Association between the Eating Family Meal and the Prevalence of Metabolic Syndrome Using Data from Korea National Health and Nutrition Examination Survey (2007–2012)
Article information
Abstract
Background
Several studies have shown that family meals promote a well-balanced and healthier diet and weight status. Metabolic syndrome is related to eating behavior. This study investigated the association between eating family meals and the prevalence of metabolic syndrome.
Methods
This cross-sectional study included 4,529 subjects who participated in the Korea National Health and Nutrition Examination Survey IV and V (2007–2012). A self-reported questionnaire was used to assess dietary status. Metabolic syndrome was defined according to the guidelines of the modified version of the National Cholesterol Education Program Adult Treatment Panel III. We compared the overall quality of dietary intake in family meal.
Results
Nutritional adequacy ratios for energy, protein, calcium, vitamin A, vitamin B1, vitamin B2, vitamin C, niacin, and potassium, and the mean adequacy ratio were significantly higher in the family meal group (P<0.05). The prevalence of metabolic syndrome was lower in the family meal group (P<0.05). However, we observed no significant association between eating family meals and the prevalence of metabolic syndrome.
Conclusion
This study demonstrated that eating family meals appeared to be associated with nutrient adequacy. However, we observed no significant differences in prevalence of metabolic syndrome between the 2 groups.
INTRODUCTION
In the last 60 years, Korea's rapid modernization and industrialization have westernized the country. Rapid industrialization brought about the breakdown of the family system, and led to an increase in the number of nuclear families and single households.1) According to Statistics Korea, single households constituted 9.1% of the total in 1990, 12.7% in 1995, 15.5% in 2000, 19.9% in 2005, and 23.8% in 2010. The number is predicted to reach 31.3% by 2025.2)
Family meals refer to meals eaten together with family members. The percentage of those eating family meals is decreasing annually, along with the increase in single households. Statistics Korea reported that the percentage of those eating family meals of breakfast, lunch, or dinner was 56.3%, 21.1%, and 68.3%, respectively, in 2007. The percentages fell to 46.1%, 14.4%, and 65.1%, respectively, in 2013.3)
Compared to eating alone, eating a family meal is associated with healthy dietary intake, including more fruits and vegetables, and less fried foods and carbonated beverages. Eating a family meal is also associated with higher intake of nutrients, including fiber, calcium, folate, and iron, and vitamins B6, B12, C, and E.45) Preparing meals for oneself may lead to inadequate dietary variety because of the use of fewer food ingredients and a lack of motivation to prepare high quality meals every day.6) In fact, divorced or bereaved spouses ate less vegetables compared with those who were married.78) Elderly adults who eat alone are at higher risk of nutritional deficiency, poor weight status,9) and death.10) Some studies reported that decreased frequency of eating family meals is more likely to cause overweight.11) Eating family meals was shown to be a protective factor for weight control in adolescence.12)
The prevalence of metabolic syndrome has increased significantly in Korea in the past 10 years.13) Metabolic syndrome is related to lifestyle factors such as drinking, smoking, exercise, and eating behaviors.1415) Several studies on the relationship between eating behavior and metabolic syndrome reported that higher intake of carbohydrate and lower intake of fiber were associated with an increase in its prevalence.16)
The first aim of this study is to compare the quality of dietary intake in a family meal group and a non-family meal group. Based on the hypothesis that metabolic syndrome may be related to nutrient intake, this study also investigated the association between eating a family meal and the prevalence of metabolic syndrome, using data of the Korea National Health and Nutrition Examination Survey (KNHANES) IV and V, conducted from 2007 to 2012.
METHODS
1. Study Sample
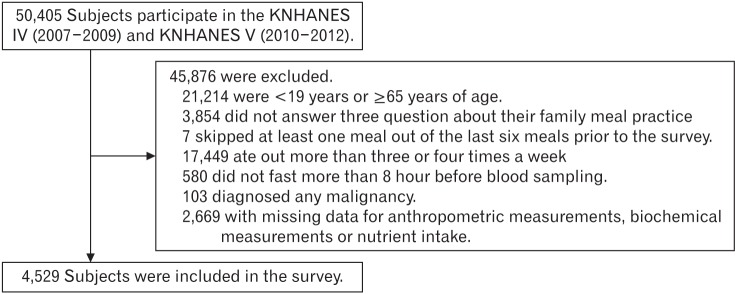
This study was based on data from the KNHANES IV and V (2007–2012). The KNHANES is a cross-sectional, nationwide survey conducted by the Korean Ministry of Health and Welfare. The KNHANES is composed of 3 sections: a health interview, health examination, and a nutrition survey. In the KNHANES IV (2007–2009) and V (2010–2012), 50,405 individuals participated in the examination. This study excluded participants younger than 19 years of age or older than 64 years of age. Those who skipped at least 1 meal out of 6 during the 2 days prior to the health examination, and those who went out to eat more than 3 or 4 times a week were excluded from this study. We also excluded subjects with missing data for laboratory tests, diet status, and nutrition intake, those who did not fast more than 8 hours before blood sampling, and those with a diagnosis of any malignancy. Finally, 4,529 subjects were included in the statistical analysis. All participants in the survey provided informed written consent (Figure 1).
