Trajectories of Handgrip Strength and Their Associations with Mortality among Older Adults in Korea: Analysis of the Korean Longitudinal Study of Aging
Article information
Abstract
Background
Handgrip strength (HGS) is a good predictor of adverse health outcomes in later life. This prospective study aimed to investigate whether HGS trajectory patterns were associated with all-cause mortality among older adults in Korea.
Methods
This study used the database of the 2006–2016 Korean Longitudinal Study of Aging. Study participants included 3,069 adults aged ≥65 years without a previous history of cancer. The trajectory model was developed to identify different homogeneous trajectory patterns of HGS according to study period. Cox proportional hazards models were then applied to investigate the association between HGS and all-cause mortality.
Results
The survival probability according to HGS during the follow-up period decreased as base HGS weakened. We identified four distinct trajectory groups of HGS among men and three among women. The risk of mortality increased as the HGS of both males and females decreased. Compared with the highest HGS group, the adjusted hazard ratios for all-cause mortality of the lowest, lower-mid, and upper-mid HGS groups among males were 3.46 (95% confidence interval [CI], 2.17–6.69), 2.26 (95% CI, 1.47–3.48), and 1.58 (95% CI, 1.07–2.32). Those of the low and mid HGS groups among females were 2.69 (95% CI, 1.39–5.21) and 1.97 (95% CI, 1.05–3.69).
Conclusion
The faster HGS declined over time, the greater the all-cause mortality risk increased compared with the slowly decreasing or maintained HGS groups among men and women. HGS measurement among older adults will be helpful in assessing their health statuses and pre-assessing disease-associated morbidity.
INTRODUCTION
The proportion of the older adult population in Korea increased to over 7% in 2000, and the country entered the era of an aging society [1]. The proportion of the older adult population has increased rapidly, and by 2026 Korea will have a post-aged community (individuals older than 65 years will make up more than 20% of the total population) [1]. Health problems of older adults are becoming significant social problems, and the burden of medical expenses is also increasing rapidly [2]. In this regard, it is essential to assess the health statuses of older adults accurately and to predict possible risks.
Several tools have been studied and developed to evaluate physical activity and health status among older adults. The assessment of and changes in muscle strength are known to be essential indicators of adverse outcomes [3]. Handgrip strength (HGS) is a measure of overall muscle strength and is known to be associated with mortality and morbidity [4]. HGS measurement is an easy, simple, and inexpensive method that can be used extensively to stratify the risk of mortality and death from aging [5]. It is known that the HGS decreases at a certain rate with increasing age. Measuring these changes over time is important in predicting the degree of decrease in the overall function of the body [6,7].
Recent systematic reviews have shown that baseline HGS is associated with early mortality, the risk of morbidity, and the incidence of complications [8]. Previous studies conducted in Korea have focused on the relationship between HGS and osteoporosis, fracture, cognitive dysfunction, and depression. However, there is little research on the correlation between mortality and HGS [9,10].
Moreover, studies that used the rate of change in grip strength as a predictor of mortality have yielded mixed results [4,11,12]. A previous study used the absolute change in HGS to model longitudinal data in survival analysis with only two consecutive HGS assessments [13]. In the Baltimore Longitudinal Study of Aging, the rate of change in grip strength in men aged <60 years was found to be more important for long-term mortality than the initial level, while for men aged ≥60 years, higher baseline grip strength but not the slope predicted longer survival over a 40-year period [11].
Therefore, we aimed to investigate the changes in HGS over 10 years and its effects on mortality among community-dwelling older adults using the database of the Korean Longitudinal Study of Aging (KLoSA). To determine the changes in HGS more accurately, a trajectory model was developed to identify different homogeneous trajectory patterns of HGS according to study period.
METHODS
1. Data and Study Sample
The present study was based on the database of the KLoSA, an ongoing longitudinal panel survey of community-dwelling older adults in Korea aged ≥45 years. It was first conducted in 2006 with biennial follow-ups, and six follow-up surveys had been completed by 2016. This biennial survey involves multistage, stratified sampling based on geographic areas. The KLoSA survey includes questionnaires on demographics, health status, marital status, level of education, and grip strength. In the first baseline survey conducted in 2006, 10,254 participants from 6,171 households were interviewed by trained interviewers using the Computer-Assisted Personal Interviewing technique. In the follow-up surveys until the sixth, the original panel retention rate showed a stable trend at 78%, and the number of valid samples that could be analyzed was 6,618. The KLoSA database also includes data on deaths. Since 2008, deaths have been reported at intervals of 2 years; data regarding the date, cause, and place of death and past medical history of dead persons are collected.
