Association Between Serum 25-Hydroxyvitamin D Levels and Dry Eye in Korean Adults: A Study Based on Korean National Health and Nutrition Examination Survey, 2010–2011
Article information
Abstract
Background
Dry eye is a common disease. Many patients continue to experience residual symptoms despite optimal treatment. Thus, new treatment options are required. The purpose of this study was to evaluate the association between serum 25-hydroxyvitamin D [25(OH)D] levels and dry eye.
Methods
This study was performed using data from the fifth Korean National Health and Nutrition Examination Survey, which is a cross-sectional study of the Korean population that was conducted from 2010 to 2011. We included adults aged >19 years who underwent ophthalmologic interviews and examinations. We excluded subjects who had comorbid conditions (rheumatoid arthritis, thyroid disease, chronic kidney disease, or depression) that are associated with dry eye. The subjects were divided into normal and dry eye groups. The dry eye group consisted of those who had clinically diagnosed dry eye syndrome or symptoms. Multiple logistic regression analysis was conducted to determine the association between serum 25(OH)D levels and dry eye.
Results
In the univariate model, the 25(OH)D levels were lower in the dry eye group than in the normal group (P=0.01). A significant association was found between severe vitamin D deficiency (<10 ng/mL) and dry eye (P=0.04). However, after multivariate adjustment, the statistical significance of the association disappeared (P-values= 0.49, vitamin D insufficiency; P=0.33, vitamin D deficiency; P=0.18, severe vitamin D deficiency).
Conclusion
Severe vitamin D deficiency was associated with dry eye in an unadjusted model, but the association was not statistically significant after adjustment.
INTRODUCTION
Dry eye is one of the most common eye diseases. Patients with dry eye experience chronic inflammation of the lacrimal gland and ocular surface, with high concentrations of several inflammatory mediators including cytokines and T-lymphocytes.12) Tumor necrosis factor (TNF)-α, interleukin (IL)-1, and IL-6 were detected in the conjunctivae of dry eyes.34) As it can lead to ocular discomfort, visual disturbance, fatigue, and decreased quality of life, dry eye is a significant public health issue.56)
The current treatment of dry eye is limited to artificial tears, topical lubricant, plugging of the lacrimal punctae, or topical anti-inflammatory treatment; further, inflammation of the ocular surface of the dry eye has been reduced by using antioxidants and omega-3.78) However, a large number of patients complain of residual symptoms even after the use of optimal medical therapies; therefore, an alternative treatment option is required.9)
Vitamin D, a fat-soluble vitamin, is produced in the skin after exposure to sunlight or is obtained via dietary intake. Vitamin D is activated by hydroxylation in the kidneys and liver. Activated vitamin D regulates calcium metabolism, and cell proliferation and differentiation; in addition, it is involved in the regulation of immune function and bone metabolism, and in the mechanism of pathogenesis of various cancers, immune diseases, and vascular diseases.101112) The anti-inflammatory effect of activated vitamin D is achieved by blocking the activation of T-helper cells and cytotoxic T cells, and reducing the production of inflammatory mediators such as IL-2, IL-6, IL-8, and IL-12.11121314) Furthermore, vitamin D inhibits inflammatory factors such as C-reactive protein, TNF-α, IL-1, and IL-6, and induces IL-10 production.1516) Therefore, it has been suggested that vitamin D may be used for the treatment of dry eye. However, studies investigating the association between vitamin D and dry eye are lacking. Therefore, this study aimed to evaluate the association between serum 25-hydroxyvitamin D [25(OH)D] levels and dry eye in Korean adults on the basis of data from the Korea National Health and Nutrition Examination Survey (KNHANES).
METHODS
1. Study Population
This cross-sectional study analyzed data consolidated from the years 2010 and 2011 of the KNHANES (2010–2012). The KNHANES has been conducted by the South Korea Centers for Disease Control and Prevention since 1998 and consists of the following three parts: health examination, health interview, and nutrition surveys. The survey was reviewed and approved by the institutional review board of the South Korea Centers for Disease Control and Prevention (2010-02CON-21-C, 2011-02CON-06-C).
