General Practitioners' Perceptions on Clinical Management and Training Needs regarding the Healthcare of Community-Dwelling People with Intellectual Disability: A Preliminary Survey in Singapore
Article information
Abstract
Background
Studies worldwide indicate that people with intellectual disability have high risks of physical and mental morbidities, and poor quality of health care. This study was aimed at determining general practitioners' perceptions on barriers in clinical assessment and training needs with regard to the healthcare of community-dwelling people with intellectual disability.
Methods
A survey questionnaire was developed specifically for the study through focus group discussions and a literature review. The study was conducted as a cross-sectional anonymous survey of private general practitioners practicing in Singapore. The survey contained questions on their experience and training needs in assessing and treating patients with intellectual disability.
Results
Forty-nine of the 272 questionnaires sent out were returned. The respondents were predominantly male general practitioners working in “solo” practices. For most general practitioners, the proportion of patients with intellectual disability ranged from 1% to 5%. Nearly 90% of general practitioners identified problems in communicating with such patients as an important barrier that affected the quality of assessment of their health conditions. Other barriers identified were behavioral issues and sensory impairments. Only one-third of the general practitioners were confident that they had sufficient knowledge of physical and mental health conditions related to patients with intellectual disability. Three-fourths of the general practitioners believed that further training in this area would be beneficial.
Conclusion
Appropriate interventions to address barriers in assessment and management of patients with intellectual disability with further training for general practitioners may improve the standard of healthcare provided to this population group.
INTRODUCTION
Intellectual disability (ID), also known by various terms such as mental retardation, learning disability, or mental deficiency, is characterized by impairments in general mental abilities (intelligence quotient <70) associated with deficits in adaptive functioning. Worldwide, approximately 1% of the general population has ID.1) No population-based studies on the prevalence of ID have been conducted in Singapore. However, data from the Ministry of Social and Family Development (Enabling Masterplan 2012–2016) indicate that approximately 3% of the resident population of Singapore has some form of disability, and there are approximately 7,000 preschool children with developmental difficulties and 13,000 schoolchildren with special needs.2)
The focus of care of people with ID has shifted from institutions to the community in the past few decades, and the situation is no different in Singapore with its vision of an inclusive society.2) With the advancement in medical sciences and greater access to health care, people with ID are living longer. However, community-dwelling people with ID are well-known to have a higher risk of both physical and mental morbidities.34) Their risk of having physical health problems, especially multiple congenital abnormalities and epilepsy, may be up to 2.5 times higher than that of the general population.5) Problems with eyesight and hearing, and coronary heart disease are especially common among people with ID.36) People with Down syndrome are at a higher risk of developing hearing impairment, thyroid disorders, and Alzheimer's disease.7) In a study conducted in Singapore, the prevalences of obesity, hypertension, and dyslipidemia were found to be higher in people with ID than in the general age-equivalent population.8) A study conducted in Taiwan had similar findings of higher prevalence of hypertension and dyslipidemia in adolescents with ID.9)
The primary health care of community-dwelling people, including those with ID, depends on general practitioners (GPs).10) Patients with ID are also entitled to the same level of care as others, but significant health disparities between people with ID and the general population are well known.11) Health problems in people with ID often go unrecognized or are managed inadequately.612) Areas of health screening, prevention, and promotion in general practice care appear to be performed less frequently for people with ID than for the general population.813) Systematic health checkups have shown high rates of undetected vision or hearing loss among adults with ID.14) In Singapore, participation in health screening for cardiovascular risk factors such as diabetes and hypertension was found to be much lower among adults with ID than among the general population. Such disparities in health monitoring may have many underlying reasons, including economic burden on people with ID and their families.8) Several barriers to assessment and care of people with ID at the primary healthcare level have been identified, including communication difficulties between physician and patient, difficulties in accessing the healthcare system, poor remuneration of GPs, and short consultation time.10) Communication difficulties in people with ID can complicate the consultation process and can make both diagnosis and treatment of health problems challenging.15) GPs have been reported to often perceive that they lack the necessary skills, resources, and training to provide adequate primary care for people with ID.161718) Lack of education and training es-pecially in communicating well with patients with ID has been reported by GPs.10) A qualitative study from the United States indicated that GPs felt that they were “operating without a map" or seeing patients with ID without knowing enough; they also expressed lack of confidence or discomfort in interacting with patients with ID, and some of their anxieties involved challenging behaviors exhibited by patients with ID.19) Negative attitudes and inaccurate perceptions of GPs toward people with ID have been found in studies from the United Kingdom.20)
To date, no study has examined GPs' views with regard to the healthcare of people with ID in Singapore. Our study was aimed at determining GPs' perceptions on barriers in clinical assessment and training needs with regard to the healthcare of people with ID living in the community.
