 |
 |
- Search
| Korean J Fam Med > Volume 32(5); 2011 > Article |
Abstract
Background
The purpose of the present study was to investigate the relation between the extent of bladder distention and the rise of blood pressure in middle aged women.
Methods
In a cross-sectional, descriptive observational study, we obtained data from 172 middle aged women at a health promotion center of Pusan National University Hospital. We measured duration of urine-holding as the degree of the extension of bladder distention. Blood pressure was measured twice while holding urine and immediately after urination. Urine holding with full bladder was confirmed by abdominal ultrasound.
Results
Difference in systolic blood pressure was 4.2 ┬▒ 10.7 (P < 0.001), and that in diastolic blood pressure was 2.8 ┬▒ 7.7 mm Hg (P < 0.001) between holding urine and immediately after urination. There was no significant correlation between the urine-holding duration and differences in systolic and diastolic blood pressure.
O'connor1) observed that blood pressure (BP) fell after prostatic obstruction was relieved. Distension of the bladder has been also shown to cause a rise in BP in anaesthetized dogs and cats, and patients with spinal cord injuries.2-4) Szasz and Whyte5) reported that diastolic and systolic BP rose in seven normal volunteers, and four patients who were in relatively good general condition at the height of bladder distension during the course of the oral fluid load and retrograde filling tests. Scultety et al.6) also observed that BPs were significantly elevated in ten healthy volunteers aged 21 to 56 years when their bladders were uncomfortably full or after excess fluid loading. In all instances, it seemed that the distension of bladder is a factor to elevate BP. However, previous studies were conducted on a small number of patients and the practical significance in the association between the extent of bladder distension and the rise of BP was not assessed. As reported in the literature, the prevalence of hypertension increased with aging. In women, the change was particularly marked after menopause.7) Accurate measurement of BP is necessary for the diagnosis of hypertension. Thus American Heart Association reported factors including bladder distension that can affect the measurement of BP, but it did not suggest any specific guidelines about bladder distension.8) Thus, the purpose of the present study was to investigate the relation between the extent of bladder distention and the rise of BP.
In a cross-sectional, descriptive observational study, we obtained data from 172 middle aged women aged 40 to 60 years at a Health Promotion Center of Pusan National University Hospital. Patients who had been diagnosed hypertension with anti-hypertensive medication, cardiovascular diseases, diabetes, cancer, liver disorders, abnormal urological condition, or taking any medication affecting BP were excluded. Patients with hypertension without anti-hypertensive medication were included in this study.
Urination normally occurs every 3-4 hours, thus BP was measured at least 3 hours after the patients had the last urination. Abdominal ultrasound was performed to determine whether a participant has a full bladder with a bladder volume of 400 to 600 mL.9) The ultrasound instrument used was the Bladder Scan BVI 2500 (Diagnostic Ultrasound Corporation, Redmond, WA, USA). This is a portable battery-operated machine consisting of a handheld scanner and a small instrument box with a screen for digital display. It contains software that automatically computes bladder volume using the bladder's front and back wall locations. BP was measured after the participants took at least 5 minutes of the rest in a chair with their backs supported and their arms bared and supported at heart level, following recommendations of JNC VII.10) Participants were refrained from smoking or ingesting caffeine for 30 minutes preceding the measurement. Measurement of BP was performed during urine-holding and after urination by a skilled nurse using a validated oscillometric automatic BP monitor (BP203RV-II; Nippon Colin, Komaki, Japan).11,12) Duration of urine-holding was defined as the time taken from the last urination until BP measurement.
Systolic and diastolic BPs before and after urination were compared by paired t-test. BP was classified according to the recommendation of the JNC VII report.10) Changes in classification of BP before and after urination were analyzed by Friedman test for repeated measurements. All P-values are two sided, and P < 0.05 was considered statistically significant.