2. General Characteristics of the Subjects
Physical examinations were performed by trained experts following standardized procedures. The height and body weight were measured to the nearest 0.1 cm and 0.1 kg, respectively. Body mass index (BMI) was calculated as weight (kg)/height squared (m2). Waist circumference was measured at the narrowest location between the iliac crest and the lower border of the rib cage. Systolic blood pressure and diastolic blood pressure were measured on the right arm using a standard mercury sphygmomanometer (Baumanometer; WA Baum Co. Inc., Copiague, NY, USA). Two systolic and diastolic blood pressure measurements were collected at 5-minute intervals and averaged for analysis. To assess serum levels of biochemical markers, blood samples were collected from antecubital veins after an overnight fast. Monthly income was divided into quartiles as follows: lower, lower middle, upper middle, or highest. Education level was divided into 4 groups as elementary school, middle school, high school, or university, by the subject's highest achieved level. Marital status was divided into 2 categories of single or married.
Regular drinkers were defined as individuals who drank alcohol at least once a month. Subjects who smoked cigarettes during the survey period were defined as current smokers. Regular exercise was defined as ≥20 minutes of vigorous-intensity physical activity ≥3 days a week or ≥30 minutes of moderate-intensity physical activity ≥5 days a week.17)
3. Dietary Assessment
Nutrient intake data were obtained from the nutrition survey in the KNHANES (IV–V). The nutrition questionnaire was based on the 24-hour recall method. To estimate the status of nutrient intake, the nutrient adequacy ratio (NAR) was calculated as the ratio of the age/gender-specific recommended nutrient intake or adequate intake. NAR was truncated at 1 if the value was over 1. The mean adequacy ratio (MAR) was obtained from the average NAR for 10 selected nutrients (i.e., protein, calcium, iron, fiber, niacin, and potassium, and vitamins A, B1, B2, and C.18)
4. Definition of Family Meal
The KNHANES contained the following 3 questions, to be answered yes or no: “Have you eaten breakfast with your family in the past year?”, “Have you eaten lunch with your family in the past year?”, and “Have you eaten dinner with your family in the past year?” The non-family meal group consisted of subjects who answered no to all 3 questions. Subjects who answered yes to any of the questions were included in the family meal group.
In order to prevent any error due to the combined absence of family meals and skipping of meals, those who skipped at least 1 out of the 6 meals prior to the nutrition survey were excluded. In order to avoid the confounding variable of eating out, subjects included those only who ate out no more than twice per week.
5. Definition of Metabolic Syndrome
Metabolic syndrome was defined according to the guidelines of the modified version of the National Cholesterol Education Program Adult Treatment Panel III.19) Metabolic syndrome was defined as the presence of 3 or more of the following criteria: (1) waist circumference ≥102 cm for men and ≥88 cm for women; (2) systolic blood pressure ≥130 mm Hg or diastolic blood pressure ≥85 mm Hg or taking any antihypertensive medication; (3) fasting plasma glucose levels ≥100 mg/dL or taking any antidiabetic medication; (4) triglyceride levels ≥150 mg/dL; and (5) high-density lipoprotein cholesterol levels ≤40 mg/dL for men and ≤50 mg/dL for women.
6. Statistical Analysis
Statistical analyses were performed using IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA). Continuous variables were expressed as mean±standard error and analyzed using Student t-test. Categorical variables were described as percentage of subjects and were analyzed using chi-square tests. The odds ratio (OR) and 95% confidence interval (CI) for metabolic syndrome were calculated using multiple logistic regression analysis after adjusting for sex, age, income, education, occupation, marital status, drinking, smoking, exercise, daily caloric intake, white blood cell count, and BMI. For all analyses, P-values <0.05 were considered statistically significant.
