Coronavirus Disease 2019 Presenting as Conjunctivitis
Article information
Abstract
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by a novel coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The world is currently challenged to handle this pandemic. The common symptoms of COVID-19 are fever, cough, fatigue, and shortness of breath. There are few reports on the association of SARS-CoV-2 with ocular abnormalities including conjunctivitis. We report a case of a 54-year-old woman who presented solely with conjunctivitis subsequently diagnosed with COVID-19. A lack of full history of her travel abroad was another issue leading to a delay in evaluating her COVID-19 status that increased the infection risk to her managing team. Thus, primary care practitioners should be suspicious of this atypical feature of COVID-19, thus enabling us to identify such patients at entry points. Maintaining safety measures while managing patients is also crucial.
INTRODUCTION
Coronaviruses are single-strand enveloped viruses with an RNA genome within the Coronaviridae family that infect humans and other mammals [1]. Previous outbreaks of coronaviruses include severe acute respiratory syndrome (SARS)-CoV in 2003 and Middle East respiratory syndrome-CoV in 2012, both of which were major threats to public health. In late December 2019, a novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified after the emergence of a pneumonia of unknown cause in Wuhan, Hubei, China termed coronavirus disease 2019 (COVID-19). Its rapid spread worldwide has led the World Health Organization to declare COVID-19 a pandemic on March 12, 2020. By March 26, 2020, 171 countries were affected by the COVID-19 pandemic, with 467,866 infected patients and 20,845 deaths, representing a 4.5% mortality rate [2]. COVID-19 exhibits a wide range of clinical presentations; the most common symptoms are fever, cough, fatigue, sputum production, headache, and shortness of breath [3]. Some reported atypical symptoms include vomiting, abdominal pain, diarrhea, anosmia, hyposmia, and ocular manifestations [4]. Several studies reported the association of SARS-CoV-2 with ocular abnormalities, including conjunctivitis. Herein, we report a case of a middle-aged female patient with COVID-19 infection who presented solely with conjunctivitis symptoms.
CASE REPORT
A 54-year-old Malay woman presented to the primary care clinic on March 31, 2020, with bilateral redness of her eyes lasting for 2 days. The redness started initially over her left eye for 1 day (Figure 1) and then spread to her right eye on the next day. These symptoms were associated with watery eyes and mild swelling over both eyelids. She denied any purulent eye discharge, eye pain, or blurring of vision. She also had no fever or any respiratory symptoms such as cough, sore throat, runny nose, or shortness of breath. She denied a history of recent contact with any conjunctivitis patient, allergies, or possible COVID-19 risk. Her history of travel to Egypt from March 10–20, 2020, was not disclosed, as Egypt was not one of the countries listed in the checklist of COVID-19-affected countries at that time.
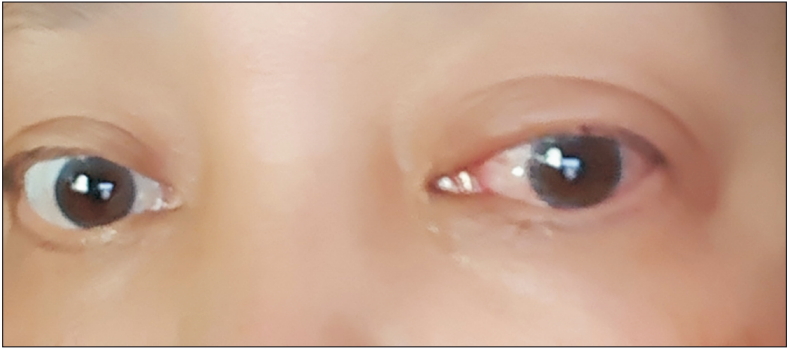
Left eye redness and eyelid swelling on presentation (day one). Informed consent was obtained from the patient for publication of this case report and accompanying images.
On examination, she was alert and conscious. Her conjunctivae were hyperemic bilaterally and there was mild swelling over her eyelids. Otherwise, her corneas were clear and her pupils were bilaterally reactive. Her vital signs were stable and she was afebrile. The patient was advised to perform cold compression and was prescribed artificial eye drops. Her eye symptoms gradually improved after 2 days.
The patient was then called by health authorities for COVID-19 testing together with her husband on April 8, 2020, after her husband developed acute respiratory symptoms starting on day 13 after travel. After 3 days, the results of her oropharyngeal and nasopharyngeal swab tests of SARS-CoV-2 by qualitative real-time reverse-transcriptase-polymerase-chain-reaction (RT-PCR) assay were positive, while those of her husband were negative. She denied any respiratory symptoms or fever during this period. She was then admitted to a COVID-19-treating hospital for further management. Subsequently, five of our managing staff who had had close contact with the patient during her visit to Hospital Universiti Sains Malaysia Outpatient Clinic were subjected to COVID-19 tests as an extra precaution even though they wore complete personal protective equipment including face shields, surgical masks, and aprons during that consultation. Their results were all negative.
