Clinical Practice Guidelines for Managing Frailty in Community-Dwelling Korean Elderly Adults in Primary Care Settings
Article information
Abstract
Aging has become a global problem, and the interest in healthy aging is growing. Healthy aging involves a focus on the maintenance of the function and well-being of elderly adults, rather than a specific disease. Thus, the management of frailty, which is an accumulated decline in function, is important for healthy aging. The adaptation method was used to develop clinical practice guidelines on frailty management that are applicable in primary care settings. The guidelines were developed in three phases: preparation (organization of committees and establishment of the scope of development), literature screening and evaluation (selection of the clinical practice guidelines to be adapted and evaluation of the guidelines using the Korean Appraisal of Guidelines for Research and Evaluation II tool), and confirmation of recommendations (three rounds of Delphi consensus and internal and external reviews). A total of 16 recommendations (five recommendations for diagnosis and assessment, 11 recommendations for intervention of frailty) were made through the guideline development process. These clinical practice guidelines provide overall guidance on the identification, evaluation, intervention, and monitoring of frailty, making them applicable in primary care settings. As aging and “healthy aging” become more and more important, these guidelines are also expected to increase in clinical usefulness.
INTRODUCTION
Aging has become an important issue worldwide. According to statistics, in 2019, 25.6%, 65.3%, and 9.1% of the world’s population were young population (aged less than 15), working age population (aged 15 to 64), and elderly population (aged 65 and over), respectively [1]. While the trend of a decreasing working age population and an increasing elderly population continues globally, it has become more noticeable in Korea, where the proportion of the elderly population was 14.9% in 2019, and is expected to increase to 31.6% by 2067. This change in the population structure leads to a steep increase in the dependency ratio. In particular, the old-age dependency ratio is expected to increase sharply from 54.3% in 2019, to 85.2% in 2067 [1].
This aging trend has also led to an increase in the burden of medical expenses. In 2019, medical expenses for elderly adults amounted to 35.7 trillion won ($32.06 billion), a 1.6-fold increase from 2015, exceeding 40% of the total medical expenses for the first time in history [2]. Periodontal disease, hypertension, acute bronchitis, back pain, and arthritis were the most common, and chronic and musculoskeletal diseases were the most frequently occurring diseases [2]. The increase in medical expenses among the elderly is linked to increasing life expectancy, a growing elderly population and dependency ratio, and an increase in the number of people with chronic diseases.
Increased chronic diseases and functional decline are typical characteristics of geriatric diseases. Because geriatric diseases involve functional aspects and an increase in disease severity, it is difficult to achieve individual well-being and social burden relief with a disease management-oriented approach to elderly health. An important view on aging can be found in a 2015 World Health Organization report, that defines healthy aging as “the process of developing and maintaining the functional ability that enables well-being in older age.” [3] In 2020, the Decade of Healthy Aging (2021–2030) report also indicated that optimizing functional ability is key to healthy aging and suggested action plans to achieve the goal of continuous global healthy aging [4].
Frailty has become important in the context of the changing perspective on aging and its management. Frailty is a vulnerable state that results from the deterioration of overall function with aging, leading to a reduced physiological reservoir function in maintaining homeostasis. Thus, frail individuals fail to respond adequately to external stress [5]. Korean studies using Fried’s frailty phenotype, the most widely used tool to identify frailty, have found prevalence rates of 8.3% frailty and 49.3% pre-frailty, respectively [6,7]. Studies using other Korean versions of frailty evaluation tools have reported the prevalence of frailty to be from 14.1% to 21.3% [8-10]. The prevalence rate tends to increase with an increase in age, and is expected to increase further given the aging trend in Korea.
Proper management of frailty is an important factor in achieving healthy aging. In fact, it has been shown that frailty intervention can improve quality of life, reduce healthcare costs, and prevent negative consequences, such as hospitalization and death [11,12]. One study found that in the United States, a 10% reduction in sarcopenia prevalence, an important factor in frailty, could lead to a $1.1 billion per year reduction in healthcare costs [12]. In addition, positive results, such as improved physical function and quality of life, fall prevention, reduced emergency visits, and decline in healthcare costs have been reported with physical activity, polypharmacy, and nutritional interventions related to frailty [13-18].
