Testing the Reliability and Validity of the Korean Version of the Pittsburgh Sleep Quality Index Using Fitbit Devices: A Cross-Sectional Analysis
Article information
Abstract
Background
Sleep disorders and insomnia are prevalent worldwide, with negative health outcomes. The Pittsburgh Sleep Quality Index (PSQI) is a widely used self-report assessment tool for evaluating sleep quality, comprising seven subdomains. The Korean version of the PSQI (PSQI-K) has been tested for reliability and validity in small sample sizes but lacks large-scale validation using objective measures.
Methods
This study was conducted with 268 Korean adults attending health check programs. Participants completed the PSQI-K questionnaire and wore Fitbit devices (Fitbit Inc., USA) to ascertain sleep parameters. Reliability was analyzed using the Cronbach’s α coefficient, and construct validity was determined through factor analysis. Criteria validity was assessed by correlating their index scores with Fitbit sleep parameters. We identified the optimal cutoff for detecting sleep disorders.
Results
The Cronbach’s α coefficient was 0.61, indicating adequate internal consistency. Factor analysis revealed three factors, explaining 48.2% of sleep quality variance. The index scores were negatively correlated with Fitbit sleep efficiency, total sleep time, and number of awakenings (P<0.05). The optimal cutoff point for identifying sleep disorder groups was ≥6.
Conclusion
The PSQI-K demonstrated good reliability and validity when correlated with Fitbit sleep parameters, offering a practical screening tool for identifying sleep disorders among Korean adults. Cutoff scores can help identify patients for sleep interventions. However, further large-scale studies are required to validate these findings.
INTRODUCTION
The prevalence of sleep disorders and insomnia has surged across diverse age groups [1]. The global sleep dynamics research estimates a 10%–20% occurrence of insomnia disorder within populations, with chronic symptoms in nearly half of the affected individuals [2]. Similarly, over one-fifth of adults experience sleep disorders in Korea [3]. Moreover, the incidence of insomnia has doubled over the last decade, emphasizing the need for effective assessment tools and interventions [4].
Accumulating evidence has underscored a correlation between compromised sleep quality and adverse health outcomes. Cardiovascular mortality, coronary heart disease, stroke, dementia, mental disorders, and metabolic syndrome are among the potential consequences of poor sleep quality [1]. A recent study even highlights associations between sleep disturbances in patients with Parkinson’s disease and alterations in white matter and functional networks, and cognitive impairments [5].
Evaluating sleep quality involves an interplay of factors, including sleep onset, maintenance, duration, and sense of revitalization upon awakening [6]. Sleep quality can be objectively and subjectively measured. Polysomnography, an objective method, is known to accurately collect sleep parameter data [7]. However, it is resource-intensive and has limited accessibility for clinicians, necessitating alternative approaches. Conversely, subjective self-rating questionnaires have the advantages of patient compliance, ease of administration, and reduced demands on healthcare personnel.
The Pittsburgh Sleep Quality Index (PSQI) is a widely utilized subjective sleep quality measure, encompassing seven key facets, including subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction [8]. The Korean version of the PSQI (PSQI-K) used in Korea [9] and also in this study assigns scores of 0–3 to each facet, resulting in a total score range of 0–21. Higher scores indicate poorer sleep quality. Notwithstanding its frequent application, discrepancies in interpreting PSQI scores—such as the use of subdomain cutoffs—have yielded suboptimal assessments of sleep disorders.
To address this gap, a previous study examined the reliability and validity of the PSQI-K in a small sample of young adults based on data from Fitbit devices (Fitbit Inc., San Francisco, CA, USA) [10]. However, the study lacks robustness as only a limited number of young adults in their 20s were tested. This study therefore aimed to comprehensively examine the reliability and validity of the PSQI-K through a relatively large-scale analysis of Korean adults. This evaluation was enhanced by objective sleep assessments using Fitbit devices, thus providing a broader perspective on sleep quality.
METHODS
1. Study Overview and Participants
This cross-sectional study included participants attending medical health check programs at two institutions: the Department of Family Medicine of the Gangnam Severance Hospital and Severance Health Checkup, Seoul, Korea, between December 2019 and December 2021. Each participant completed the PSQI-K questionnaire [8,9]. The PSQI-K questionnaire is presented in Supplement 1. Each participant wore a Fitbit device on their wrist—one of the most common wireless physical activity trackers estimating sleep parameters and stages in the consumer market [11-13]. Among the 280 participants who voluntarily participated in this study, we excluded 12 individuals who had missing data or did not complete the questionnaire. Subsequently, 268 participants were included in the analysis. Written informed consent was obtained from each participant.
