Comparison between the International Classification of Primary Care and the International Classification of Diseases Classifications in Primary Care in Korea
Article information
Abstract
Background
The International Classification of Primary Care-2 (ICPC-2) is a classification method designed for primary care. Although previous studies have found that ICPC-2 is a useful tool for demonstrating the relationship between patients’ expectations and health providers’ diagnoses, its utility of ICPC-2 has yet to be fully studied in Korea. This study aimed to evaluate the practicality of ICPC-2 in Korean primary care.
Methods
The study was conducted at primary care clinics in Seoul and Gyeonggi areas from October to November 2015. Third-year family medicine residents examined and analyzed the medical records of patients who visited primary care physicians using ICPC-2, and the results were compared with those obtained using the International Classification of Diseases-10 (ICD-10) (Korean version: Korean Standard Classification of Diseases-7).
Results
A total of 26 primary care physicians from 23 primary care clinics participated in the study. Furthermore, 2,458 ICD-10 codes and 6,091 ICPC-2 codes were recorded from the data of 1,099 patients. The common disease codes were vasomotor and allergic rhinitis (J30), according to ICD-10, and acute upper respiratory infection (R74) in ICPC-2. Comparing disease status by body systems, the proportion of gastrointestinal disease with ICD-10 codes was significantly higher than that with ICPC-2 codes (P<0.001). Furthermore, patients with >4 diagnoses accounted for 36% of the ICD-10 classifications, whereas those with >4 diagnoses accounted for 4% of the ICPC-2 classifications.
Conclusion
Introducing ICPC as a complementary means for diagnosing common diseases could be a practical approach in Korean primary care.
INTRODUCTION
Primary care effectively reduces the risk of disease and mortality rate by accurately grasping patients’ health problems based on detailed information, including not only their chief complaint or physical signs but also their concerns and reasons for their visit, as well as familial or socioeconomic problems through a long-term doctor–patient relationship [1-5]. The classification and coding of medical care content are important for accumulating patients’ medical information and supplying appropriate and continuous medical services during primary care [6].
The 10th Revision of the International Statistical Classification of Diseases and Related Health Problems (International Classification of Diseases-10 [ICD-10]), developed by the World Health Organization, is an international classification and diagnostic tool that provides information on the causes of death and diagnoses of morbidity and mortality statistics [7]. In South Korea, the translated version of ICD-10 has been adapted for medical classification under the national health insurance (NHI) system, and medical fee reimbursement is performed based on ICD-10 [8]. ICD-10 is also useful for comparisons between countries, final diagnoses, and insurance claims [7]. ICD-10 codes lack accuracy in terms of clinical diagnoses and concepts [9]. The limitations of ICD-10 include detailed content regarding the individual care of patients, such as patients’ reasons for encounters (RFEs), healthcare processes, or unsolved medical problems [10]. Therefore, the use of ICD-10 codes may be limited in primary care clinics because many patients present with ambiguous symptoms. In addition, the fee-for-service payment, in which the National Health Insurance Corporation reimburses hospitals and doctors for each service they provide to their patients according to ICD-10, has certain problems, such as a high cost per encounter amount and the use of many codes to obtain reimbursement [11]. Furthermore, diverse and subdivided healthcare statistics containing RFEs, healthcare processes, and diagnoses are required to manage and prevent diseases at the national level.
The International Classification of Primary Care (ICPC), developed by the World Organization of Family Doctors in 1987, offers the following three important elements of doctor–patient encounters: RFEs, diagnoses or problems, and process of care. ICPC-2, published in 2000, is based on a biaxial structure and consists of 17 chapters, each divided into the following seven components: (1) symptoms and complaints; (2) diagnostics, screening, and preventive procedures; (3) treatment procedures and medications; (4) test results; (5) administrative; (6) referral; and (7) diagnosis/disease [12]. ICPC provides detailed information regarding patient care from the start of RFEs to its conclusion with a diagnosis [12-14]. Therefore, ICPC is a patient-centered classification method conducted by recording RFEs, diagnoses or problems, and care [15]. ICPC is widely used in Europe; however, it is not yet broadly recognized in Asia. A Chinese study found that ICPC is useful in monitoring general practice from the perspective of both patients and providers [16]. However, only a few studies have been conducted in South Korea. Therefore, this study aimed to investigate the medical care contents of patients who visited primary care clinics using ICPC-2 and compared the results with those using ICD-10 in the Korean population residing in the Seoul and Gyeonggi.