As mentioned above, with the increase in the elderly population, healthy aging is gaining more and more emphasis and the management of frailty is increasing in importance. However, there are still no standardized clinical guidelines for the diagnosis and assessment of frailty and the implementation of appropriate interventions in Korea. Although the research on frailty is accumulating, and the guidelines for frailty have been developed and reported, it is difficult to apply them directly to the medical environment in Korea. Therefore, it is necessary to develop clinical practice guidelines for communitydwelling elderly adults in Korea to properly manage frailty in primary care settings.
METHODS
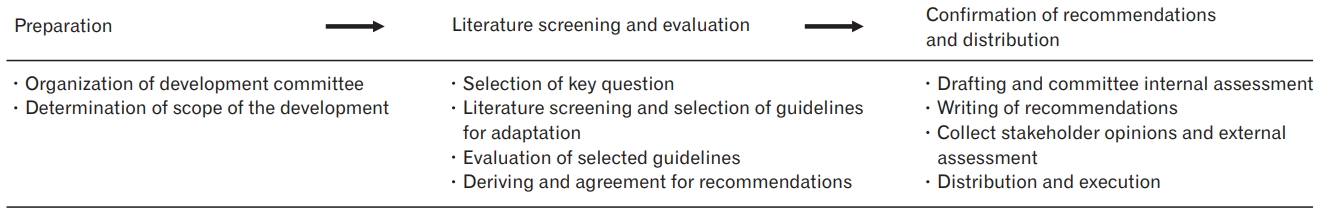
The clinical practice guidelines for frailty were developed using an adaptation method, which is outlined in the “Handbook for clinical practice guideline developer,” version 1.0 [19]. The development process was carried out in three phases: preparation, literature search and evaluation, and confirmation of recommendations and distribution (Figure 1).
1. Preparation: Organization of the Development Committee and Determination of the Scope for Guidelines
The development committee consisted of experts recommended by the associated academic societies. Specialists in family medicine and geriatricians participated in the development of the guidelines, and the committee consisted of six members of the legislation committee, 12 members of the development committee, and four members of the advisory committee.
The scope of the guidelines was determined by the committee to be as follows: (1) population: community-dwelling elderly adults aged 70 and older; (2) intervention: diagnosis and preventive or therapeutic intervention for frailty; (3) professionals: physicians in charge of primary healthcare in the community; (4) outcomes: prevention of occurrence of frailty and complications caused by frailty; and (5) healthcare setting: outpatient clinic in primary care setting.
2. Literature Search and Evaluation
For the literature search, we first selected key questions related to the recommendations. Each key question was structured in accordance with the PICO (P: population, I: intervention, C: comparison, O: outcome) format. A literature search was conducted based on these key questions. To select the clinical practice guidelines to be used for adaptation, we searched for literature published between January 1, 2000, and October 31, 2019. Electronic databases such as PubMed, KoreaMed, MedRIC, Google Scholar, and several guideline databases, including Guideline International Network, National Institute for Clinical Excellence, Scottish Intercollegiate Guidelines Network, and New Zealand Guideline Group, were searched. After the literature search and screening process, five guidelines were selected (Supplement 1).
These guidelines were evaluated for suitability using the Korean Appraisal of Guidelines for Research and Evaluation II (K-AGREE-II), which consists of 23 items organized into six domains [20]. The International Conference on Sarcopenia and Frailty Research International Clinical Practice Guidelines for Identification and Management [21], which obtained more than 70% in domain 3 of the K-AGREE-II, rigor of development, was chosen as the main guideline for adaptation. The remaining four guidelines did not meet the criteria for selection, as determined with the K-AGREE-II, but it was decided to refer to all of them after the development committee agreed in consideration of individual significance (Supplement 2).