METHODS
The study was conducted as a cross-sectional anonymous survey of private GPs practicing in Singapore. Ethical approval for the study was obtained through the institutional and cluster review boards (NHG DSRB Ref: 2013/00387). A pilot survey questionnaire was developed by the study team through focus groups and information gathered through review of literature on the healthcare of community-dwelling people with ID, particularly the work of Lennox and team.10) The questionnaire was piloted on four GPs not involved in the study and was modified further in accordance with their feedback. The final version of the survey questionnaire had 14 items divided into two sections with seven statements each. The first section dealt with the physician's experience in assessing and managing patients with ID, while the second section was on the physician's training on health conditions associated with ID. Except for the final item on training, the questionnaire followed a 5-point Likert response format with options of “strongly agree,” “agree,” “neither agree nor disagree,” “disagree,” and “strongly disagree,” so that GPs could indicate their level of agreement or disagreement with a given statement. The final item on training on health conditions associated with ID listed potential topics of interest from which the respondents could choose multiple options. The questionnaire also had sections on demographic and practice characteristics of GPs.
1. Study Population
Initially, we included all the GPs (n=72 at the time of the study) enrolled in the Mental Health-General Practitioner Partnership Program (MH-GPPP).21) MH-GPPP was established by the Institute of Mental Health, Singapore, as a partnership program with GPs to focus on its objectives of providing liaison specialist services and to identify and train GPs with competencies to treat mental illness in the community. GPs under this program received some training on mental illnesses such as schizophrenia and depression but did not receive training on health care of patients with ID. Later, another 200 GPs were randomly selected from a database of GPs in Singapore. Overall, 272 GPs were selected as the target study population.
Survey questionnaires were sent to the participants by post. Each survey questionnaire had a cover letter with a brief description of the study and study enrolment details. The questionnaire and the return envelopes did not have any identifiers to ensure anonymous return of survey forms. A follow-up telephone call was made to each GP/practice after 2 weeks to check if the GP/practice had responded to the questionnaire. Names of GPs who had not responded at the end of 2 weeks (on telephone enquiry) were noted, and a further telephone reminder was given to all of them after 4 weeks.
