The Effect of Trigger Point Injections on Pain in Patients with Advanced Cancer
Article information
Abstract
Background
It has been reported that in 62.5% of cases of incurable cancer pain, the complaint is due to myofascial pain syndrome. Trigger point injections using dibucaine hydrochloride help patients with such cancer pain. This study evaluated the efficacy of trigger point injections for alleviating pain in patients with advanced cancer.
Methods
Twenty patients with advanced cancer who had a life expectancy of 6 months or less and had been diagnosed with myofascial pain syndrome were treated with trigger point injections. Prior to treatment, a Visual Analog Scale (VAS) was used to measure the resting pain level and discomfort upon application of pressure on the site of pain. These values were compared with last treatment measurements.
Results
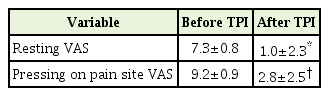
The mean pre-treatment VAS scores for pain at rest and upon application of pressure on the pain site were 7.3 and 9.0, respectively. These scores decreased significantly to 1.95 and 3.2, respectively, after the treatment (P<0.05).
Conclusion
Trigger point injection is an alternative and effective pain control modality for advanced cancer patients with myofascial pain syndrome.
INTRODUCTION
Myofascial pain syndrome is a condition characterized by an area of muscle with hypersensitive response, called a trigger point, which can cause pain, muscle weakness, limited range of motion, symptoms of autonomic nervous system mismatch, depression, and insomnia among other symptoms. Trigger points are regions of tender muscle fibers (taut bands) in skeletal muscle that can evoke major pain [1,2].
The pain caused by cancer is extensive, and some forms are resistant to even opioid medication. Among incurable cancer pain, one investigation reports that 12%–17% of cancer patients complain of pain and of those 62.5% are experiencing myofascial pain syndrome. Everyone has experienced functional muscle pain in their daily lives, but cancer patients can experience sustained episodes of such pain [3]. Myofascial pain syndrome was observed in one out of nine patients treated for cancer in the head and neck, and a decreased quality of life was observed among these patients [4]. In a previous study, 84.9% of cancer patients reported their response to trigger point therapy using Neovitacain injection for myofascial pain as ‘good’ or ‘better’ and Visual Analog Scale (VAS) scores also improved [5].
This study aimed to evaluate the effect of trigger point injections on the advanced cancer patient with cancer pain.
METHODS
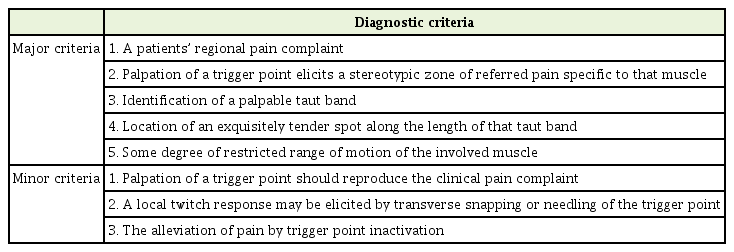
The study enrolled a total of 20 advanced cancer patients in hospice care. They were able to verbally express their pain levels and their presumed life expectancy was approximately 6 months or less. Procedures were conducted only on those patients who agreed to receive trigger point injections after receiving sufficient explanation regarding the treatment. Trigger points were determined using the diagnosis criteria of Simons (Table 1) [6]. Patients prone to bleeding or infection were excluded. Details of previous or current medications and remedies intended for pain control were recorded during the assessment period.
A physical examination was conducted to check for trigger points, and suspected areas were injected with 1 to 4 mL of lidocaine depending on the size of the muscle [6,7]. Based on another study, the average number of injections was 2.4 and 3.7 at the time of evaluation, so we estimated the efficacy after the fourth injection [5]. In our study, the treatment was limited to one or two injections per week. And maximum injections of times were limited of four injections, if initial two injections were effective. When the administration was terminated before the final injection, the evaluation was performed at that time point or the next treatment day. Pain levels were compared between before and after injections using a 100-mm VAS scale for pain at rest and pain upon application of pressure to the trigger point.
The collected data was analyzed by IBM SPSS statistics ver. 20.0 program (IBM Corp., Armonk, NY, USA). The VAS of the pain before and after trigger point injections was considered to be statistically significant when the P-value was less than 0.05 using the Wilcoxon signed-rank test, a nonparametric test of two related samples.
This study was reviewed and waived by the Institutional Review Board, and it complied with the Declaration of Helsinki. And written informed consents were obtained from patients.