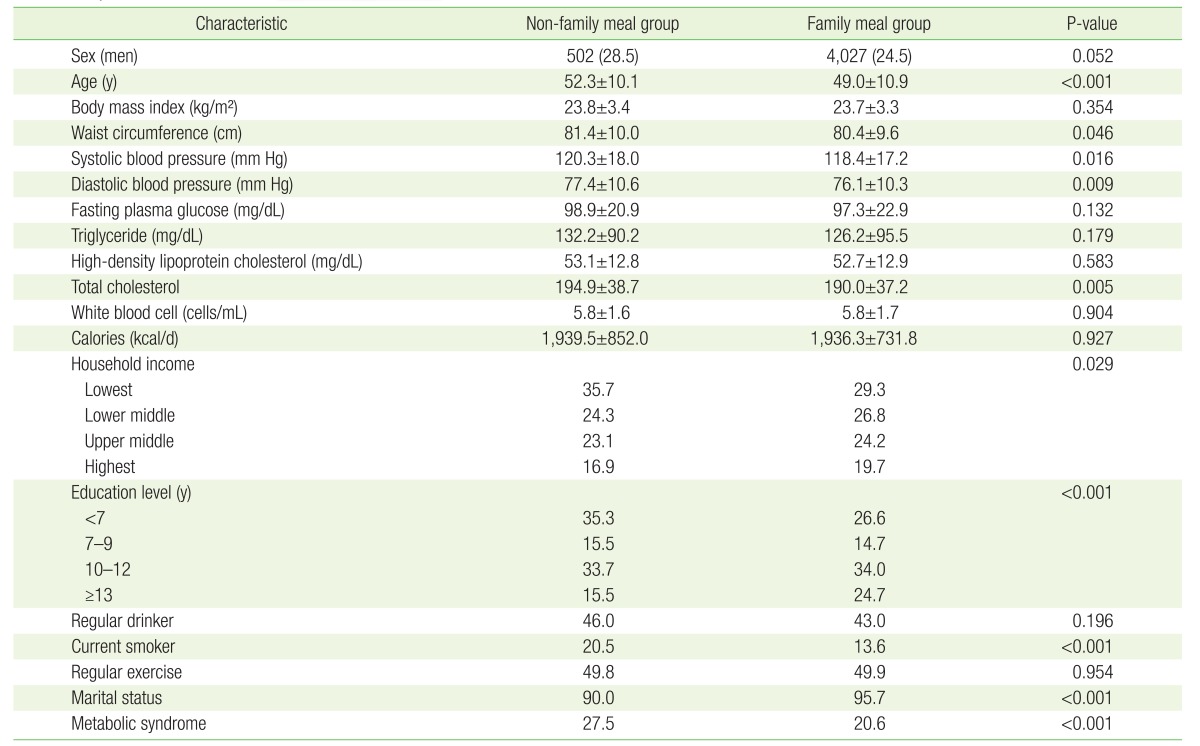
RESULTS
The average waist circumference was smaller in the family meal group (Table 1). The subjects in the family meal group showed significantly lower levels of blood pressure and total cholesterol and had a higher percentage with high income compared with the non-family meal group. In addition, individuals in the family meal group were more likely to exercise and had a lower percentage of current smokers. The percentage of those who were married was higher in the family meal group. The prevalence of metabolic syndrome was lower in the family meal group (all P-values <0.05) (Table 1).
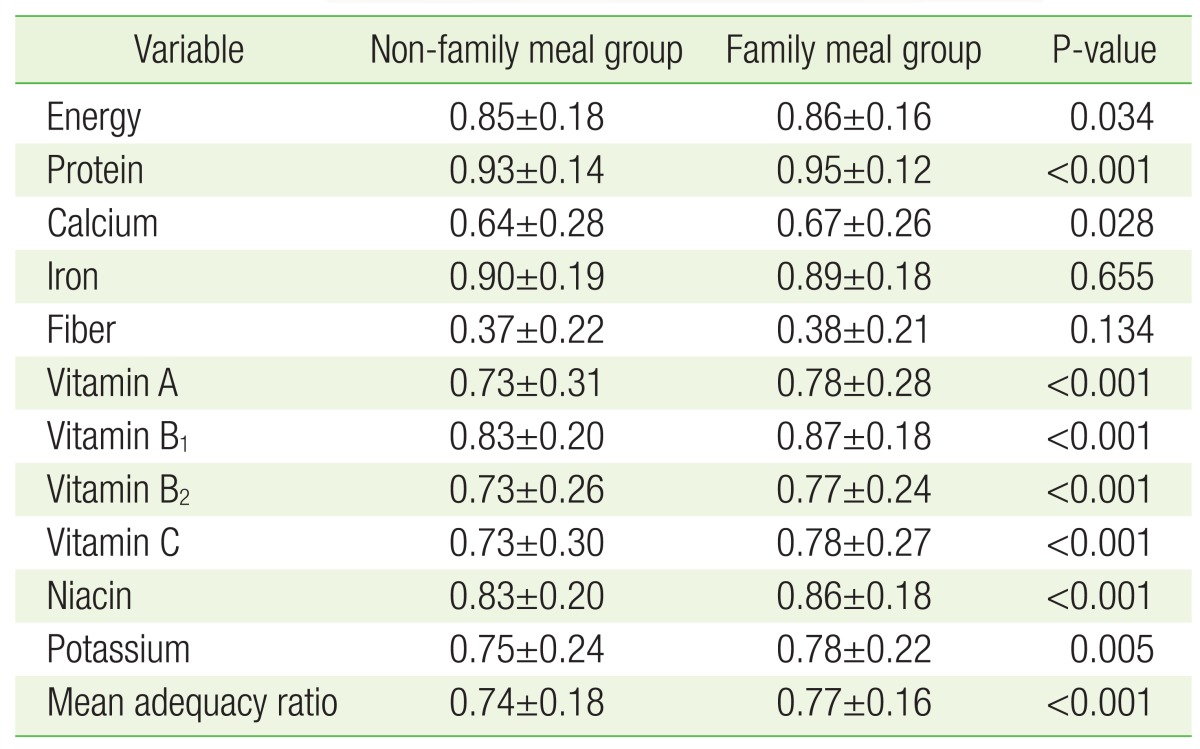
To evaluate meal quality, we compared the NAR and MAR in the family meal group and the non-family meal group (Table 2). The family meal group had more intake of energy, protein, calcium, vitamin A, vitamin B1, vitamin B2, vitamin C, niacin, and potassium, and a higher MAR (P<0.05).
In multiple logistic analysis, the OR (95% CI) for the family meal group was 0.68 (0.55–0.84) without adjusting for other variables. After adjusting for sex and age, the OR (95% CI) for metabolic syndrome was not significant in model 2 (0.82 [0.66–1.02]) (Table 3).
DISCUSSION
This study investigated the association between eating a family meal and nutritional adequacy, and between eating a family meal and the prevalence of metabolic syndrome.
The family meal group showed significantly lower measurements of waist circumference, systolic blood pressure, diastolic blood pressure, and cholesterol level. NAR was calculated to determine the nutrient adequacy. The family meal group showed significantly higher intake of energy, protein, calcium, niacin, and potassium, and vitamins A, B1, B12, and C. The MAR was also higher in this group. Therefore, eating family meals meant eating more balanced meals.
A prior study showed that higher intake of carbohydrate was associated with an increased prevalence of metabolic syndrome.16) In this study, the level of energy intake was higher in the family meal group compared to the non-family meal group. However, the OR (95% CI) for metabolic syndrome was 0.68 (0.55–0.84) in the family meal group without any adjustment, and was 0.81 (0.64–1.03) with adjustment for age, sex, income, education, marital status, drinking, smoking, exercise, daily energy intake, white blood cell count, and BMI. Therefore, in spite of higher energy intake in the family meal group, there was no statistically significant association between eating family meals and the prevalence of metabolic syndrome.
