The Association between Cancer Screening and Cancer History among Korean Adults: The 2010–2012 Korea National Health and Nutrition Examination Survey
Article information
Abstract
Background
Cancer survivors are at a higher risk of primary cancer recurrence and development of second primary cancer. In both cases, early disease detection is crucial. This cross-sectional study assessed cancer screening participation rates according to cancer history.
Methods
Data were obtained from the 2010–2012 Korea National Health and Nutrition Examination Survey for 12,500 participants. Of these, 624 cancer survivors were enrolled in this study. Sampling weights were applied to maintain the representativeness of the Korean adult population.
Results
Overall 2-year cancer screening rates prior to the survey in male and female cancer survivors were 59.9% and 73.7%, respectively, while opportunistic cancer screening rates were 33.5% and 52.1%, respectively. The odds ratios (95% confidence interval) of the overall cancer screening among the cancer survivors, compared to others, were 1.16 (0.79–1.72) in male and 1.78 (1.20–2.63) in female participants, after the adjustment for confounding variables. The odds ratios (95% confidence interval) for opportunistic cancer screening and National Cancer Screening Program among cancer survivors were 1.56 (1.07–2.27) and 0.80 (0.53–1.21) in males and 2.05 (1.46–2.88) and 0.66 (0.46–0.95) in females.
Conclusion
Female cancer survivors showed a higher rate of overall and opportunistic cancer screening than did the male cancer survivors. Further efforts are required to improve cancer screening among male cancer survivors.
INTRODUCTION
In 1986, the National Coalition for Cancer Survivorship in the United States established the definition of a cancer survivor as any person diagnosed with cancer from the time of initial diagnosis until death [1]. Worldwide, the number of cancer survivors continues to increase. In Korea, there are approximately 1.6 million cancer survivors [2], with over 30 million survivors worldwide [3].
Important concerns for cancer survivors are disease recurrence or metastasis of primary cancer, the development of second primary cancer, and treatment-related adverse effects. A previous study based on cancer registry data showed that cancer survivors faced a 1.1- to 1.6-fold higher risk of a second primary cancer than that of the general population [4]. In the United States, one in six of all incident cancers are diagnosed in cancer survivors, with second primary cancers as a leading cause of mortality among cancer survivors [5]. In survivors achieving relatively good prognosis for the initial primary cancer, a second primary cancer is likely to be the direct cause of death. The increased health risk stems from cancer itself, in addition to lifestyle; genetic susceptibility; environmental factors, such as health service accessibility; and the late carcinogenic effects of chemotherapy and radiation therapy [6]. To reduce cancer-related mortality, careful observation of primary cancer recurrence and second primary cancer is an essential component of the follow-up care of cancer survivors [7]. In Korea, little is known about cancer screening practices among cancer survivors, and neither evidence-based guidelines nor a proper management system for these patients has been established. However, it is well-accepted that ongoing, long-term cancer screening is essential.
The present study aimed to investigate whether a higher rate of cancer screening is evident in cancer survivors than in individuals without a history of cancer. Moreover, we examined the association between a history of cancer and participation in organized versus opportunistic cancer screening.
METHODS
1. Study Designs and Participants
The 2010–2012 Korea National Health and Nutrition Examination Survey (KNHANES) was conducted as a population-based cross-sectional survey that is designed to assess the health-related behavior, health condition, and nutritional status of Koreans. All health examination components were conducted in a local hospital or at mobile examination centers that traveled to each survey location. The field operation team consisted of a doctor, nurse, radiological technician, interviewer, and dietitian, all of whom followed standardized protocols. The sampling units were households selected using a stratified, multistage, probability sampling design according to the geographic area, sex, and age group, based on household registries. Participants who agreed to participate in the study provided written informed consent [8].
This present study utilized the data from 25,534 individuals who participated in the 2010–2012 KNHANES. Individuals younger than 40 years (n=11,873) and nonresponders regarding cancer diagnosis (n=140) and cancer screening (n=1,021) were excluded from the study. Thus, the final study population consisted of 12,500 participants (5,369 males and 7,131 females), including 624 cancer survivors (229 male and 395 female survivors).
All participants provided written informed consent and were given the right to refuse to participate according to the National Health Enhancement Act. This study was approved by the Institutional Review Board of the Korea Centers for Disease Control and Prevention.
2. Definition of Health-Related Behavior and Socioeconomic Status
Body mass index (BMI) was calculated as the ratio of the individual’s weight in kilograms to his or her height in meters squared (kg/m2).