The KNHANES (2010–2011) included 15,932 adults aged >19 years who underwent ophthalmologic interviews and examinations. After excluding 6,583 subjects with comorbid conditions (rheumatoid arthritis, thyroid disease, chronic kidney disease, or depression) that are associated with dry eye, 9,349 subjects were included in the analyses.
Evaluation of age, sex, monthly house income level, residential area, educational level, employment status, body mass index (BMI), comorbidity (hypertension, diabetes, and dyslipidemia), cigarette smoking, binge drinking, regular physical activity, sleep duration, sun exposure time, and history of eye surgery were included in the analyses. Binge drinking was defined as drinking >7 drinks in one place at least once per month for men, or drinking >5 drinks in one place at least once per month for women. Regular physical activity was defined as 30 minutes of moderate physical activity performed more than three times in a week.
2. Measurement of Vitamin D Level
Serum 25(OH)D levels were commonly used to represent vitamin D status because 25(OH)D is the most stable component of various forms of vitamin D in vivo. Serum 25(OH)D levels were measured using radioimmunoassay (1470 WIZARD gamma-counter; PerkinElmer, Turku, Finland). The serum 25(OH)D levels ranged from 4 to 51 ng/mL, and the values were divided into 4 groups17181920) as follows: severe vitamin D deficiency (<10 ng/mL), vitamin D deficiency (10–19 ng/mL), vitamin D insufficiency (20–29 ng/mL), and vitamin D sufficiency (>30 ng/mL).
3. Criteria for Dry Eye
The subjects were divided into 2 groups as follows: normal and dry eye groups. The dry eye group included patients with clinically diagnosed dry eye syndrome or symptoms. The normal group included those who answered “no” to the following questions: “Have you ever been diagnosed with dry eye syndrome by a physician?” and “Have you ever felt the symptoms of dry eye?” Subjects who responded “yes” to at least one of the questions were included in the dry eye group.
4. Statistical Analyses