3. Confirmation of Recommendations
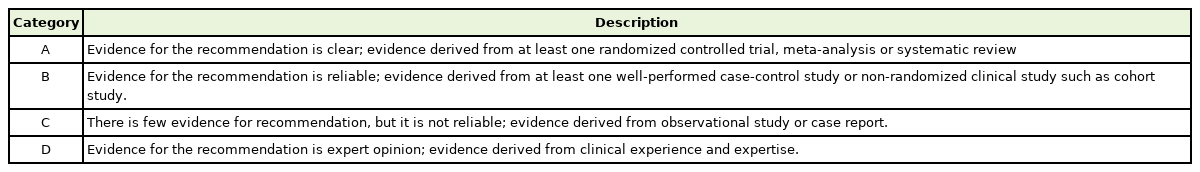
To derive recommendations for clinical practice guidelines for frailty, recommendations related to key questions were first compiled from the selected guidelines for adaptation. Based on these findings, recommendations were drafted. The guidelines used in the adaptation had different levels of evidence and strengths of recommendation, which could not be incorporated. Therefore, we used the level of evidence and strength of the recommendation criteria of the Korean Academy of Medical Sciences [22]. Tables 1 and 2 present the level of evidence and strength of recommendation, respectively. The strength of recommendation was determined by considering both the level of evidence, and the benefit and harm of the recommendation, along with the criteria of the Korean Academy of Medical Sciences.
A three-round Delphi consensus was conducted for the committee members to confirm the recommendations prepared, including the level of evidence and strength of the recommendation. In the first round, the related data were shared via e-mail for the members, and their opinions were obtained. In the second round, a 9-point scale of agreement was used for 16 items. In the survey results, 1–3 points indicated a lack of agreement, 4–6 points indicated that it was unclear whether there was agreement, and 7–9 points indicated that there was agreement. In accordance with the RAND/UCLA appropriateness method user’s manual (2001) [23], agreement was defined as the absence of a panel with a disagreement (1–3 points) response, with the average point of the panel being between 7 and 9 points for each item. Fourteen of the 16 items were agreed upon in the second round, and two items were not agreed upon. These two items were revised to reflect the opinions of committee members, and the third round was conducted. In the third round, all items were agreed upon, and the Delphi consensus process was completed (Supplement 3). The recommendations were subsequently finalized after consultation with the Special Committee on Geriatric Medicine of the Korean Academy of Family Medicine, and internal and external reviews were conducted. Finally, the recommendations were revised based on the opinions collected from internal and external reviews, and the guidelines were completed after a committee discussion.
4. Ethics Statement
This study was approved by the institutional review board of the Chungbuk National University Hospital (CBNUH 2021-03-007) and was conducted according to the tenets of the 1964 Declaration of Helsinki and its later amendments. It was published simultaneously in the Korean Journal of Family Medicine and the Korean Journal of Family Practice, with the approval of the editor-in-chiefs of the two journals, in order to enhance the utilization of guidelines for frailty in primary care settings in Korea.
RESULTS
Table 3 presents the guidelines for managing frailty in communitydwelling Korean elderly adults in primary care settings. In total, 16 recommendations were made, including five for diagnosis and assessment, and 11 for intervention and monitoring. Details of the level of evidence and strength of recommendations for each of these are attached as a supplementary file (Supplement 4) [15,16,21,24-61]. The full text of these guidelines can also be found at https://www.kafm.or.kr. In addition, the various evaluation tools examined during the development of the guidelines are also attached as separate files (Supplement 5) [6,8,62-71].
1. Diagnosis and Assessment
Screening for frailty (recommendations 1 and 2)
It is recommended to conduct a screening test for frailty among community-dwelling elderly adults aged 70 years or older. (Strength of recommendation: I, level of evidence: A)
It is recommended to use validated evaluation tools to conduct screening tests for frailty. (Strength of recommendation: I, level of evidence: A)
Screening for frailty is a critical first step in identifying patients with frailty and implementing appropriate interventions. For a proper screening test, the use of a validated evaluation tool is required, and the choice of the tool requires consideration of time, convenience of the evaluation method, and location requirements. Considering these points, the Frailty Phenotype Questionnaire (FPQ) and the Korean version of the FRAIL scale (K-FRAIL scale) are the evaluation tools applicable for screening for frailty in primary care settings.
The FPQ is suitable for screening tests, as it is not only includes for Fried’s frailty assessment, which is widely used for the diagnosis of frailty, but also consists of questionnaire items that do not require much time [62]. A total score of 0 indicates robustness, 1–2 indicates prefrailty, and 3–5 indicates frailty [62].
