmonary infection presenting with multiple nodules, which was an unusual presentation of a MAC pulmonary infection.
Unlike MTB, MAC is not an obligate pathogen. Therefore, the isolation of MAC species from a respiratory sample is not sufficient evidence of NTM lung disease. In 1997, the American Thoracic Society issued a revised set of diagnostic criteria for NTM pulmonary disease. According to these criteria, a patient with NTM lung disease must have compatible symptoms and signs, and a compatible chest radiography or chest CT abnormalities. The current case did not strictly satisfy the diagnostic criteria proposed by the American Thoracic Society in terms of radiographic findings. The diagnostic criteria of NTM lung disease must be expanded to such cases of SPN, multiple nodules, and multiple cavitary nodules, as in our case.
In our case, we could not initially rule out MTB lung infection due to the chest CT findings, which showed multiple cavitating nodules with centrinodular nodules. There was also the possibility of metastatic lung disease. We did not suspect MAC lung infection because there was neither bronchiectasis in the right upper lobe or the left lingular segment nor a fibrotic change in the upper lobe. While the bronchoscopy findings were sufficient to diagnose the patient with MAC lung infection, we also conducted a PCNA to rule out metastatic lung disease. The tissue from the PCNA confirmed NTM lung infection. In conclusion,we differentiated the atypical presentation of MAC lung infection from MTB lung disease or metastatic lung disease.
NTM have emerged as an increasingly important pathogen in the last two decades. In Korea, NTM pulmonary disease is most frequently caused by MAC. There has been an increasing prevalence of MAC infections, and an increasing number of cases presenting with atypical findings. Our case report highlights the importance of differentiating among MTB, MAC infection, and metastatic lung disease in cases of multiple cavitary nodules. Clinicians should consider the possibility of MAC lung infection with various findings on chest radiography and chest CT. We believe that PCNA can be a valuable diagnostic tool for differentiating MTB and MAC, and differentiating between malignant diseases and infectious diseases when a pulmonary nodule is revealed on chest radiography or chest CT scans.
In conclusion, to the best of our knowledge, this is a very rare report of a MAC pulmonary infection presenting with multiple cavitary nodules. As the prevalence of MAC infections increases, more cases start to show atypical radiographic findings, compared to the typical apical fibrocavitary or bronchiectatic nodular forms. Other forms of MAC have been reported, such as SPN and multiple nodules.
In this report, we present another form of MAC pulmonary infection. Therefore, clinicians should consider the possibility of MAC lung disease with various findings on chest radiography or chest CT scans. In addition, PCNA can be a useful diagnostic tool for evaluating multiple nodules to differentiate metastatic lung diseases from infectious diseases such as MTB or MAC lung infections.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.