METHODS
1. Study Design
This study was conducted at primary care clinics in the Seoul and Gyeonggi from October 2015 to November 2015. This study was conducted as part of a public research project supported by the National Evidence-based Healthcare Collaborating Agency (NECA). Informed consent was obtained from all the participants. The study was approved by the Institutional Review Board of NECA (IRB approval no., 15-022).
There are 420 primary care clinics located in the Seoul and Gyeonggi-do where members of the Korean Association of Family Physicians practice. We excluded clinics that declined to participate (N=397). Finally, 23 primary care clinics were included in this study. A total of 26 primary physicians from 23 clinics agreed to participate, and we collected data from 1,099 patients from these primary care clinics.
The investigators were third-year family medicine residents. After standardized education and training on the ICPC classification system (2 hours of theory and 2 hours of practice), they visited the sample primary care clinics. They observed the patients’ medical care processes and completed case report forms (Supplement 1). The investigators recorded the basic information (age and sex) of patients who visited the clinics and coded diseases using ICD-10 (Korean version: Korean Standard Classification of Diseases-7) and the main medical problems (symptoms) using ICPC-2. The two coding systems were compared by analyzing the frequency of primary and accessory diagnoses of ICD-10 and seven components of ICPC-2. The seven ICPC-2 components for the most common diagnoses in ICD-10 were also analyzed.
2. Survey for Primary Physicians
A total of 26 primary care physicians responded to the questionnaire. The questionnaire items were about the degree to which ICPC codes are helpful in primary care, degree of improvement in the primary care environment, matters to be reinforced for the introduction of ICPC codes, and baseline information about the primary physicians (age, sex, working years, average number of outpatients per day, and experiment about ICPC) (Supplement 2). Items measuring satisfaction were scored from 1 (very poor) to 5 (excellent), except for items that required reinforcement for the introduction of ICPC codes (descriptive questions). The questions measuring satisfaction were scored from 0 to 10, with higher scores indicating higher levels of satisfaction.
3. Statistical Analysis
The results are expressed as mean and standard deviation (SD) for continuous variables or numbers (percentage) for categorical variables. We conducted a chi-square test to compare the differences in categorical variables. A paired t-test was used to confirm the difference in awareness between ICD-10 and ICPC-2. Two-sided values of P<0.05 were regarded as significant. All analyses were conducted using IBM SPSS Statistics for Windows ver. 25.0 (IBM Corp., Armonk, NY, USA).
RESULTS
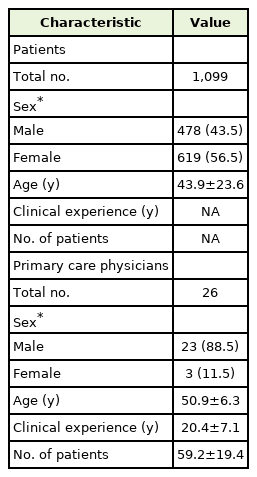
The general characteristics of the samples are presented in Table 1. We analyzed 1,099 patients aged 1–94 years (mean age, 43.9±23.3 years). We recruited 22–74 patients from each clinic, and 26 primary care physicians participated voluntarily. The mean±SD age was 50.9±6.3 years, and 23 (88.5%) were men. The average number of patients who visited a clinic per day was 59.2±19.4. Four physicians (15.4%) had experience with ICPC-2.
A total of 2,458 ICD-10 and 6,091 ICPC-2 codes were recorded from the participant’s data. ICPC-2 codes included 1,976 RFEs (32.4%), 2,459 processes (40.4%), and 1,656 diagnoses (27.2%). Symptom and sign codes according to ICD-10 (R code) totaled 76 (3.1%) (Table 2).
The classification status according to ICD-10 and ICPC-2 codes by body system is described in Supplement 3, which shows 2,460 ICD-10 and 1,638 ICPC-2 codes. The most common diagnosis codes reported using ICD-10 were for the respiratory system (n=895, 36.4%), followed by the digestive (n=400, 16.3%), musculoskeletal (n=218, 8.9%), and circulatory (n=154, 6.4%) systems. The most common diagnosis codes reported using ICPC-2 were for the respiratory system (n=780, 47.6%), followed by the digestive (n=201, 12.3%), cardiovascular (n=143, 8.7%), endocrine/metabolic (n=130, 7.9%), and musculoskeletal systems (n=126, 7.7%) (Supplement 3). In the comparison of disease status by body system, the proportion of gastrointestinal disease with ICD-10 codes was 16%, which is significantly higher than the 12% reported with ICPC-2 (P<0.001).