The FRAIL-Scale, a tool similar to the FPQ, consists of five questions, with one of Rockwood’s frailty index added to four items of Fried’s frailty assessment [9]. The FRAIL-Scale is also suitable for use in primary care settings because it requires little time to administer, and the evaluation method is not difficult and does not require a high level of expertise. In addition, the feasibility and validity of the Korean version of the K-FRAIL scale were also studied. The evaluation score scheme for the K-FRAIL-Scale was the same as that for the FPQ [9].
Diagnosis and assessment of frailty (recommendations 3, 4, and 5)
Diagnostic tests for patients with frailty or pre-frailty status in the screening test may be considered. (Strength of recommendation: IIb, level of evidence: C)
It is recommended to conduct a comprehensive geriatric assessment (CGA) in patients diagnosed with frailty. (Strength of recommendation: I, level of evidence: A)
It is recommended that patients diagnosed with advanced frailty be referred to geriatric specialists who can provide specialized management in geriatric medicine. (Strength of recommendation: I, level of evidence: C)
CGA is a key process in the prevention of negative consequences that involve implementing necessary interventions through appropriate evaluation for elderly individuals with frailty [72,73]. Although CGA is important in frailty, there are difficulties surrounding its use, as it is made up of several domains, which require a considerable amount of time when conducting evaluation tests for each area. There may also be space restrictions. Therefore, CGA cannot be implemented in all community-dwelling elderly adults. This is the reason why screening and diagnostic evaluations are required to identify frail elderly adults.
Diagnostic tests to confirm frailty may be conducted in patients with suspected frailty or pre-frailty after screening. However, there is no clear boundary between screening and diagnostic tests; therefore, a diagnostic test is not mandatory. The following assessment tools may be used when conducting diagnostic tests: Fried’s frailty assessment [6], the Korean Frailty Index for Primary Care [74], and the Korean Frailty Index [8].
CGA should be conducted on patients diagnosed with frailty after screening and diagnostic tests; however, because of the time and space requirements mentioned above, it may be difficult to carry out CGA in primary care settings in Korea [73]. To address these issues, CGA tools have been developed so that they can be applied to outpatient clinics by reducing the time required and simplifying the items. CGA tools with proven reliability and validity in Korea include the Korean Brief Comprehensive Geriatric Assessment Questionnaire and the Korean Comprehensive Assessment Tools for Geriatric Ambulatory Care [63,75]. In addition, for the Korean Comprehensive Assessment Tools, a short version was also developed, which can be applied when performing CGA in outpatient clinics in primary care settings [63].
2. Intervention and Monitoring
Polypharmacy (recommendation 6)
It is recommended to assess and review the medications being used by patients with frailty and to make adjustments to the drugs, if necessary. (Strength of recommendation: I, level of evidence: A)
Polypharmacy is defined as either dosing a variety of drug simultaneously, or dosing an excessive number of drugs. Elderly adults are more likely to develop polypharmacy because they often have various chronic diseases. Negative outcomes, such as falls, drug side effects, drug interactions, and increased hospitalization and mortality, are more commonly observed in patients with polypharmacy [76-78]. Therefore, in patients diagnosed with frailty, a review and evaluation of the medications being used is required.
Tools to evaluate the appropriateness of prescription drugs for elderly adults include the beers criteria (available from: https://www.americangeriatrics.org/media-center/news/older-people-medications-are-common-updated-ags-beers-criteriar-aims-make-sure) [79], Screening Tool of Older Persons’ potentially inappropriate Prescriptions/Screening Tool to Alert doctors to the Right Treatment (STOPP/START) criteria (available from: https://psnet.ahrq.gov/issue/stoppstart-criteria-potentially-inappropriate-prescribing-older-people-version-2) [80], and Korean Potentially Inappropriate Medication List [81]. These instruments present representative drugs that are potentially inappropriate for the elderly, so it is recommended that medication adjustments be made with reference to the drug assessment being taken, if necessary.