Our study analyzed the 2006 baseline interview data of 3,069 participants aged ≥65 years. All participants provided written informed consent, and the survey protocol was approved by the Institutional Review Board of Statistics Korea. Among the 10,254 participants of the KLoSA in 2006, 7,185 were excluded due to age (<65 years) and those who had been diagnosed with cancer were also excluded. We also excluded those who underwent HGS measurements only once during follow-up. To investigate the association between HGS and all-cause mortality among these individuals, we finally included 3,069 (1,317 men and 1,752 women) study subjects at the baseline. During the 10-year follow-up period, 696 subjects died (22.7%), of whom 385 (55.3%) were men and 311 (44.7%) were women.
2. Measurements
The education level was classified on the basis of the final education level as follows: below elementary school, middle school, high school, and college and higher. Marital status was categorized as living with and not living with a spouse. The status of not living with a spouse included divorce, bereavement, and separation for a variety of reasons, such as long-term accommodation and long stays abroad.
Subjects with chronic illness were assessed for the presence of hypertension, diabetes mellitus (DM), chronic lung disease, chronic liver disease, heart disease, and stroke. The subjects were classified according to smoking status as non-smokers, former smokers, and current smokers. Former smokers were defined as those who did not smoke at present but had consumed more than 5 packs of cigarettes in the past. Subjects were classified according to alcohol consumption as non-drinkers, former drinkers, and current drinkers. Subjects who drank usually or frequently or recently were classified as “current drinkers.” Non-drinkers were classified as “non-drinkers” who did not drink usually but drank initially, and others as “former drinkers.” According to the activity level, we defined an exercise group, comprising those who exercised regularly at least once a week, and a non-exercise group. Body mass index (BMI) was evaluated by dividing the body weight by the square of the height (kg/m2) and the degree of obesity was evaluated on the basis of BMI. BMI of 30 kg/m2 or higher was classified as severe obesity, 25–29.9 kg/m2 as obesity, 23–24.9 kg/m2 as overweight, 18.6–22.9 kg/m2 as normal, and ≤18.5 kg/m2 as low weight. The cognitive function of participants was assessed using the Korean version of the Mini Mental Status Examination (MMSE), which is widely used to screen for the cognitive impairment of older adults in Korea. Depression was assessed using the 10-item short-form Center for Epidemiological Studies-Depression scale, a screening tool for evaluating depression. Subjects were classified according to self-rated health. In the survey, subjects were asked to check five items (very good, good, normal, poor, and very bad) about subjective health status, which were then classified into three items (good, moderate, and bad). HGS was assessed using a handgrip dynamometer (TANITA Hand Grip Meter Blue 6103; Tanita Co., Tokyo, Japan). The grip strength of both hands was measured twice using a dynamometer, and the average value was used. The average values of grip strength were divided into three groups among women and four groups among men.
3. Statistical Analysis
We analyzed the baseline characteristics of the participants by sex. The baseline characteristics of the study participants were assessed using analysis of covariance. The values are expressed as means±standard error or as percentages.
Group-based trajectory modeling had been designed to classify a population into distinct subgroups based on the patterns of HGS. We used the ‘traj’ command of the Stata procedure to select group-based modeling. Using this approach, we could identify relatively homogeneous clusters of developmental trajectories within a sample population. The model selection procedure with ‘traj’ is an iterative model-fitting and decision process that requires both statistical and subjective determinations. We followed a two-stage model selection process suggested by Nagin [13], whereby the number of trajectory groups was determined in the first stage and the best polynomial trajectory function was determined, and the Bayesian information criterion (BIC) value was calculated in the second stage. We selected the final best model with the lowest absolute BIC value [14], and in making this selection, clinical knowledge and group size (e.g., whether a group was reasonably large [>5%]) were also considered [14].