The top 10 codes according to ICD-10 and ICPC-2 are presented in Table 3. The most common diagnosis codes reported using ICD-10 were vasomotor and allergic rhinitis (J30), acute bronchitis (J20), gastritis and duodenitis (K29), and essential hypertension (I10). The most common codes reported using ICPC-2 were acute upper respiratory infection (R74), allergic rhinitis (R97), acute bronchitis/bronchiolitis (R78), and uncomplicated hypertension (K86). Table 4 shows the RFEs and treatment process codes for vasomotor and allergic rhinitis (J30), which were the most frequent diseases when ICD-10 was used, according to ICPC. Although the patient had the same disease according to ICD-10, ICPC-2 could provide more detailed descriptions of various RFEs and treatment processes than ICD-10.
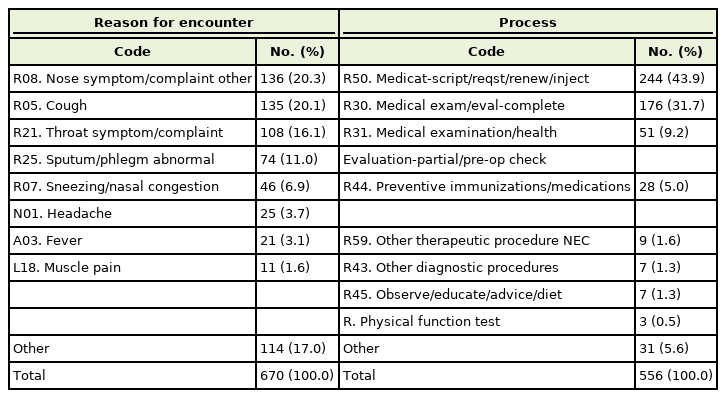
Reason for encounters and processes of care for vasomotor and allergic rhinitis in the ICD-10, according to the ICPC-2 classification
Figure 1A describes the percentage of patients with comorbid diagnosis codes according to ICD-10 and ICPC-2. The number of patients with no diagnosis codes for ICD-10 was 0%, whereas it was 17% for ICPC-2. Patients with one, two, three, and more than four diagnoses accounted for 18%, 23%, 24%, and 36% of the sample, respectively, in ICD-10. The same groups comprised 39%, 29%, 11%, and 4% of the sample, respectively, according to ICPC-2. The proportion of patients with more than four diagnosis codes in ICD-10 was significantly higher than that in ICPC-2.
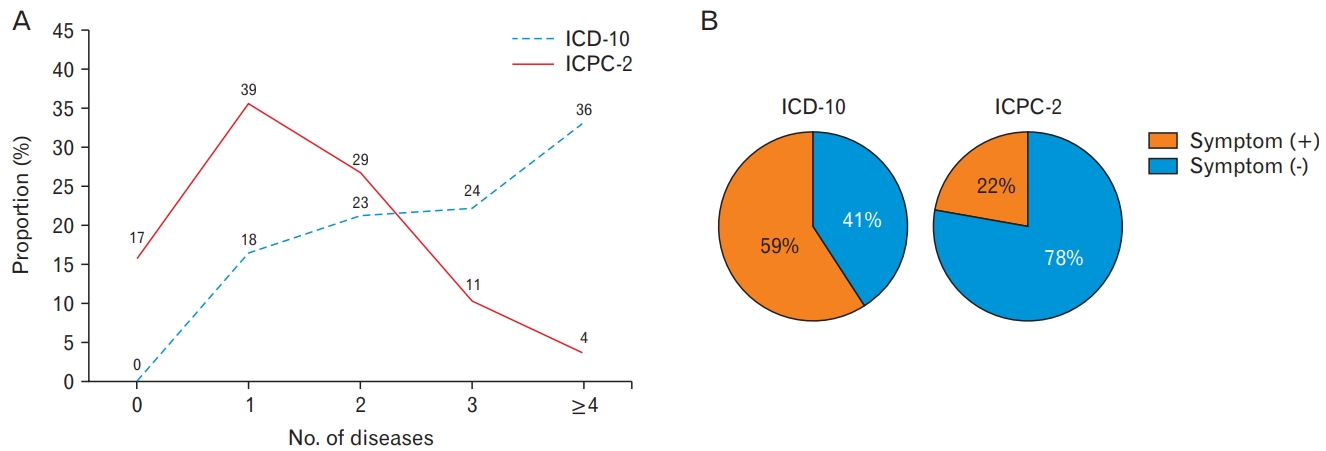
Comorbid diagnosis codes according to International Classification of Diseases-10 (ICD-10) and International Classification of Primary Care-2 (ICPC-2).