Physical activities (recommendation 7)
It is recommended that physical activities, including resistance, aerobic, and balance exercises, be implemented in patients with frailty. (Strength of recommendation: I, level of evidence: A)
The prevention of muscle loss through physical activity in frail elderly individuals is one of the most important factors in maintaining function [82]. However, because the level of fitness possible is different for each person, it is necessary to evaluate individual physical abilities for each patient and recommend appropriate programs accordingly [83,84]. To evaluate the physical capability of elderly adults, evaluation tools such as the Short Physical Performance Battery and Senior Fitness Test are available. In addition, there are other methods such as assessment of performance in activities of daily living and instrumental activities of daily living, and the physical activity assessment items included in the CGA for an approximate determination of physical function.
As expected, using these assessment tools, it is highly ideal to apply programs tailored to the capacity for physical activity of each patient. However, there are restrictions in their use in outpatient clinics because of the issues with time and required personnel. As an alternative, the method of measuring physical fitness and prescribing exercise programs of the National Fitness Awards operated Korea Sports Promotion Foundation may be considered (available from: http://nfa.kspo.or.kr).
After assessing the capacity for physical activity in elderly adults with frailty, and then recommending physical activity, three basic guidelines are included: (1) It is recommended that aerobic physical activity, muscle strengthening, and balance training activities be carried out by adults aged 65 years or older; (2) They should start with low-intensity exercise and gradually increase the intensity; and (3) Warm-up and cool-down should be included before and after exercise. As previous studies have shown, physical activity has a clear beneficial effect on frailty, but there may be risks associated with physical activities in elderly adults, so the above basic guidelines should be followed with caution.
For treatment through physical activity, more attention is required for elderly adults, particularly those in high-risk groups. Elderly adults with movement limitations are considered a high-risk group, and thus, the following exercises are recommended by Health Moves for Aging Well (Health Moves): (1) sitting position: bending arms, walking in place, bending, and straightening ankles; (2) standing position: standing on a chair and standing in place [85]. Elderly individuals with underlying diseases are also among the high-risk groups. Cardio-cerebrovascular disease, heart disease, hypertension, diabetes mellitus, and joint diseases can cause restrictions on physical activity [86]. Therefore, it is necessary to recommend physical activities based on an understanding of the precautions for each disease, and appropriate individual exercise should be prescribed.
Nutrition and oral health (recommendations 8 and 9)
It is recommended to evaluate body weight loss and nutritional status in patients with frailty and to perform interventions. (Strength of recommendation: I, level of evidence: A)
Evaluation and training of oral health in patients with frailty should be considered. (Strength of recommendation: IIa, level of evidence: A)
Evaluation of nutritional status is important in the intervention for frailty, as poor nutrition and malnutrition are found to be related to the occurrence and deterioration of frailty [24,25]. Nutritional search tools are available to assess weight loss and nutritional status. One of the widely used tools is the Mini Nutritional Assessment (MNA), which has the advantage of being able to screen comprehensive nutritional status of elderly patients in a short period of time and is also useful for predicting mortality. In addition, the Korean version of the MNA is a recommended tool for nutritional evaluation in primary care settings. It requires less than 10 minutes to complete, and studies of the elderly population in Korea that have used this tool have been reported [64,87].
Nutritional intervention should be implemented for frail elderly individuals with identified nutritional problems through evaluation, but there is still confusion about its effectiveness and direction of intervention [21,24,88]. Nevertheless, we recommend that nutritional interventions, including protein supplementation, be conducted in patients with frailty who have been found to be undernourished according to the MNA through a review of related studies [89-91]. A dosage of 1.5 g/kg/d protein supplementation has shown effectiveness, should it be required [91].
Additionally, oral health is closely related to the nutritional status of the elderly. Furthermore, studies have reported that oral health is also related to frailty, which requires evaluation, intervention, and nutritional evaluation [26,65,92]. In the outpatient clinic in the primary care setting, assessment tools such as the Geriatric Oral Health Assessment Index are available, and should be encouraged for regular dental examinations in the care of elderly patients [93,94]. Dental examinations should be conducted every 3–6 months for patients with teeth, and every 12 months for patients without teeth, by the dentist.
Vitamin and hormones (recommendations 10 and 11)
Vitamin D supplementation is recommended only for patients with frailty with vitamin D deficiency. (Strength of recommendation: I, level of evidence: A)
Hormone supplementation therapy aimed at treating frailty is not recommended. (Strength of recommendation: III, level of evidence: A)
Several studies have reported that low vitamin D levels are associated with frailty [27,95]. Thus far, with regard to vitamin D, there has been no consensus on the deficiency or the minimum required concentration [96]. Furthermore, studies on vitamin D administration in frail elderly individuals have failed to show uniform results [24,97-99]. However, vitamin D administration in elderly adults with confirmed frailty has shown positive results in preventing falls [100]. Accordingly, vitamin D supplementation should be carried out in frail elderly individuals with vitamin D deficiency.