We used complex sample analysis according to the statistical guidelines of the Korea Centers for Disease Control and Prevention for analyzing raw data from the KNHANES. To determine differences between the groups, we used chi-square tests to compare categorical variables and linear regression analysis to analyze continuous variables. Multiple logistic regression analysis was used to evaluate the association between serum 25(OH)D level and dry eye, and the results were reported as odds ratios (ORs) and 95% confidence intervals (CIs). Statistical significance was set at a P-value <0.05. The PASW SPSS software ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for all the analyses.
RESULTS
1. Baseline Characteristics of the Study Subjects
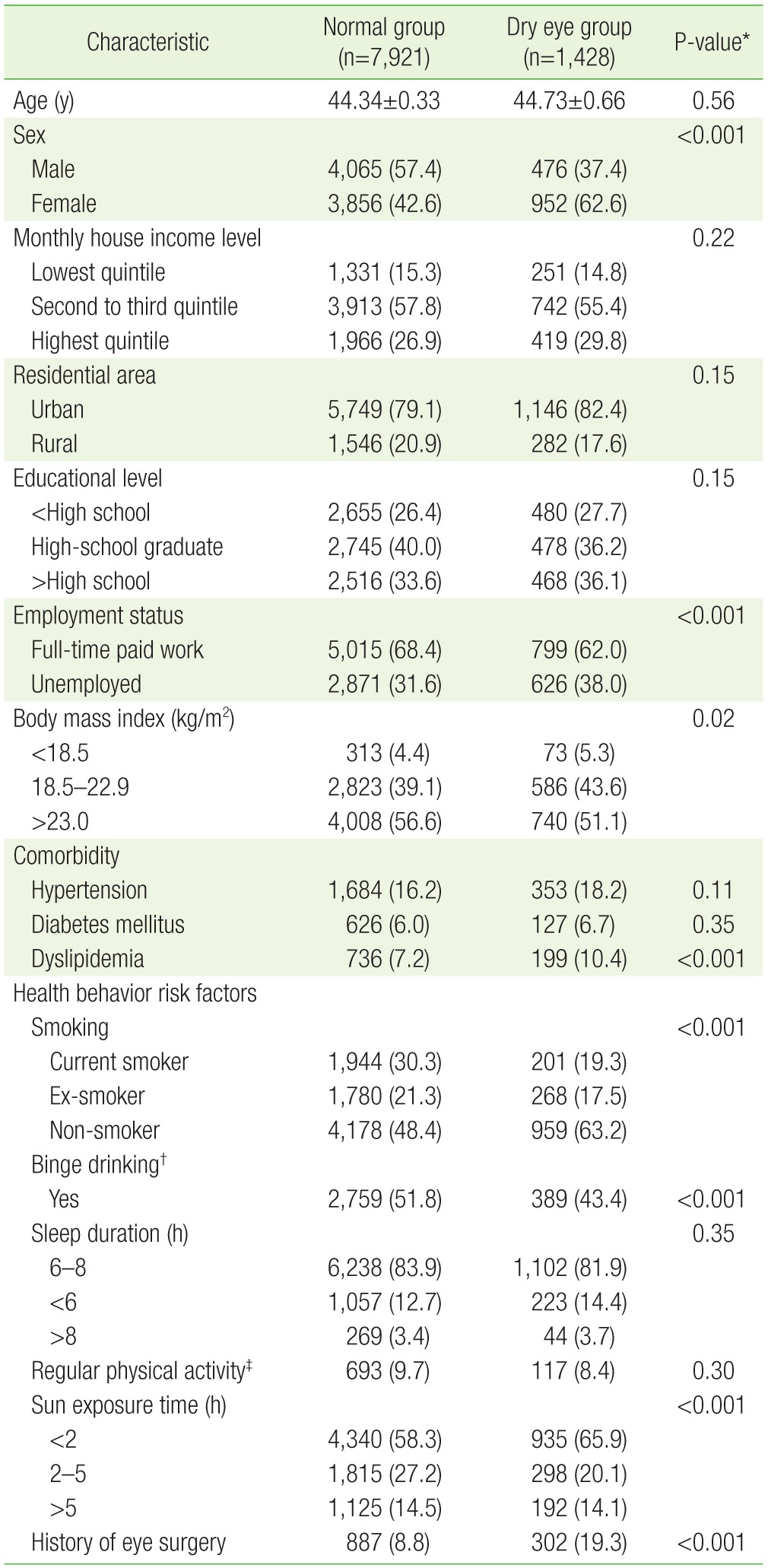
Of the 9,349 subjects, 7,921 were assigned to the normal group (mean age, 44.34±0.33 years) and 1,428 were assigned to the dry eye group (mean age, 44.73±0.66 years). The sex distribution was significa different between the groups (normal group: 57.4% men and 42.6% women; dry eye group: 37.4% men and 62.6% women; P<0.001). The frequency of full-time paid work was significantly higher in the normal group (68.4%) than in the dry eye group (62%, P<0.001).
The distribution of BMI was significantly different between the groups (normal group: 4.4%, <18.5 kg/m2; 39.1%, 18.5–22.9 kg/m2; 56.6%, >23.0 kg/m2; dry eye group: 5.3%, <18.5 kg/m2; 43.6%, 18.5–22.9 kg/m2; 51.1%, >23 kg/m2; P=0.02).
The distribution of smoking status was significantly different between the groups (normal group: 30.3% current smokers, 21.3% exsmokers, and 48.4% non-smokers; dry eye group: 19.3% current smokers, 19.5% ex-smokers, and 63.2% non-smokers; P<0.001). The frequency of binge drinking was significantly higher in the normal group (51.8%) than in the dry eye group (43.4%, P<0.001). The distribution of subjects with sun exposure time was significantly different between the groups (normal group: 58.3%, <2 hours; 27.2%, 2–5 hours; 14.5%, >5 hours; dry eye group: 65.9%, <2 hours; 20.1%, 2–5 hours; 14.1%, >5 hours; P<0.001). The percentage of subjects with a history of eye surgery was significantly lower in the normal group (8.8%) than in the dry eye group (19.3%, P<0.001). Other general characteristics were not significantly different (Table 1).