Figure 1B presents the diagnosis codes and presence of related symptoms in ICD-10 and ICPC-2. In ICD-10, the digestive system had the second-highest number of diagnosis codes. There were 289 patients corresponding to 400 digestive ICD-10 codes. Of these, 170 (59%) did not have digestive symptoms. There were 164 patients corresponding to 201 digestive ICPC-2 codes. Of these, 36 (22%) did not exhibit any digestive symptoms. Thus, significant differences were found between ICD-10 and ICPC-2 (P<0.001) (Figure 1B).
The primary care physicians’ awareness of ICD-10 and ICPC-2 is presented in Supplement 4. The familiarity score was significantly higher for ICD-10 than for ICPC-2 (3.8±0.9 versus 2.0±0.9, P<0.001). The scores for the degree of helping care for patients’ health and reflectivity of the treatment process were significantly higher for ICPC-2 than for ICD-10 (degree of helping care for patients’ health: 2.8±0.9 in ICD-10 versus 3.5±0.7 in ICPC-2, P=0.016; reflectivity of treatment process: 3.2±1.1 in ICD-10 versus 3.8±0.7 in ICPC-2, P=0.002). The scores for writing time, difficulty in determining a relevant diagnosis code, and satisfaction were not significantly different between ICD-10 and ICPC-2.
DISCUSSION
This study compared the RFEs, symptoms, processes, and diagnoses of patients who visited primary care clinics using ICPC-2 and ICD-10 codes. ICPC-2 provided more varied and comprehensive information regarding RFEs and patient symptoms. Furthermore, the proportion of patients with more than four diagnoses was significantly lower with ICPC-2 than with ICD-10. Additionally, the presence of symptoms related to the diagnosis code was significantly higher with ICPC-2 than with ICD-10.
A recent study reported that symptom-specific ICD-10 codes lacked sensitivity and failed to encompass many patients with relevant coronavirus disease-2019 (COVID-19) symptoms [17]; thus, the false-negative rate was unacceptably high. The identification of these symptoms is important for COVID-19 surveillance and research. Similar inaccuracies have been reported in the literature regarding atrial fibrillation and stroke [6,18].
Detailed information, such as reasons for seeking care, emotions, cognitions, worries, and fears, is necessary for the comprehensiveness and continuity of patient treatment in primary care [19]. Detailed patient information is also associated with improved outcomes [3,19] and increased efficiency of care [20-22]. Furthermore, under the same diagnosis, the treatment course can vary based on the patient’s condition, underlying disease, or needs. Unfortunately, ICD-10 codes do not sufficiently explain the complete and precise medical history of each patient [18]. Unlike ICD-10, ICPC-2 can provide diverse information, including RFEs, decision-making processes, and outcomes of care [23]. Therefore, ICPC-2 is required to support comprehensive, continuous, and patient-centered primary care. The number of ICD-10 diagnosis codes, except for symptom (R code) and prevention (Z code) codes, was 1.36 times greater than that of ICPC-2 diagnosis codes (-70 to 99). However, the total number of ICPC-2 codes, classified as detailed codes, such as RFEs and process of care, was 2.66 times greater than the number of ICD-10 codes. Furthermore, 36% of the patients were diagnosed with more than four comorbidities, accounting for nearly one in three cases in ICD-10; however, it was only 4% in ICPC-2.
This pronounced disparity in the number of diagnosis codes could be due to current NHI services. Although doctors can barely determine a patient’s diagnosis at their first encounter or presentation (in this study, undiagnosed patients accounted for 15.2% [n=167]), presumed diagnosis codes were included in ICD-10 for claims under the NHI service. However, ICPC-2 could determine RFEs and diagnostic processes (test, treatment for acute disease, etc.) for a precise diagnostic decision-making. Therefore, ICPC-2 could be a useful tool for reflecting the relationship between patient expectations and health providers’ diagnoses.