Hormonal changes associated with aging are associated with sarcopenia, which is known to play a role in the development of frailty. Hormones that are mainly associated with frailty include growth hormones, testosterone, and dehydroepiandrosterone. There have been discussions on whether supplementation of these hormones could improve or delay frailty, but this is not recommended because the benefits of using this therapy are unclear and there is a possibility of long-term side effects.
Cognitive function (recommendations 12 and 13)
Evaluation of cognitive function in patients diagnosed with frailty should be considered. (Strength of recommendation: IIa, level of evidence: B)
Interventions to prevent cognitive impairment should be considered selectively in patients diagnosed with frailty. (Strength of recommendation: IIa, level of evidence: A)
Several studies have reported that frailty acts as a predictive factor or is associated with cognitive impairment [28,29,101]. The implementation of interventions for cognitive functions in patients with frailty or prefrailty also results in the effective maintenance of functional conditions [89]. Therefore, proper evaluation and intervention for cognitive functions in frail elderly individuals is important. Evaluation tools, such as the Korean Mini-Mental State Examination, can be used to screen for cognitive impairment [66], and the Montreal Cognitive Assessment can be used if mild cognitive impairment is suspected (available from: https://new.neuro.or.kr/file/K-MoCA.pdf) [102-104].
It is not yet clear whether implementing interventions when cognitive impairment is confirmed will help prevent complications or manage frailty. However, there is evidence that implementing multifactorial interventions, such as exercise, nutritional supplementation, and cognitive training, is effective in the recovery and prevention of the progression of frailty. In the outpatient clinic of the primary care setting, such multifactorial interventions can be considered selectively for frail elderly adults with mild cognitive impairment [30,31,89,105]. These interventions are mainly composed of non-pharmacological therapy, including (1) prevention by controlling cardio-cerebrovascular risk factors [106-108], (2) physical activity and exercise therapy [89,105,109], and (3) cognitive training [110]. There is a lack of evidence as to whether pharmacological treatment is helpful in cognitive intervention for patients with frailty.
In patients with moderate to severe cognitive impairment, who are difficult to manage in a primary care setting, referral to a medical institution capable of comprehensive intervention should be considered. Additionally, a referral is also required for patients with dementia accompanied by various behavioral disorders and psychological symptoms [32,111].
Fall (recommendation 14)
Fall screening tests (history taking for falls and assessment of gait and balance) should be conducted in elderly adults with frailty, and interventions should be considered for multi-dimensional fall risk assessment and fall prevention in high-risk groups. (Strength of recommendation: IIa, level of evidence: B)
Falls are a common problem among the elderly population. The incidence of falls among community-dwelling elderly adults aged 65 or older is reported to be approximately 30%–40%, and increasing with age [112,113]. Falls in elderly adults cause physical damage and increase functional dependence, which reduces the quality of life. Frailty is closely related to falls and fractures in elderly adults, and may be involved in increasing the risk of death from fall-related fractures [114]. Therefore, in patients with frailty, it is necessary to identify their history of falls and conduct fall screening tests, such as walking and balance assessment.
In this context, a more comprehensive “multi-dimensional fall risk assessment” and intervention should be considered if the patient is determined to be at a high risk for falls. Fall-related risk factors include old age, past experience of falls, polypharmacy, impaired vision, walking disorders, muscle weakness, arthritis, osteoporosis, hypoglycemia, and cognitive dysfunction [115,116]. A multidimensional fall risk assessment of these various risk factors can also help determine appropriate interventions for problems based on the results of the assessment [116].
Regarding interventions for fall risk factors, exercise interventions have been reported to improve fall-associated indicators and to increase muscle strength, but did not reduce the actual incidence of falls [117,118]. However, some studies have reported that exercise therapy helps to reduce the incidence of falls and improve walking ability and balance [119]. Considering the clinical significance of falls, although the evidence is limited, exercise therapy for fall intervention should be implemented in patients in high-risk groups. In addition, vitamin D supplementation may be considered, when the patient has a deficiency [116,120].