We used Cox proportional hazards models to investigate the association between trajectory patterns for HGS and all-cause mortality. Cox proportional hazards regression models were used to identify the likelihood of death according to the degree of HGS. For samples that satisfied the inclusion criteria, a complex sample file was constructed by applying weights to the sample, and a complex Cox regression analysis was performed. Two Cox proportional hazards regression models were constructed to evaluate the relationship between trajectory patterns for HGS and mortality. Model 1 was adjusted for age, BMI, hypertension, DM, chronic lung disease, chronic liver disease, stroke, and self-rated health. Model 2 was adjusted for the same variables as model 1 plus level of education, marital status, smoking, alcohol consumption, regular exercise, activities of daily living, MMSE, and depression. All analyses were performed using Stata/MP ver. 13.1 for Windows (Stata Corp., College Station, TX, USA). Analysis items with a P-value of <0.05 were considered statistically significant.
RESULTS
The baseline characteristics of the study participants by sex are presented in Supplementary Table 1. Among the participants, 42.9% were men and 57.1% were women. The mean age was 71.6±0.1 years among men and 72.3±0.1 years among women (P<0.001). Regarding chronic diseases, chronic lung disease and stroke were more frequent among men (P<0.001) and hypertension was more frequent among women (P<0.001). A higher proportion of women had two or more diseases (P<0.001). Regarding self-rated health status, a significantly higher proportion of women rated their health as bad (P<0.001). The proportion of participants with elementary school education or below was higher among women (86.0%) than among men (52.1%). A significantly higher proportion of men than women lived with a spouse, drank and smoked frequently, and exercised regularly.
According to the degree of HGS, four groups of male subjects (the low HGS, lower-mid HGS, upper-mid HGS, and high HGS groups) and only three groups of female subjects (the low HGS, mid HGS, and high HGS groups) were assessed because division into four groups yielded one group that comprised less than 5% of the entire group and had no statistical significance among women.
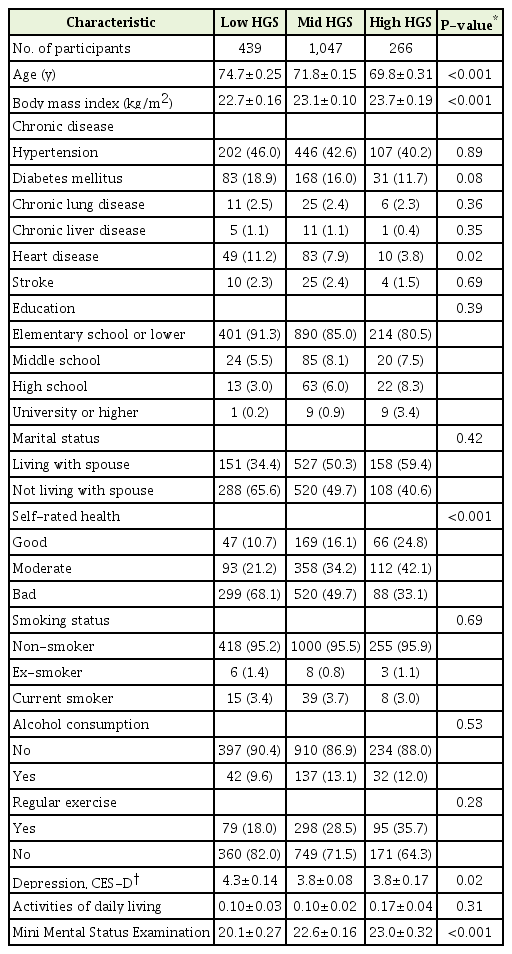
The characteristics of men by HGS trajectory are shown in Table 1. The mean age of the group with higher HGS was lower and the mean BMI was higher (P<0.001). The subjective assessment of their health status was better (P<0.001) and the mean MMSE score was significantly higher in the high HGS group (P<0.001).
The characteristics of women by HGS trajectory are shown in Table 2. As observed among men, the mean age was lower among women with higher HGS and the mean BMI was higher (P<0.001). Self-rated health and the MMSE score were better in the higher HGS group.