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and approved by the Institutional Review Board of the Theragen Bio Institute (approval number: 700062-20190819-GP-006-02).
2. Measurement of Sleep Quality
The PSQI, developed by Buysse et al. [8], was translated into Korean by Shon et al. [9] to measure sleep quality. It is a self-administered questionnaire consisting of 19 questions designed to assess sleep quality during the previous month. Each item in the PSQI-K is scored from 0 to 3, where 0 and 3 indicate positive and negative extremes on the Likert scale, respectively. The global PSQI-K score is the sum of these items, with scores ranging from 0–21.
3. Measurement of Sleep Pattern
Sleep efficiency, total sleep time, sleep latency, and awakenings index were measured using Fitbit—a reasonable and reliable tool used to estimate sleep parameters [12,13]. Total sleep time implies the total time spent sleeping. Sleep latency refers to the time difference between lying in bed and actually falling asleep, and sleep efficiency is calculated as a percentage by dividing total sleep time by total bedtime. Number of awakenings during sleep refers to the number of awakenings from the start of sleep until immediately before the last awakening [14].
4. Statistical Analysis
The internal consistency reliability of the PSQI-K was analyzed using Cronbach’s α. For validity, a factor analysis was conducted using the varimax factor extraction and rotation method, and the number of factors was calculated using eigenvalues and factor loadings. Correlations between the total PSQI-K score and sleep efficiency, total sleep time, sleep latency, and awakenings index were analyzed using Spearman’s rho correlation coefficient. The optimal cutoff, reflecting the sensitivity and specificity for identifying the “sleep disorder group” based on the measured PSQI-K, was analyzed with the receiver operating characteristic (ROC) curve based on the Fitbit’s sleep efficiency index of ≤95%.
RESULTS
1. Characteristics of the Study Participants
The mean age of the participants was 46.5 years. Of the 268 participants, 62 (23.1%) were men and 206 (76.9%) were women.
2. Reliability
Table 1 presents the results of the reliability analysis of the PSQI-K. The criteria for calculating item-total correlation coefficients were set at ≥0.30, and the internal consistency coefficient was set at ≥0.60. Reliability testing of the PSQI-K revealed that the item-total correlation coefficient was 0.24–0.64, with all items except for the “use of sleep medication” item meeting the criterion of ≥0.30. The Cronbach’s α for the PSQI-K was 0.61.
3. Construct Validity
The results of the varimax principal component analysis and the factor rotation of the seven components of the PSQI-K tool are presented in Table 2. Three factors were derived: the first included two items—sleep duration and habitual sleep efficiency—accounting for 20.2% of the variance. Factor 2 included three items—sleep latency, sleep disturbance, and use of sleep medication—accounting for 15.3% of the variance. Factor 3 included two items—subjective sleep quality and daytime dysfunction—accounting for 12.7% of the variance. The total explanatory power (variance) of the model was 48.2%. Bartlett’s test of sphericity was 311.86 (degrees of Freedom=21, P<0.001), indicating that the factor analysis model was appropriate. Additionally, the Kaiser-Meyer-Olkin measure of sampling adequacy was 0.60, confirming that the extracted factors adequately explained the variables [15].
4. Criteria Validity
Table 3 presents the results of the correlation between the PSQI-K score and sleep efficiency, total sleep time, sleep latency, and awakenings index on Fitbit. The PSQI-K score was negatively correlated with Fitbit’s sleep efficiency, total sleep time, and awakenings index (r=-0.25, P<0.001; r=-0.14, P=0.024; and r=-0.16, P=0.012, respectively). However, PSQI-K score was not significantly associated with sleep latency (P=0.241).
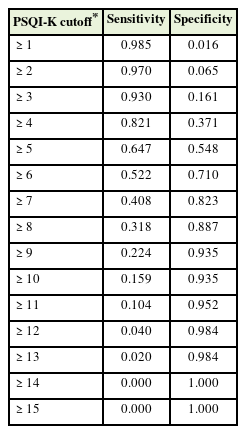
5. Sensitivity, Specificity, and the Cutoff
The results of the ROC curve analysis are presented in Table 4 and Figure 1. The PSQI-K cutoff for determining sleep disorders was ≥6—the most suitable for the sleep disorder group based on the sleep efficiency index of the Fitbit with a sensitivity of 0.52 and specificity of 0.71, and the area under the ROC curve was 0.66 (95% confidence interval, 0.58–0.73).