Health-related behaviors and lifestyle information were evaluated using a self-reported questionnaire administered during each survey period. Daily calorie intake was assessed using a 24-hour food recall method. Smoking status was classified as never smoker, former smoker, and current smoker. Participants who smoked cigarettes during the relevant survey period were defined as current smokers. “At-risk” drinking was screened using the Alcohol Use Disorders Identification Test (AUDIT), which consists of three domains: hazardous alcohol use, dependence symptoms, and harmful alcohol use. Participants who engaged in the vigorous-intensity physical activity at least 3 days a week and/or moderate-intensity physical activity or walking at least 5 days a week were part of the regular physical activity group. Participants with chronic diseases were those who answered “yes” to the question “Have you ever been clinically diagnosed with hypertension, dyslipidemia, diabetes, or cardiovascular/cerebrovascular disease?”
Participants were also asked to respond to open-ended questionnaires that included the following question: “What is your average monthly income including salary, property income, pension, government subsidies, and allowance?” Marital status was defined as married and not separated (currently married and living with his or her spouse), single (either not married, previously married but now separated, widowed, or divorced), or nonresponders (a participant who did not respond). Educational level was classified into four categories: elementary school or less, middle school, high school, and college or more. Occupational status was categorized into three groups: (1) manual worker; clerk; service or sales worker; skilled worker in agriculture, forestry, or fisheries; an operator or assembler of vehicles, boats, or planes or of equipment and other machinery; and factory workers; (2) office worker, manager, professional, and administrator; and (3) others, defined as unemployed, housekeepers, and students. Urban residents were defined as individuals who live in the metropolitan regions of cities. Insurance type was categorized as national health insurance (regionally insured and workplace insured) and public assistance (medical aid and essential livelihood protection).
3. Definition of Cancer Survivors and Cancer Screening
Cancer survivors comprised those who answered “yes” to “Have you ever experienced any cancer or malignancy in your lifetime?” Those who answered “no” were assigned to the non-cancer group.
Participants were also asked the following question: “Have you undergone cancer screening any time within the last 2 years?” Participants who answered “yes” were further questioned about the type of cancer screening. Cancer screening was recategorized as opportunistic or via the National Cancer Screening Program (NCSP) according to the funding source of screening. Participants were included in both groups if they answered that they had received both tests. Opportunistic cancer screening was defined as cancer screening in which the examinee, his or her acquaintances including their family, or employer paid the cost for an examination performed in either the private healthcare sector, such as private general hospitals, clinics, and health checkup centers. The NCSP offers free cancer screening via the Korean National Health Insurance Corporation or at public health centers.
4. Data Management and Statistical Analysis
Data obtained from the 2010–2012 KNHANES were considered to represent the standard population. We applied sampling weights to each participant’s data to ensure that the dataset represented the entire Korean population without biased estimates. Continuous variables were presented as a means±standard error (SE), and categorical variables were described as weighted frequencies±SE.
General linear models and χ2 tests were used to compare the means of continuous variables and the frequencies of categorical variables according to cancer history by sex. Odds ratios (ORs) and corresponding 95% confidence intervals (95% CI) for cancer screening among cancer survivors were calculated using multivariate survey logistic regression analyses. The statistical analyses were performed using SAS statistical software ver. 9.4 (SAS Institute Inc., Cary, NC, USA). Differences were considered significant at values of P<0.05 [8]. All statistical tests were two-tailed.
RESULTS
The general characteristics of all study participants are shown in Table 1. The mean age was 54.9 years for males and 56.7 years for females. The percentages of male and female cancer survivors were 3.2% and 5.1%, respectively. The 2-year participation rates for overall cancer screening were 56.6% for males and 60.8% for females.
Table 2 shows the participants’ characteristics according to cancer history. Cancer survivors were older and less likely than individuals without a history of cancer, to be alcohol consumers (all P-values <0.001). Male cancer survivors exhibited lower BMI and fewer current smokers than males without a cancer history. Female cancer survivors showed a higher rate of chronic disease than females without a history of cancer. The percentages of overall cancer screening within the last 2 years in the non-cancer group and the cancer survivors were 56.5% and 59.9% for males (P=0.437) and 65.4% and 73.7% for females (P=0.006). Female cancer survivors were more likely to receive cancer screening than females with no history of cancer. According to the type of cancer screening, female cancer survivors were more likely to participate in opportunistic cancer screening but less likely to use the NCSP, and this was not observed in male cancer survivors. The percentages of opportunistic cancer screening in the non-cancer and cancer survivor groups were 30.3% and 33.5% for males (P=0.410) and 38.6% and 52.1% for females (P<0.001), respectively. The percentages of individuals who underwent NCSP screening were 27.0% and 28.1% in males (P=0.749) and 30.5% and 24.4% in females (P=0.033), respectively.