2. Analysis
To allow greater clarity in analysis and presentation, responses to the items of the survey questionnaire were modified as follows: “strongly agree” and “agree” responses were clubbed together as “agree,” while “disagree” and “strongly disagree” responses were clubbed together as “disagree.” The “neither agree nor disagree” responses were left unchanged. For the analysis of demographic data and responses to statements, descriptive statistics was used. Chi-square tests were used to compare differences in responses with regard to sex, years of experience, and type of practice of GPs. All statistical analyses were performed using PASW SPSS Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
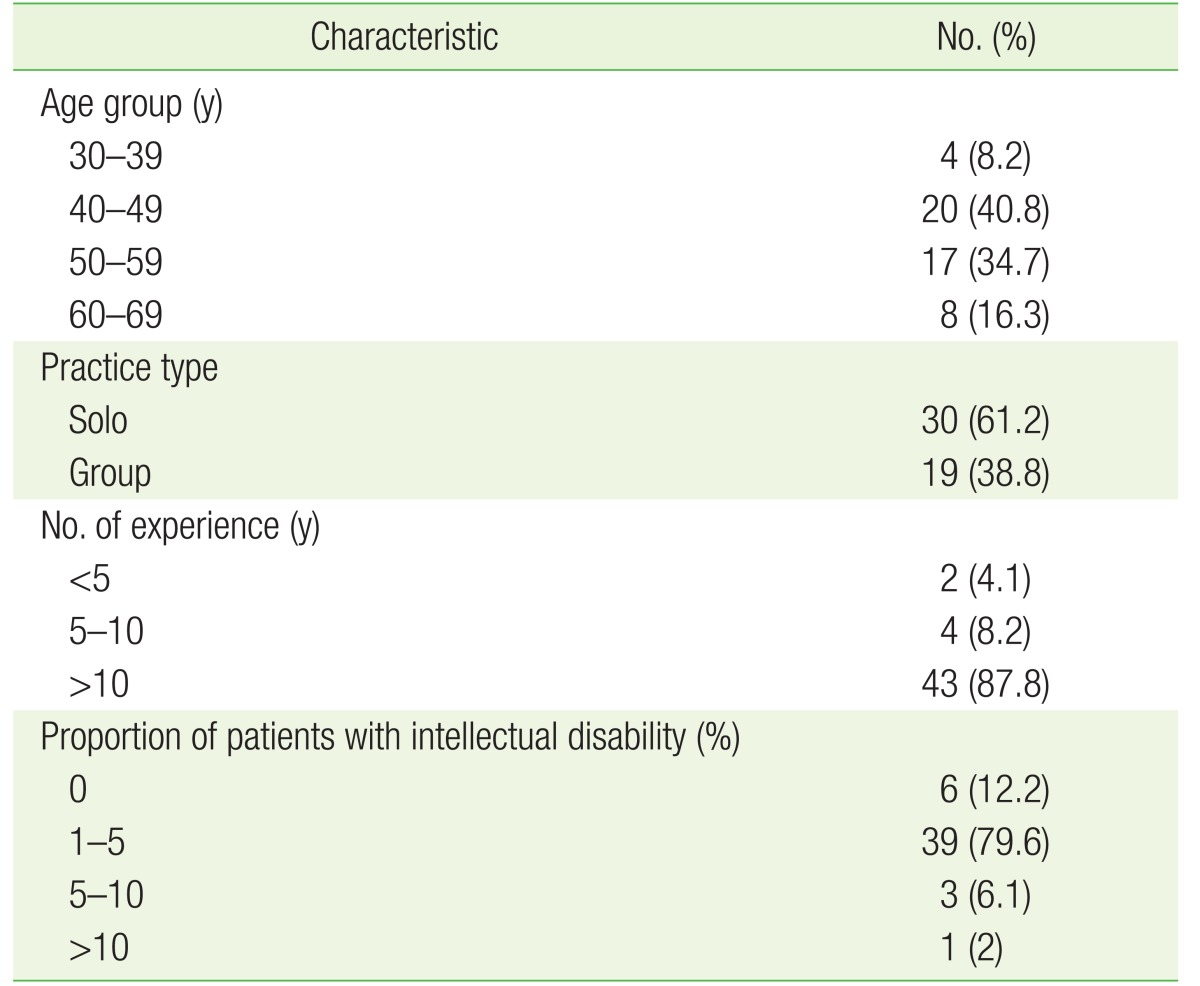
Forty-nine of the 272 questionnaires sent out were returned, resulting in a response rate of 18.01%. Twenty-nine (59.2%) of the GPs who responded were men. The mean age of the respondents was 50.29 years (range, 33 to 66 years; median, 50.0 years; standard deviation [SD], 8.52). The mean number of years of experience of the GPs in clinical practice was 21.25 years (range, 2 to 35 years; median, 22 years; SD, 8.71). The rest of the demographic and practice characteristics of the GPs are given in Table 1.