2. Serum 25(OH)D Levels
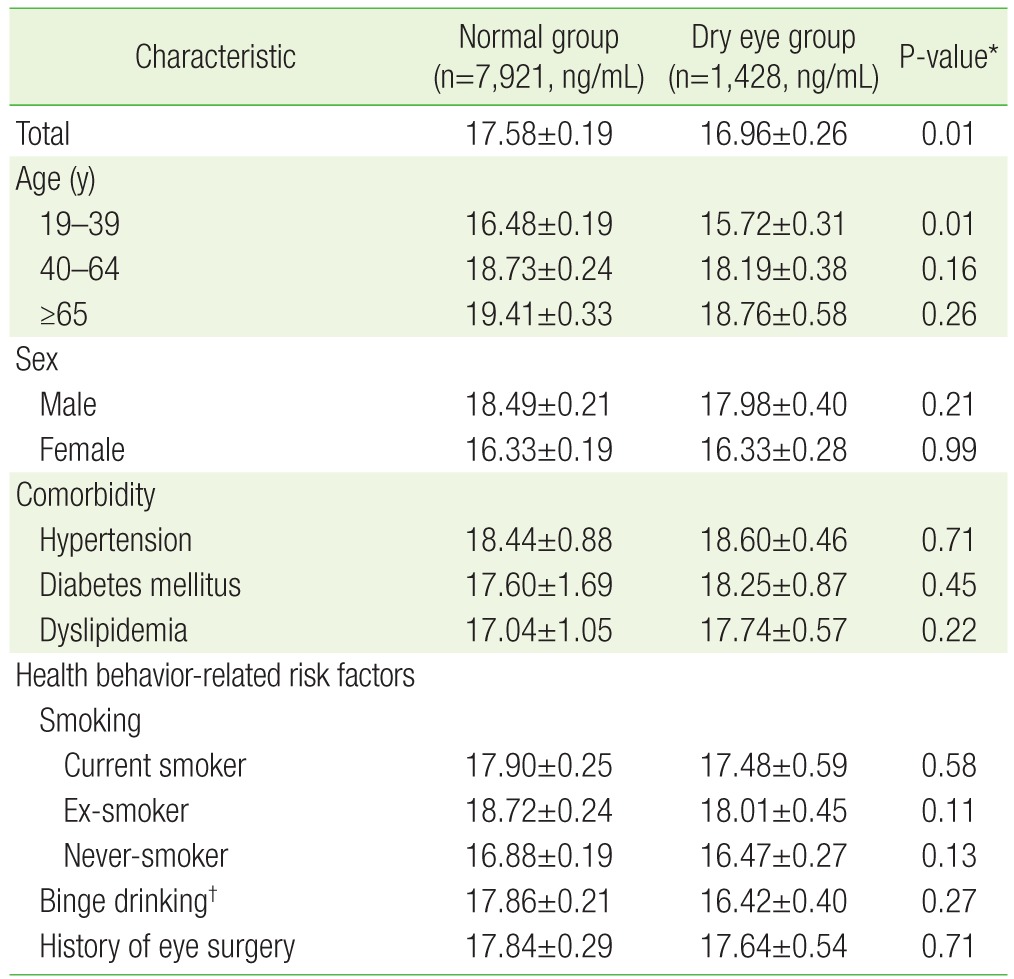
The serum 25(OH)D level in the normal group (17.58±0.19 ng/mL) was significantly higher than that in the dry eye group (16.96±0.26 ng/mL, P=0.01). In addition, the serum 25(OH)D level of those aged 19–39 years was significantly higher in the normal group (16.48±0.19 ng/mL) than in the dry eye group (15.72±0.31 ng/mL, P=0.016). Serum 25(OH) D levels were not significantly different for any other variables (Table 2).
3. Relationship between Serum 25(OH)D Level and Dry Eye
OR was 1.20 (95% CI, 0.77 to 1.86) for vitamin D insufficiency, 1.453 (95% CI, 0.95 to 2.21) for vitamin D deficiency, and 1.61 (95% CI, 1.00 to 2.61) for severe vitamin D deficiency in the crude model. Compared with vitamin D sufficiency, a lower serum 25(OH)D level was associated with an increased risk of dry eye. In particular, severe vitamin D deficiency was significantly correlated with dry eye (OR, 161; 95% CI, 1.00 to 2.61) (Table 3).