Table 3 presents the multivariate logistic regression results for the overall screening of cancer survivors after adjusting for confounding factors. Compared to the non-cancer group, the age-adjusted ORs (95% CI) for overall cancer screening within the last 2 years among cancer survivors were 1.06 (0.74–1.52) for males and 1.62 (1.22–2.14) for females. After adjusting for age, BMI, daily calorie intake, marital status, socioeconomic status (including educational and occupational status and household income), residence area, and insurance type in model 2, the ORs (95% CI) for overall cancer screening among cancer survivors were 1.18 (0.81–1.72) for males and 1.59 (1.19–2.13) for females. After fully adjusting for lifestyle factors such as smoking status, AUDIT score, physical activity, and chronic diseases in addition to the factors in model 2, the ORs (95% CI) were 1.16 (0.79–1.72) for males and 1.78 (1.20–2.63) for females (model 3). Female cancer survivors were more likely to have undergone cancer screening within the last 2 years than females with no history of cancer.

Multivariate-adjusted odds ratios and 95% confidence intervals for cancer screening within 2 years among cancer survivors compared to individuals without a history of cancer (non-cancer)
To further examine the association between a cancer diagnosis and cancer screening type, logistic regression analyses were performed after stratifying overall cancer screening by opportunistic screening and NCSP screening (Figure 1). Compared to the non-cancer group, the ORs (95% CI) for opportunistic cancer screening among cancer survivors were 1.56 (1.07–2.27) for males and 2.05 (1.46–2.88) for females. On the contrary, female cancer survivors were unlikely to make use of the NCSP (0.66 [0.46–0.95]).
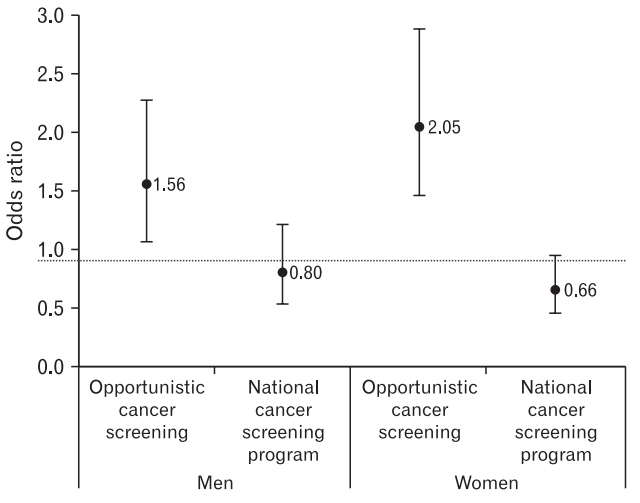
Odds ratios for cancer screening of cancer survivors compared to individuals without a history of cancer. Adjusted for age, body mass index, daily calorie intake, household income, marital status, years of education, occupational status, residence area, insurance type, smoking, Alcohol Use Disorders Identification Test score, physical activity, and chronic diseases, including hypertension, dyslipidemia, diabetes, and cardiovascular/cerebrovascular diseases.
DISCUSSION
The results of this cross-sectional study showed that female cancer survivors were more likely to undergo overall cancer screening than females without a history of cancer, after controlling for age and other confounding factors. However, this difference was not observed in male cancer survivors. Stratification of overall cancer screening by opportunistic and NCSP-based screening showed that both male and female cancer survivors were more likely to choose opportunistic cancer screening. For female cancer survivors, the OR for participating in the NCSP was relatively low.
Cancer is the leading cause of death in Korea [9], and its detection and management at an earlier, precancerous stage would lower mortality [10,11]. Screening for cancer or a precancerous lesion is the most effective method for early disease diagnosis and results in better prognostic outcomes. To reduce the burden of malignant diseases, since 1990, Korean health authorities have provided free cancer screening via the NCSP for the five major cancers (stomach, colorectal, liver, breast, and uterine cervix) for individuals aged greater than 40 years [12]. In the private sector, many individuals undergo opportunistic cancer screening through health checkups. As a result of national and personal efforts in early detection and intervention, the 5-year relative cancer survival rate increased from 41.2% in 1993–1995 to 69.4% in 2009–2013, according to the “cancer facts and figures 2015” in the Republic of Korea, published by the National Cancer Information Center [13].
Cancer survivors are at higher risk for not only recurrence of primary cancer but also a second primary malignancy and comorbidities such as cardiovascular diseases and diabetes. These susceptibilities are attributed to genetic factors, behavioral risk factors, and previous anticancer treatment, including chemotherapy and radiotherapy [14]. Multiple cancers involving different organs can arise from deletions or mutations in oncogenes and tumor suppressor genes. Previous studies showed that breast cancer survivors have a fourfold higher risk of contralateral breast cancer [15,16]. In colorectal cancer survivors, due to the risk, as previously mentioned, a careful evaluation of synchronous and metachronous colorectal cancers has been recommended [17].