RESULTS
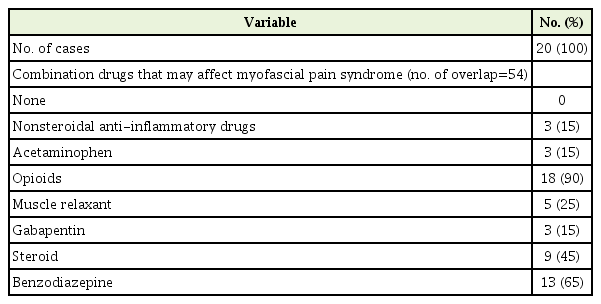
Within the study group, there were 16 males (80%) and four females (20%). The participants included two patients in their 60s (10%), 15 in their 70s (75%), and three in their 80s (15%); the mean age was 74.2 years. The most common primary diseases were cancer of the gastrointestinal tract (30%) followed by pulmonary cancer (25%). The most common pain complaints were ‘severe pain’ (50%) followed by ‘moderate pain’ (30%). The areas of pain to be evaluated included: the ‘thoracolumbar area’ (41.6%) and the ‘neck and shoulder area’ (33.3%) (Table 2). In regards to medication combinations used for myofascial pain syndromes, 90% of patients had used opioids, followed by benzodiazepines (65%) and steroids (45%) (Table 3).
The VAS at rest before and after injections decreased from 7.3 to 1.95 (P-value <0.001). The VAS with pressure applied to trigger points before and after injections decreased from 9.0 to 3.2 (P-value <0.001) (Table 4). Thirteen patients (65%) improved immediately after injections, while five patients (25%) improved within 3 days, and two patients (10%) had no improvement after injections. None of the patients experienced increased or worsened pain. Pain improvement was only assessed at the injection site and the affected area of the injected muscle, though many patients had decreased pain in other areas. For example, after injections in the cervical area, pain in forearm also improved. These results were excluded from the analysis because causality is difficult to prove. If there was no response after the first and second injections, no additional treatments were performed. There were five patients whose symptoms such as nausea, vomiting, depression, and insomnia, unrelated to pain after injection, improved at the same time. Three patients (15%) complained of pain at the injection site for 1 to 2 days after the injections, but no other side effects were noted. Pain and swelling at the site of injection were self-limiting.
DISCUSSION
Myofascial pain syndrome is a pain syndrome caused by muscle and fascial lesions. It causes a trigger point, or hypersensitive region in the skeletal muscle. Pain is consistently reproduced at a specific site when the trigger point is stimulated.8) Common sites of pain include the head, neck, and lower back. It is usually managed with conservative treatment such as physical therapy and medication. In severe cases, the pain needs to be alleviated by inactivating the trigger point and restoring muscle function.1,7,9) Various studies have reported that pain due to cancer can create trigger points, that trigger points can coexist with cancer pain, and that pain may be exacerbated by cancer [5,10]. Especially in advanced cancer patients, opioids alone may not adequately control pain or the side effects of the opioids may prevent a satisfactory dosage from being attained [11-13]. In those cases, although cancer pain is difficult to control, total pain can be improved by managing other types of pain such as myofascial pain syndrome.
Most tender points are caused by myofascial pain syndrome, while some cancer pains can also create tender points. Therefore, it is difficult to differentiate cancer pain from myofascial pain syndrome before injection. Two patients with non-responsive pain were thought to have pain secondary to the cancer itself.
In this study, the accompanied symptoms such as nausea, vomiting, depression, and sleeping disorders were improved in a few patients. Because the pain itself is highly stressful, it affects the autonomic nervous system and can cause concomitant symptoms. Therefore, proper treatment of pain can improve the patient’s overall quality of life.
During the course of this study, some patients who did not benefit from the first injection were later satisfied with the final injections. This may be due to insufficient dosages or inappropriate site of injection initially. For that reason, we recommended at least two treatments before considering the injections ineffective.
There are several limitations of this study. First, the efficacy of treatment was dependent on the skill of the practitioner. Secondly, it was difficult to control the combined medicines that could interfere with pain control by injection. Lastly, the study group was small, and the study lacked a control group.
This study suggests that trigger point injection is an effective and safe supplemental treatment for controlling pain in cancer patients. However, the primary regimen for cancer pain remains to be the basic principles of the World Health Organization guidelines and attempting to control all cancer pain by trigger point injection alone is not advised.
Notes
No potential conflict of interest relevant to this article was reported.