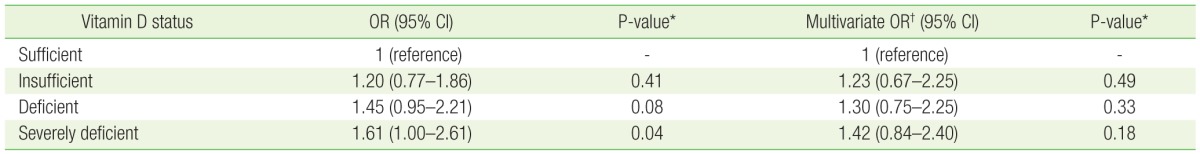
Logistic regression analysis model for the unadjusted odds of dry eye based on vitamin D levels, and model 2 for the adjusted odds of dry eye based on vitamin D levels
OR was 1.24 (95% CI, 0.66 to 2.41) for vitamin D insufficiency, 1.30 (95% CI, 0.75 to 2.25) for vitamin D deficiency, and 1.42 (95% CI, 0.83 to 2.41) for severe vitamin D deficiency after adjusting for age, sex, BMI, smoking, binge drinking, sun exposure time, and history of eye surgery. Vitamin D level tended to decrease as the risk of a diagnosis or symptoms of dry eye increased. However, the OR for vitamin D status did not significantly correlate with dry eye (Table 3).
DISCUSSION
In the present study, in which the association between serum 25(OH) D level and dry eye was evaluated using data from the KNHANES-V (2010–2011), the serum 25(OH)D level (17.58±0.19 ng/mL) in the normal group was significantly higher than that in the dry eye group (16.96±0.26 ng/mL). This study was performed in Korean adults older than 19 years who had no medical history of disease associated with dry eye (rheumatoid arthritis, thyroid disease, chronic renal failure, and depression; P=0.01). In addition, the OR of severe vitamin D deficiency for dry eye was 1.61 (95% CI, 1.00 to 2.61; P=0.04). However, in the adjusted model, this was not statistically significant.
In a previous study, each 10-ng/mL increase in serum vitamin D levels, measured using 25(OH)D, was associated with a significant decrease in dry eye symptoms, as assessed using the 5-item dry eye questionnaire and tear film parameters.9) Moreover, in the same study, Mediterranean diet had an effect to improve systemic inflammatory markers.
Further, Yildirim et al.21) reported an association between dry eye and impaired tear function in patients with vitamin D deficiency, similar to the results of the present study, in which the dry eye group had significantly lower serum 25(OH)D levels than the normal group (P=0.01). Moreover, a lower serum 25(OH)D level was associated with an increased risk of dry eye, particularly in case of a severe vitamin D deficiency (OR, 1.61; 95% CI, 1.00 to 2.61; P=0.04). However, after adjusting for age, sex, BMI, smoking, binge drinking, sun exposure time, and history of eye surgery, this was not statistically significant (OR, 1.42; 95% CI, 0.84 to 2.40; P=0.18).
This study has certain limitations. First, dry eye syndrome and symptoms were diagnosed using only a simple questionnaire rather than subjective symptoms, physical examination results, or abnormal test results. Second, although seasonal variations can affect serum 25(OH)D levels, the present study did not consider this variable. Third, as this study was conducted only on Korean population, it is difficult to apply our findings in the general population. Fourth, our statistical methods or variables might have been different from those used in previously conducted studies. Finally, the cross-sectional nature of this study did not allow for evaluation of the cause-and-effect relationship between serum 25(OH)D level and dry eye. Our study results could have errors due to these limitations. Therefore, further prospective cohort studies are needed.
However, this study has several strengths. It is the first to investigate the association between vitamin D level and dry eye in adults using data from the KNHANES, which is a large-scale survey representing the Korean general population. Although our results showed that the serum 25(OH)D level in the normal group was significantly higher than that in the dry eye group, in Korean adults older than 19 years, we did not find a significant association between serum 25(OH)D level and dry eye after adjustment for various confounding factors.
In conclusion, the present study revealed no significant association between vitamin D level and dry eye. Further studies are needed to confirm the relationship.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.