In summary, our patient presented with conjunctivitis lasting for 4 days that had started on day 11 after returning from travel abroad. She was incidentally found to be positive for COVID-19 because her husband presented with acute respiratory infection with travel history. None of the managing team members were infected despite having direct contact with her due to adequate safety practices.
Informed consent was obtained from the patient for publication of this case report and accompanying images.
DISCUSSION
In late December 2019, SARS-CoV-2 was identified after the emergence of a series of cases of pneumonia of unknown cause in Wuhan, Hubei, China later identified to be COVID-19. This new viral illness has become a global public health concern in 2020 and exhibits a wide range of clinical presentations [3]. In this case report, the patient presented an atypical symptom of conjunctivitis and was subsequently diagnosed with COVID-19. She strongly denied any respiratory symptoms and fever, which are the common symptoms of COVID-19 [3]. We missed the early diagnosis of COVID-19 and treated the condition as common viral conjunctivitis as she did not fulfill the patient under investigation criteria and had an incomplete travel history.
The reported ocular manifestation of COVID-19 is acute follicular conjunctivitis meeting the criteria for acute viral conjunctivitis [5]. Previous studies showed SARS-Cov-2 led to ocular complications, but not in the early stage of infection [5,6]. They also suggested ocular symptoms commonly appear in patients with severe pneumonia [6]. However, this patient manifested with redness of the eyes and epiphora for 4 days without any preceding respiratory symptoms. Her presentation was similar in a confirmed COVID-19 patient who only had conjunctivitis characterized by conjunctival congestion and watery secretion for 3 days in early-stage disease [7].
The American Academy of Ophthalmology issued an alert in March 2020 that a simple red eye could be a sign of COVID-19 [8]. As SARS-CoV-2 is believed to be transmitted via droplets and contact surface through the mouth, nose, and eyes, the conjunctival mucosa can be directly exposed to infectious droplets during close contact and fomites when the eye is touched by contaminated hands [9]. The conjunctiva mucosa, nasolacrimal duct, and upper respiratory duct share the same entry receptor of SARS-CoV-2, angiotensin-converting enzyme 2 (ACE 2) [9]. Thus, the possibility of tear transmission of SARS-CoV-2 should not be ignored.
There are a few reports on the association of SARS-CoV-2 with ocular abnormalities such as conjunctivitis [6]. In one study, 12 of 38 clinically confirmed COVID-19 patients had ocular manifestations consistent with conjunctivitis; 11 of these patients with conjunctivitis had positive results for SARS-CoV-2 on RT-PCR from nasopharyngeal swabs [6]. The patient with conjunctivitis also showed positive results for SARS-CoV-2 on RT-PCR from both conjunctival and nasopharyngeal swabs [6]. However, transmission through infected ocular tissue or fluid remains controversial. The results of previous studies suggested that the conjunctiva is not a preferred tissue for SARS-CoV-2 infection due to the extremely low positivity rate of SARS-CoV-2 in tears and conjunctival secretions of patients with COVID-19 and the lower ACE 2 receptor expression on conjunctiva compared to that in human lungs [10]. Further research is needed to confirm SARS-CoV-2 ability to infect ocular tissue as well as its transmission mechanism.
Another issue raised here is that the patient acted against quarantine guidance as she thought she had common conjunctivitis and she had no respiratory symptoms. She was unaware that her conjunctivitis could be an atypical symptom of COVID-19 and, therefore, did not reveal her travel history, resulting in the primary care physician to treat her as having no risk of COVID-19. The implication of not revealing the COVID-19 risk can lead to disease transmission to health care workers. This case resulted in five health care workers being tested for the condition and placed on home isolation while awaiting these results. Fortunately, the results were negative. Information on epidemiological risk can affect patient management and limit disease spread, especially during the current COVID-19 pandemic; furthermore, increasing our role in triaging patients before further evaluation is required.
Therefore, we need to stay alert to the atypical symptoms of COVID-19 including viral conjunctivitis as a possible presentation, especially in those with associated risk factors such as a history of travel abroad or contact with patients with suspected or confirmed COVID-19. Face-to-face proximity during eye examinations may lead to exposure to patient secretions [8]. Healthcare workers should always practice the full recommended measures including strict hand hygiene and protecting exposed mucous membranes by wearing goggles, face shields, and face masks [8].
In conclusion, conjunctivitis is a common presentation in primary care; during the current COVID-19 pandemic, it should be suspected as one symptom of COVID-19, especially in persons at risk. Increased awareness of conjunctivitis as an atypical presentation of COVID-19 will heighten precautions including self-isolation and seeking medical attention by the public. Lastly, adequate history-taking, especially patient epidemiological risk factors, is crucial to prevent delay in evaluating COVID-19 status and virus transmission to healthcare workers, especially those on the front line.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
We would like to acknowledge the Hospital USM Director and the patient who provided consent for the case to be used for learning and publication purposes.