The change in HGS among participants during the study period is shown in Figure 1. Among participants in the high HGS group, the HGS was maintained or increased among women over time, while the grip strength of the middle HGS and low HGS groups decreased gradually with time. Both men and women showed a greater decrease in the low HGS group.
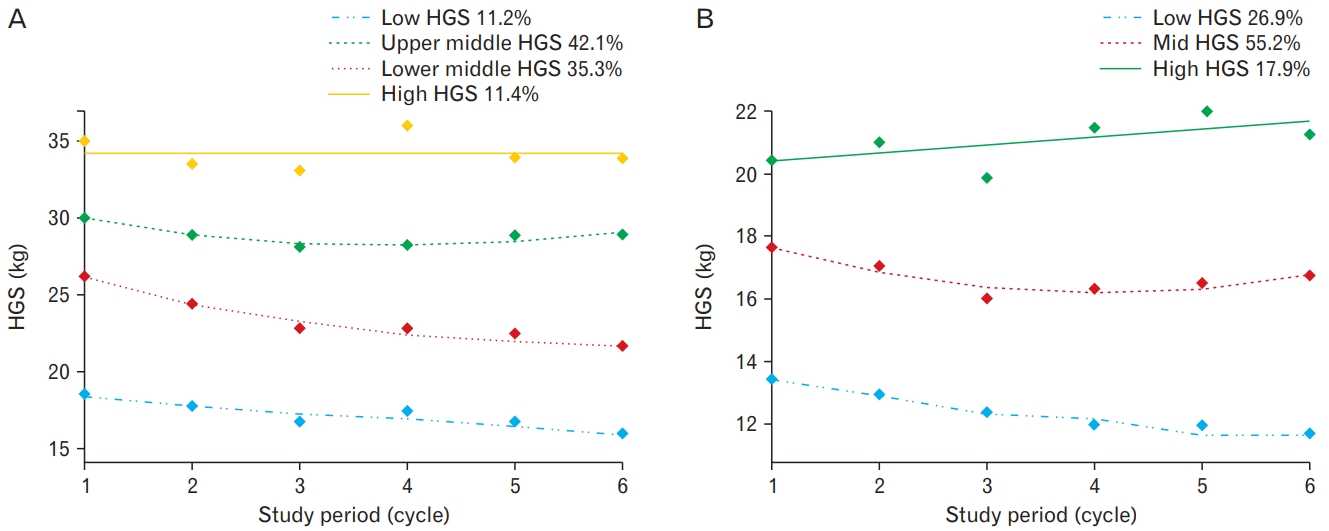
Handgrip strength (HGS) trajectories of the participants during the study period for men (A) and for women (B). In the high HGS group among males, HGS was maintained during the study period while it decreased gradually in the low HGS group (P<0.001).
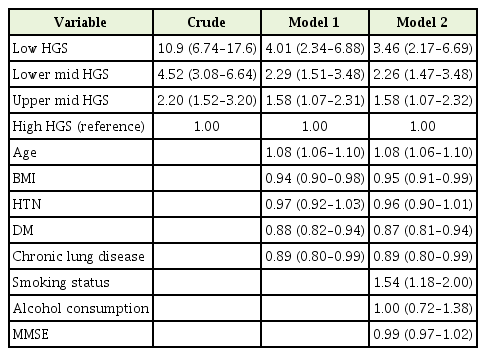
Table 3 shows the Cox proportional hazard ratio (HR) of all-cause mortality associated with HGS trajectories among men, and the data were adjusted for confounding variables (age, BMI, comorbidities, self-rated health, education, marital status, smoking, alcohol consumption, regular exercise, MMSE, and depression). The HR of the low HGS group was 10.9 (95% confidence interval [CI], 6.74–17.6) and the adjusted HR was 3.46 (95% CI, 2.17–6.69) after adjusting for cofounding variables. Among the various variables analyzed in model 2, factors associated with mortality were age, comorbidities (hypertension, DM, chronic lung disease, chronic liver disease, heart disease, and stroke), marital status, and smoking.
Table 4 shows the Cox proportional HR of all-cause mortality associated with HGS among women. The crude HR of the low HGS group was 6.61 (95% CI, 3.87–11.30) and the adjusted HR was 2.69 (95% CI, 1.39–5.21) compared with the high HGS group. The analysis of model 2 showed that age and DM were related to mortality.