Several studies reported that higher levels of several antioxidants in serum are conversely associated with metabolic syndrome risk.2021) Individuals in the family meal group had more antioxidant vitamins compared to those in the non-family meal group. Even though eating family meals resulted in more energy intake, there were no significant differences in prevalence of the metabolic syndrome between the groups. We assumed that this may be related to the higher intake of antioxidant vitamins in the family meal group.
Our study has some limitations. First, since this study is based on cross-sectional data obtained from the KNHANES IV and V, the relationship between eating family meals and metabolic syndrome remains unclear. Second, it is highly likely that the survey participants could have given recall-biased information due to time differences between information retrieval and the actual experience. Third, the question about having family meals was formulated to find out if a participant had breakfast, lunch, and dinner during the prior 1 year. However, the question about skipping meals was formulated to find out if a participant had breakfast, lunch, and dinner for only the 2 days prior to the nutrition survey. For this reason, although only those who had all 6 meals during the 2 days prior to the nutrition survey were selected as appropriate subjects, there is insufficient evidence that subjects usually had 3 meals per day. Lastly, this study showed that subjects in the non-family meal group had many health-related risk factors that were statistically significant. Although these risk factors were adjusted in multiple logistic analysis, there is a possibility that risk factors that were not covered in this study were present.
In conclusion, this study showed that eating family meals appeared to be associated with more balanced dietary intake, and that energy intake in the family meal group was higher than in the non-family meal group, but the prevalence of metabolic syndrome was not significantly higher than in the non-family meal group.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.