Social frailty (recommendation 15)
Evaluation and intervention for social frailty in patients diagnosed with frailty are recommended. (Strength of recommendation: I, level of evidence: C)
Social frailty is a concept that has become more important, as it involves multiple factors resulting from the accumulation of deficits in physical, psychological, and social aspects [121]. In fact, several studies have confirmed that social frailty leads to physical or psychological dysfunction [33,122,123], and that social frailty without physical frailty is associated with functional decline [33].
Social frailty involves the following domains: social activities, roles, relationships, and support [33]. Several tools, measuring these domains, have been developed to assess social frailty. Tools, such as the Tilburg Frailty indicator, a seven-item social frailty index, and a social vulnerability index, can be used. The Lubben Social Network Scale is often used, and research on the validity and reliability of the Korean version is underway, which can be used to evaluate social support needs [67]. Immediate support is required when the risk of social isolation is high, but the evidence related to the intervention for social frailty remains limited [124,125].
Interventions for social frailty are usually performed by combining parts of social frailty interventions with existing frailty interventions. These include conducting exercise programs for physical activity intervention in groups, or implementing volunteer visit programs for social contact with patients who suffer from movement restrictions [117,126,127]. More effective intervention can be achieved if community and medical institutions work together.
Monitoring (recommendation 16)
Periodic evaluation and monitoring may be considered in patients diagnosed with frailty. (Strength of recommendation: IIb; level of evidence: D)
It is very important to identify frailty and determine what interventions are required, but it is difficult to expect a significant effect if it is only a one-off event. Existing clinical practice guidelines have rarely addressed monitoring, and even though literature reviews have been conducted, there is a lack of evidence regarding periodic evaluation and monitoring of patients with frailty. However, because frailty is a continual concept, periodic evaluations and subsequent development and implementation of intervention plans are required.
The following methods can be considered for periodic evaluation and monitoring of patients with frailty: (1) the use of CGA and (2) monitoring using mobile technology. CGA is an important evaluation process for developing early intervention plans for patients diagnosed with frailty [34,128]. However, CGA can also be used for revaluation, because the status of individual patients may change from the time of the initial assessment [72,73]. At the time of revaluation, a CGA can be re-conducted focus on areas with deterioration of condition [73]. With advances in mobile technology, research results on monitoring of frailty using remote monitoring equipment have been reported [129-132]. Based on these findings, mobile technology, in addition to CGA, may serve as an effective monitoring method.
CONCLUSION
Aging is now a worldwide problem, and “healthy aging,” as proposed by the World Health Organization, is also a global challenge to achieve. Healthy aging is a concept that emphasizes the importance of maintaining function for the individual well-being of elderly adults. It also argues that frailty results from the overall decline in function. Therefore, the proper management of frailty is important for achieving healthy aging.
Considering the effects of frailty on healthy aging, these clinical practice guidelines are beneficial, as they provide overall guidance on a set of processes for identifying and evaluating frailty, implementing appropriate interventions, and periodically monitoring frailty status. In addition, involving primary care settings is important for the effective management of frailty, and this guideline, from this perspective, may also be meaningful. This guideline will be updated to reflect its actual usage experience in the field of healthcare and related research results, which will be published later. This would solve the problem of insufficient evidence regarding the recommendations for the management of frailty. The development committee expects this guideline to help manage frailty in primary care settings and contribute to improving quality of life in the aging population.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
This study received financial support from the Korean Academy of Family Medicine.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4082/kjfm.21.0162. Supplement 1. Strategies of searching. Supplement 2. Results of Korean Appraisal of Guidelines for Research and Evaluation II (K-AGREE-II). Supplement 3. Results of Delphi consensus. Supplement 4. Details of overall recommendation, including the process of deriving individual recommendations. Supplement 5. The various assessment tools include in the recommendations.
Strategies of searching
Results of Korean Appraisal of Guidelines for Research and Evaluation II (K-AGREE-II)
Results of Delphi consensus
Details of overall recommendation, including the process of deriving individual recommendations
The various assessment tools include in the recommendations