The Kaplan-Meier survival curves presented in Figure 2 showed a better overall survival probability in the groups with stronger HGS among both women and men.
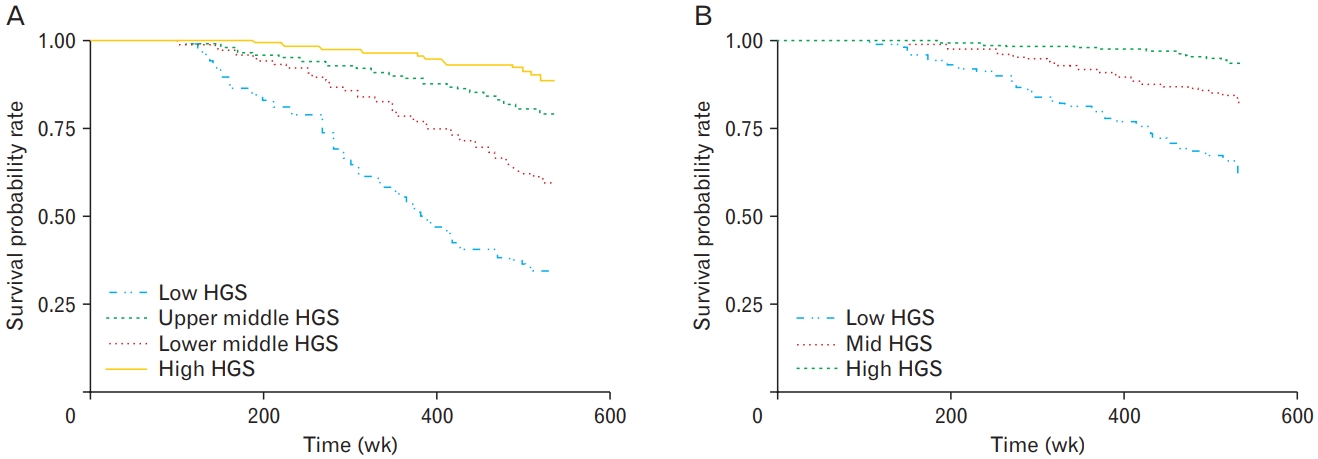
Kaplan-Meier survival curves stratified by Handgrip strength (HGS) for men (A) and for women (B). Among both men and women, the overall survival probability was better in the groups with strong HGS (P<0.001).
We performed a subgroup analysis by selecting only those with an above-average HGS at the baseline to further assess the association of mortality with changes in HGS trajectory among healthy subjects. Both male and female subjects were selected along three trajectory patterns of groups, and the HRs of mortality were significantly higher in the high trajectory group than the low trajectory group in both sexes (males: HR, 2.94; 95% CI, 1.14–7.60; females: HR, 3.80; 95% CI, 1.10–13.10) (Supplementary Table 2).
DISCUSSION
Using data from a 10-year follow-up study of the nationwide Korean community-dwelling population, we demonstrated that the faster HGS declined over time, the greater was the risk of all-cause mortality compared with the group with slowly decreasing or maintained HGS among both men and women, even after adjustments for other risk factors. In addition, among those with an above-average HGS at the baseline, the risk of mortality also increased in the group with decreasing HGS over time in both men and women.
Wu et al. [7] in 2017 found that HGS was an independent predictor of all-cause mortality and cardiovascular diseases in a meta-analysis study of the relationship between HGS and all-cause mortality, cardiovascular disease, and cancer in community-dwelling populations. Park et al. [15] in 2019 assessed 13,901 persons from 2008 to 2011 for HGS, depression, and all-cause mortality and found that the risk of mortality was higher in the lower HGS group at the baseline. However, in these prospective studies, HGS was determined on the basis of measurements at baseline examination only. Possible changes in HGS levels during the follow-up period were not taken into consideration.
Our study differed in that we used repeated-measures data on HGS from a 10-year longitudinal study. Using a trajectory model, we identified four distinct trajectory patterns for men and three for women older than 65 years. These trajectories showed parallel declines throughout the study period. HGS decreased significantly as age increased and differed among the sexes.