DISCUSSION
We verified the reliability and validity of the translated PSQI-K to evaluate subjective sleep quality and ascertain the optimal cutoff score for diagnosing sleep disorders in Korean adults. In this study, the reliability coefficient of the PSQI-K was 0.61, within the 0.6–0.8 standard for an adequate reliability coefficient. Cronbach’s α is a measurement that calculates the internal consistency of an assessment instrument [16]. In this study, the reliability coefficient of the PSQI-K was 0.61, which was lower than that of 0.84 reported by Shon et al. [9]. However, a Cronbach’s alpha value between 0.6 and 0.8 is deemed acceptable [16-18]. Thus, this study confirmed the acceptable reliability of the tool. The difference in Cronbach’s α between this study and that of Shon et al. [9] may be due to the use of polysomnography in their study [9], whereas Fitbit was used in this study.
An exploratory factor analysis was conducted to verify the construct validity of the PSQI-K. Among the seven subfactors, those with an eigenvalue of ≥1.0 and factor loadings of ≥0.60 were categorized into three factors, explaining 48.2% of sleep quality. This finding differs from those of Shon et al. [9] where a two-factor division was obtained. Construct validity pertains to how effectively a set of indicators represents or reflects a concept that is not directly measurable. Our approach involved examining the covariations of factors and their loadings on latent variables through an exploratory factor analysis. The resultant structural model revealed a three-factor structure. By employing factor rotation, the initial matrix was transformed into a simple structure matrix, enhancing interpretability. To this process, the varimax method was applied, assuming independence among factors and, consequently, zero inter-factor correlations. This method has the advantage of clearly distinguishing between factors, rendering interpretation more straightforward. In the evaluation of construct validity, the factors exhibited a distinct and well-defined latent meaning, facilitating a more straightforward interpretation.
The criterion validity of the PSQI-K was verified using indicators of sleep efficiency, total sleep time, sleep latency, and number of midnight awakenings measured using Fitbit trackers. The PSQI-K total score was weakly negatively correlated with Fitbit’s sleep efficiency (r=-0.25), total sleep time (r=-0.024), and number of midnight awakenings (r=-0.016), indicating a lack of validity compared to the study by Shin and Kim [10] This may be due to the differences in the characteristics of the study participants. While the study by Shin and Kim [10] had a small sample size comprising only young adults working in hospitals, the present study had a larger and more diverse study population encompassing various ages.
Fitbit uses accelerometers and heart rate sensors to estimate sleep stages (light, deep, and rapid eye movement sleep). While these can provide a good approximation, they may not be as accurate as data collected through polysomnography, which involves a more extensive array of sensors, including electroencephalography [19]. Moreover, there is a potential for error in the results due to environmental stimuli or user factors; hence, the user regularity with using the Fitbit during sleep should also be considered [12].
However, recent advances in wearable devices and big data analytics have made it possible to collect and analyze lifestyle and environmental data. An integrated analysis of these data can predict individual health risks, based on which appropriate management measures through active participation in healthcare behaviors can be encouraged. These measures are expected to prevent or delay the onset of diseases, thereby minimizing economic losses for individuals and society [20]. Therefore, this study, which evaluated the validity and reliability of the PSQI-K—a diagnostic tool for sleep disorders—using a simple and user-friendly wearable device compared to polysomnography—an existing diagnostic tool—is expected to have positive significance.
The optimal cutoff for distinguishing sleep disorder groups based on the PSQI-K total score was 6 points, which is consistent with previous studies. Thus, Korean adults with a PSQI-K total score of ≥6 can be screened as “poor sleepers,” which may be a useful criterion for identifying sleep disorder groups in research and clinical practice.
This study has several limitations. We did not consider the history of sleep disorders or sleep medication types—two factors that should be accounted for in future studies. In addition, participants were selected from only two hospitals; therefore, the study population may not be representative of the general Korean population. Further reliability and validity should therefore be confirmed through studies involving representative populations. Despite this study’s limitations, we verified the reliability and validity of the PSQI-K using Fitbit for a relatively large number of participants of various ages, As compared to a previous study which included a small sample size comprising only young adults working in hospitals [10].
In conclusion, the PSQI-K, which is frequently used as a screening tool for sleep disorders in Korean adults, was highly correlated with the Fitbit tracker, a simple objective measurement tool, in terms of sleep efficiency, total sleep time, sleep latency, and number of awakenings. The study also verified a cutoff for the PSQI-K to identify “poor sleepers,” which can be used as a more convenient tool for screening patients for sleep interventions.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
This research was supported by the Korea Institute of Planning and Evaluation for Technology in Food, Agriculture, and Forestry (IPET) through High Value-added Food Technology Development Program, funded by Ministry of Agriculture, Food and Rural Affairs (MAFRA) (grant number: 321030051HD030).
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4082/kjfm.23.0166.
Korean version of the Pittsburgh Sleep Quality Index.