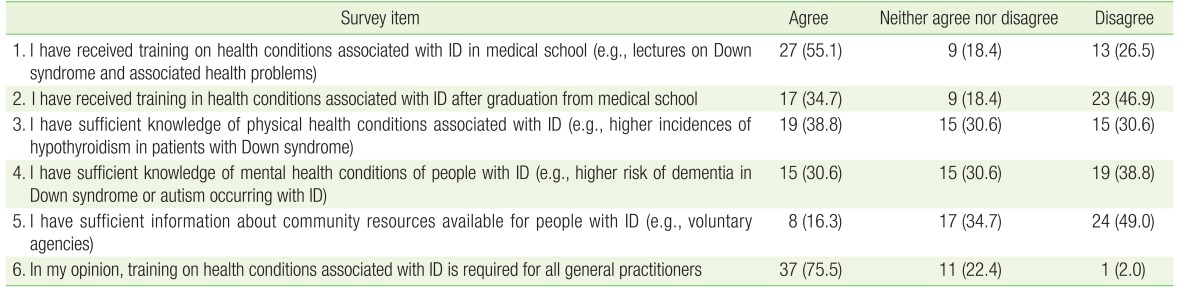
Responses with regard to GPs' experiences in assessing and managing people with ID are given in Table 2. Responses with regard to training on health conditions related to ID are given in Table 3.
To the final statement in the questionnaire, “If training is available on health conditions in patients with ID, I will be keen to attend, ” responses indicated that 89.8% (n=44) of GPs were keen to attend such training if available. Topics chosen for training in descending order of preference were “mental health conditions in ID” (79.6%), “autism” (75.5%), “physical health conditions associated with ID” (73.5%), and “community resources” (61.2%). Comparison of responses to survey items with sex, age group, or length of experience of GPs was not statistically significant. With regard to the type of practice (solo versus group), a significant difference was found in responses to only one statement; all the 9 GPs (18.4%) who “agreed” that they preferred not to treat patients with ID were from solo practice.
DISCUSSION
This is the first survey of GPs in Singapore to examine the barriers in clinical assessment and training needs with regard to the healthcare of people with ID living in the community. The response rate in our survey was relatively low (18.01%) but was comparable with that (25%) in a previous postal survey of GPs on the healthcare issues in Singapore.22) Although this low response rate makes generalization of findings difficult, several important areas in relation to the assessment and management of patients with ID by GPs and their training needs were clearly identifiable.
Respondents of this survey were predominantly male GPs (nearly 60%) with a mean age of 50 years. Most GPs were working in solo practices and had substantial length of experience in clinical practice. These findings were comparable with the results of previous surveys of GPs in Singapore.2223) The proportion of patients with ID constituted 1% to 5% of the overall patient population for most GPs who responded to the survey. This indicates that patients with ID constitute only a minor part of their work, which might make GPs less confident or inexperienced in dealing with these patients over time.
The responses from GPs to statements on difficulties in communication with patients and their caregivers, and other barriers to assessment and management of patients with ID, such as behavioral issues and sensory impairments, confirm that GPs have substantial difficulties in these areas. Nearly 90% of the GPs who responded identified problems in communicating with patients with ID as an important barrier that significantly affected the quality of assessment and treatment of the patients' health conditions. These findings are similar to those from surveys of GPs on barriers to assessment of patients with ID in other countries.1024) Solutions to such barriers may involve strategies such as increasing the length and frequency of consultations, developing reminder cards for health screenings or reviews, and providing education to individual patients and their caregivers so that they can more proactively seek appropriate health care.825) Having the same physician to see the patient every time and the presence of a familiar caregiver who can reassure the patient during physical examination can play a huge role in improving the quality of examination of a patient with ID by a GP.