Subjects in the group that experienced a slow decline in HGS was younger, more educated, weighed more, and exercised more regularly than those that experienced a fast decline. The former tended to live with a spouse and had better self-related health perception, good cognitive function, and less depression than the latter. However, our findings showed that the association of HGS with mortality remained significant after adjusting for these confounding factors.
Through repeated measurement of HGS during the study period, we proved the association between HGS and mortality more precisely, beyond the limits of measurement error that could be obtained using only one measurement. In addition, the present study was conducted in a nationwide population, and the patterns of HGS decline among older adult Koreans over time could be presented for both men and women. This study showed once again the importance of steady maintenance of the physical performance represented by HGS in the older adult population, which is hard to reveal in studies using onetime measurements of HGS.
Although it is well known that grip strength decreases with age [6], there have been few studies of the direct or indirect association of mortality with changes in grip strength over time. In Japan, Taniguchi et al. [6] showed a decrease in HGS over time in both male and female groups. The high HGS group showed a higher rate of regular exercise, suggesting that prevention of muscle strength reduction through regular exercise is important in the older adult population as well [16,17]. This finding is consistent with the results of our study. However, we have shown through subgroup analysis that the rapid decline in HGS can predict future mortality, even among those with above-average HGS at the baseline. Even among subjects with well-preserved HGS at the baseline, this suggests that the maintenance of physical performance is important for the prevention of future mortality.
In our study, the HGS among women in the higher HGS group increased slightly during the study period. This implies that muscle power and physical performance were relatively well preserved in that group. On the other hand, this observation might result from sampling bias or measurement bias regarding HGS during the study period.
Although the precise mechanism underlying the correlation between HGS and mortality is not yet known, several studies have confirmed that sarcopenia associated with aging is associated with mortality. Among older adults, it is known that sarcopenia increases the risk of cardiovascular disease and is related to the risk of type 2 DM and falls [18-20]. Sarcopenia reflects weaker whole-body muscle strength, which is known to be associated with traditional risk factors for death or cardiovascular disease, that is, lower body weight [21], physical inactivity [22], and chronic diseases, such as diabetes and hypertension [23]. HGS is a very simple but closely related method of measuring the degree of sarcopenia among older adults, which supports the results of our study [24].
In one population study, a positive correlation of HGS with the serum concentration of insulin-like growth factor 1 (IGF-1) was reported [25]. IGF-1 is a key regulator of muscle cell proliferation and differentiation and an inhibitor of cell apoptosis and necrosis [26]. Decreased IGF1 level is related to insulin resistance [27], type 2 diabetes [28], ischemic heart disease [29], and mortality [30].
The present study had several strengths that should be highlighted, such as its large community sample size, the prospective design (10-year period of follow-up), HGS, and physical assessments using validated measures, and availability of data on several lifestyle and health variables. In addition, since the study was carried out only among healthy residents in Korea, the current findings can be generalized to the Korean population. Moreover, we conducted our analysis after adjusting for multiple sociodemographic variables including age, gender, education level, comorbidities, obesity, smoking, alcohol consumption, and cognitive status.
However, the study also had a few limitations that should be acknowledged. First, we were limited to self-reported health conditions and did not use biomarkers to describe a common mechanism of muscle mass reduction with age. Second, we adjusted for age and other variables in the analysis; however, age was inversely related with the HGS, and may have a greater impact on mortality in the higher HGS group. Third, only deaths from all causes were assessed. Further research is needed to investigate the association of HGS trajectory with cause-specific mortality, such as cardiovascular and other-cause mortalities.
Nonetheless, to our knowledge, the present study is the first to demonstrate the longitudinal and independent relationship of trajectories of HGS with all-cause mortality among older Korean adults, controlling for various covariates. In conclusion, this prospective study showed that lower HGS over time is a significant risk factor for mortality among older Korean adults. However, further studies are needed to determine the mechanism underlying the correlation between decreased HGS trajectory and mortality.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported by Wonkwang University in 2019.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4082/kjfm.19.0140.
Baseline characteristics of study participants according to sex.
Cox proportional HR of mortality according to HGS trajectories of those with an above-average HGS at baseline.