After analyzing the 2001, 2005, and 2007 KNHANES data, Cho et al. [18] reported that cancer survivors are more likely to obtain cancer screening than the non-cancer population. Schumacher et al. [19] reported that in a US population, female cancer survivors recorded higher screening rates for cervical and breast cancer than individuals with no history of cancer. According to a Canadian study, Grunfeld et al. [20] found that breast and endometrial cancer survivors were more likely to be screened than the controls. Our results are consistent with those previously reported studies, but in all of those cases, the focus was on the primary cancer type or site-specific cancer screening, with no consideration of differences in payment among cancer survivors and various control groups. Our study showed that male cancer survivors are less likely than their female counterparts to participate in overall cancer screening but were more likely to undergo opportunistic cancer screening than were males without a previous cancer diagnosis. Female cancer survivors were more likely than the non-cancer population to participate in overall cancer screening, especially opportunistic screening, and less likely to use the NCSP. The more careful cancer screening by female survivors may in part explain their higher 5-year relative cancer survival rate compared to male survivors (78.2% versus 62.2%, respectively).
Because this study could not confirm the date of the screening test, it is possible that participants did not receive the NCSP because they received opportunistic screening.
Previous studies reported that barriers hindering participation in NCSPs include less trust in these programs and a lack of awareness of the existence and importance thereof [21]. Indeed, there is a gap between the current performance of the Korean NCSP and the Korean cancer screening guidelines published in 2015 by the National Cancer Center regarding the seven most common cancers [2]. Health authorities should focus their efforts on policies to remove these barriers and to increase trust and awareness of the NCSP, such as providing better information on the necessity of cancer screening. Moreover, the quality of screening by healthcare centers and access to trustworthy medical facilities should be improved. Limited healthcare resources should be adequately redistributed to those populations most in need of medical services. In one study, few cancer survivors were recommended by their physicians to undergo screening for second primary cancer, and few had adequate information regarding cancer screening [12]. Recommendations for regular health checkups should be mandatory, in addition to educating cancer survivors, especially males, on the importance of cancer screening. Efforts at the national and the personal level can improve treatment outcomes in patients with primary cancer and will improve the detection of second primary cancers at an earlier stage, thus reducing the socioeconomic burden on the rest of society.
Our study had several limitations. First, we could not confirm our conclusion that cancer survivors are more likely to undergo cancer screening because of the cross-sectional design of our study. Individuals concerned about their health tend to undergo more regular health checkups, introducing a risk of overdiagnosis of cancer. However, regardless of the association between cancer survivors and screening rates, all physicians should recommend routine screening for these patients based on practice guidelines. A second limitation was the potential misclassification of some participants, as cancer screening was self-reported using a questionnaire.
Additionally, some cancer survivors might have confused a periodic follow-up after anticancer treatment as active second primary cancer screening [12]. Third, the cancer type, nature of the screening units, and methods used were neither identified nor differentiated. We also did not discriminate between a recent versus a non-recent cancer diagnosis. The methods of cancer screening may be different depending on the type and timing of cancer diagnosis. However, further analysis was not performed because it is thought that the number of each group is small to be analyzed. We are considering further study using the data from 2012 onward.
Despite these limitations, this study has several strengths. It examined the association between cancer history and cancer screening based on the nationally representative 2010–2012 KNHANES data. Sampling weights were applied to all analyses to ensure that the results were representative of the general Korean population. Additionally, overall cancer screening was stratified as either opportunistic cancer screening or NCSP-based screening, which allowed us to discriminate between users of the public versus private healthcare system.
In conclusion, this study showed that all cancer survivors exhibit higher rates of opportunistic cancer screening than non-cancer patients. Moreover, female, but not male, cancer survivors are more likely to participate in overall cancer screening, although female cancer survivors are less likely to participate in the NCSP. These results highlight the need for greater participation of male cancer survivors in cancer screening, for improvements in the NCSP, and for increased public awareness of the national screening program. Health authorities should develop cancer policies that ensure better distribution of their limited resources to those individuals and healthcare units most in need. Finally, access to adequate cancer screening by cancer survivors requires that healthcare professionals establish appropriate evidencebased and cost-effective guidelines.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
The KNHANES was conducted by the Korea Ministry of Health and Welfare in 2010–2012. We thank all of those who attended the KNHANES and all of the participants in this survey.