While almost all GPs agreed with the principle of equal entitlement of good quality care for patients with ID as others, some GPs (18.4%) preferred not to treat people with ID, while 26.5% of the responders were unsure of this. Although our survey did not identify the reasons behind such attitudes, this may be a reflection of their lack of confidence in assessing and managing such patients, or personal prejudices against people with ID. Negative attitudes of GPs toward people with ID are not unknown, and such attitudes may influence the quality of healthcare provision for this population group.626) The finding that the GPs who “agreed” that they did not prefer to treat patients with ID were all from solo practice settings, may indicate the limited facilities or support that GPs have while working in such settings. Education of GPs to reduce misconceptions about ID and providing appropriate compensation and facilities for those attending to patients with ID may help to change this predicament. Financial incentives from the National Health Service in England for GPs who conduct annual health checkups for people with ID have been found to improve healthcare services provided to this population.27) No such programs have been implemented in Singapore. Surprisingly, only 49% of the GPs confirmed that they had facilities for people with disability and mobility issues in their practice. Such facilities will likely improve in the future with the government's push for inclusion of and accessibility for people with disabilities in Singapore.2)
Statements on training and knowledge in the survey mainly assessed GPs' self-assessment of their training and level of confidence in assessing and managing patients with ID. Although nearly 55% of GPs had received some form of training on health conditions related to ID as an undergraduate, only a few received training later. Only one-third of GPs were confident that they had sufficient knowledge of the physical and mental health conditions of patients with ID. The percentage of GPs with information on community resources available for people with ID was even lower (16.3%). These finding are not unique to Singapore. In a similar survey of GPs in Australia, only one-quarter of GPs felt adequately trained in ID and only 10% received any postgraduate training in ID.10) Three-fourths of GPs in our survey believed that training on health conditions related to ID would be beneficial for all GPs and were keen to choose multiple topics, including mental and physical health conditions, autism, and community resources. Acknowledgment of the need for further training for GPs on health conditions related to patients with ID has been a recurrent theme in similar surveys conducted in other countries.102428) Evidence exists that increasing the knowledge of health providers on health issues in patients with ID, especially the need for vigilant health monitoring, might improve the health status of this population.29) GPs' increased understanding of the health-risk factors associated with specific disabilities and other system factors that contribute to health disparities between people with ID and the general population might ameliorate or prevent the high rates of morbidity and mortality in this population.11) Canada and Aus-tralia have developed guidelines and practical recommendations to inform primary-care providers about the health needs of people with ID and the best approaches to management.730) It is important that GPs are supported in improving their confidence and expertise in assessment and management of patients with ID, and similar guidelines and recommendations may be helpful for GPs in Singapore as well. Partnerships between mental health professionals/institutions and GPs such as MH-GPPP,21) and liaison between GPs and social sectors are steps in the right direction.
Our survey had a relatively low response rate, and owing to the limitations of the study design, identification and follow-up of non-responders were not possible. Moreover, in our survey, nearly one-fourth of the target study population had close liaison with mental health services through MH-GPPP, while the rest were selected randomly. As the survey was conducted in anonymously, we were not able to identify the differences in response rate or views between the groups. However, as the practice settings of these two groups were not dissimilar and as the GPs under the MH-GPPP did not receive any specific training on healthcare of patients with ID, it was unlikely that their responses would be significantly different from each other. Our study was limited to private GPs, and responses of GPs working in polyclinics under the public healthcare system in Singapore may differ from those of GPs in this survey.
In summary, our study was a preliminary attempt to understand the barriers that GPs face with regard to assessment and management of community-dwelling people with ID and their training needs. The findings of this survey point to the presence of several barriers for GPs in this area and call for appropriate interventions to address them. In addition, targeted training opportunities for GPs could improve the standard of health care provided to people with ID in the community. Further large-scale studies are required to confirm our findings.