Diagnosis codes related to the digestive and musculoskeletal systems in ICD-10 outnumbered those in ICPC-2. In addition, among patients diagnosed with digestive or musculoskeletal diseases according to ICD-10, more than half did not complain of related symptoms. These results could imply that ICD-10 utilizes some codes for other purposes, such as healthcare claims, and not for actual patient diagnoses.
Under the current reimbursement system, physicians might not only include codes of suspicious diagnoses according to ICD-10 but also enter codes for preventive medication [24]. For example, when a patient reports gastric discomfort while taking nonsteroidal anti-inflammatory drugs, physicians may prescribe proton pump inhibitors or histamine-2 receptor antagonists with painkillers and then enter the digestive system codes in ICD-10 to claim insurance. In this survey, the difference in the proportion of digestive system codes and the change in the rank order of musculoskeletal system codes between the two classification systems could support this process. Similarly, when physicians prescribe medications for respiratory diseases, they usually prescribe painkillers and gastrointestinal medications to protect the gastric mucosa. For health insurance reimbursement, physicians inevitably code for a diagnosis that is unrelated to the ICD-10 symptoms.
Therefore, ICD-10 could misrepresent patients’ actual health conditions, leading to distortion of medical care. Since the priority of disease according to ICD-10 includes patients’ fictional diseases, demographics using ICD-10 can cause errors, such as easily coding certain diseases frequently for health insurance claim estimates. Therefore, given the increasing need for diverse, subdivided, and precise healthcare statistics at the national level, it is necessary to adopt classifications that are more appropriate and supplement the primary care insurance system by reflecting the actual healthcare.
ICPC-2 can overcome the limitations of the existing ICD-10. However, because ICPC is a classification system for primary care, it might be more practical to apply it as an auxiliary means for addressing common diseases in primary care rather than introducing it for all diseases. Some ICPC-2 categories, such as RFEs or processes before diagnosis using ICD-10, may be useful in primary care clinics. Furthermore, ICPC-2 can be used at the end of outpatient care for reimbursement claims, such as care coordination, communication, or counseling with patients after care, and for payment reform with proper charges for these basic primary care services [25]. These efforts could result in more accurate data, enabling the administration of more effective treatments. These measures can also emphasize primary care areas such as prevention and counseling among patients and physicians. This can also improve the quality of primary care.
Our study has several limitations. First, we cannot generalize the results to other specialized clinics and countries. The participating physicians were limited to family medicine doctors working in specific areas in South Korea. However, previous studies conducted in other countries have also reported that ICD-10 could be inaccurate regarding atrial fibrillation and stroke [6,18]. Second, respiratory symptoms were the most common (i.e., cough, nasal symptoms, throat symptoms, and sputum) according to ICPC-2 in this study. These results might be because the survey spanned from October to November 2015, when respiratory diseases were prevalent. Third, the participation rate in this study was too low; therefore, there may have been selection bias. Further studies with larger sample sizes are required to confirm our results.
Despite these limitations, this study was the first to use ICPC-2 to prospectively analyze RFEs and healthcare services in primary care by trained investigators (doctors) while observing doctors’ medical care during visits.
In conclusion, our study demonstrated that ICD-10 does not accurately reflect actual primary care conditions. We also found that ICD-10 could be used for incidental purposes (claims for health insurance or suspected diagnoses) rather than for actual patient diagnoses. Thus, ICD-10 should be supplemented for diverse and subdivided patient care. Thus, introducing ICPC as a complementary means for diagnosing common diseases could be a solution to Korean primary care. Further studies are required to clarify the issues involved with the adoption of ICPC-2.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
This study was supported by National Evidence-based Healthcare Collaborating Agency (NECA-C-15-008) and the Korean Academy of Family Medicine.
Acknowledgements
We thank the National Evidence-based Healthcare Collaborating Agency (NECA) and the Korean Academy of Family Medicine for supporting this study.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4082/kjfm.22.0119.
Case report form used in this study
Questionnaire for primary care physicians used in this study
Classification status according to ICD-10 and ICPC-2 codes by body system
Physicians’ awareness of ICD-10 and ICPC-2.