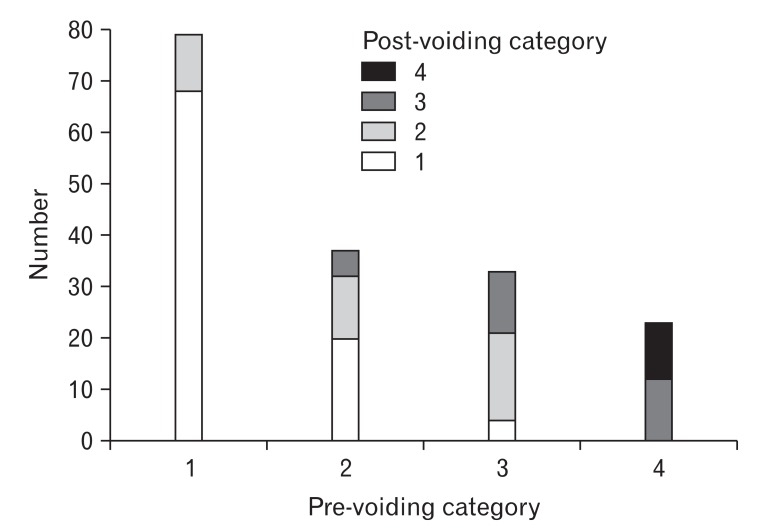
Participants had an average age of 54.5 (┬▒ 9.9) years and an average body mass index (BMI) of 23.9 (┬▒ 2.8) kg/m2. Their duration of holding-urine ranged from 3 to 15 hours (7.0 ┬▒ 3.4 hours). Systolic and diastolic BPs were 124.2 ┬▒ 20.8 and 78.3 ┬▒ 13.3 mm Hg while subjects had been holding urine for at least 3 hours since the last urination, but decreased to 120.0 ┬▒ 21.0 and 75.4 ┬▒ 12.3 mm Hg, respectively after urination. The average differences in systolic and diastolic BP before and after urination were 4.2 ┬▒ 10.7 mm Hg and 2.8 ┬▒ 7.7 mm Hg, respectively (P < 0.001) (Figure 1). There was no significant correlation between duration of holding urine and difference of systolic (r = -0.053, P > 0.05) or diastolic BP (r = 0.015, P > 0.05) after adjustment for age and BMI. The subjects were compared the change of their stage among normal, prehypertension, and stage 1 and 2 hypertension before and after urination. After voiding urine, the numbers of subjects in normal, prehypertension, and stage 1 and 2 hypertension were 92 (53.5%), 40 (23.3%), 29 (16.9%), and 11 (6.4%) respectively. 24 people (26.1%) out of 92 in normal group after urine-voiding changed their stage (20 in prehypertension, 4 in stage 1 hypertension) during holding urination. 17 people (42.5%) in prehypertensive group after urine-voiding changed into the stage 1 hypertension group during holding urination. Being stage 1 hypertension after urine-voiding, 12 people (41.4%) had experienced their BP elevated during holding urination, so they were classified into the stage 2 hypertension group. Urine voiding brought significant BP lowering results (Table 1 and Figure 2).
Prevalence of hypertension is estimated to be as much as 1 billion individuals worldwide, and approximately 7.1 million deaths per year may be attributable to hypertension.13) According 1998-2007 Korea National Survey, hypertension was very common among Koreans, especially among elderly and people with higher BMI. A higher rate of hypertension was also noted for postmenopausal women.14)
Accurate measurement of BP is important for diagnosis of hypertension. BP should be measured while a subject is sitting on a chair with a back and the subject's arm should be placed on the same level as heart. Caffeine, exercise, and smoking should be avoided for at least 30 minutes prior to measurement.10) Another guideline mentions briefly that bladder distension might cause significant deviations in measured BP.9)
We found that BP significantly decreased after emptying bladder as compared to that while bladder distension. Thus, the distension of bladder raises BP. However, the correlation between the extent of bladder distension and the rises of BP was not significant, suggesting that though holding urine could elevate BP, and BP was not elevated proportionally as the duration of holding urine. This phenomenon suggests that there was so-called ceiling effect on the elevation of BP and that urine volume in bladder did not always correlate with the duration of holding urine, because the rate of bladder filling would vary depending upon the fluid intake, the state of renal function, and individual variation. Distension of bladder has been recognized as a factor to elevate BP. In practice, it is often observed that patients with normal BP found themselves having a high BP when BP was measured while holding urine for a long time as a previous study.1) However, the correlation between the extent of bladder distension and the rises of BP and whether the correlation is proportional have not been determined.
The urine storage process has been known to depend on the coordinated control of a storage chamber, the bladder body, its outlets, the bladder base and urethra, but the mechanisms underlying this process are poorly understood.15) Funke et al.16) reported that there was a significant correlation between the changes of the arterial pressure and arterial plasma renin activity in ten patients with chronically distended bladder due to benign prostatic hyperplasia before and after bladder drainage. They suggested that the renin-angiotensin system might be involved in patients with bladder distension. Hogenson17) said that following surgery and anesthesia, increased sympathetic stimulation caused by a high level of circulating catecholamines can lead to acute postoperative hypertension, and bladder distension may be a causal factor. Another possible cause of the difference of BP between before and after urine-voiding is a 'white coat' effect. When BP was measured for the first time at the health promotion center, subjects might be somewhat nervous. During the second measurement of BP, subjects might be settled. This change of psychological state can influence their BP.18)
In this study, duration of bladder distension was calculated indirectly by asking to the patients. Although only the patients insisting they surely remembered the duration of urine-holding were included and abdominal ultrasound was performed to confirm a full bladder, depending on patient's memory is a limitation in this study. Unfortunately, we also did not perform real-time ultrasound measurement of bladder volume in our subjects. Ideally, BP should have been measured first at the emptying state in bladder, and then BP should have been rechecked repeatedly over time till bladder would be full. The present study, however, could not get the baseline BP because when the subjects had arrived at the health promotion center, they had already been holding urination at least for an hour.
In conclusion, systolic and diastolic BPs were elevated by bladder distension of at least 3 hours of urine-holding, but there is no positive correlation between the extent of bladder distension and the rise of BP in menopausal women. Our finding suggests that distension of the bladder is a factor to increase BP, thus in practice, BP should be measured after emptying the bladder.
ACKNOWLEDGEMENTS
This study was supported by 2010 Research Grant from Pusan National University Yangsan Hospital.
References
1. O'connor VJ. Observations on the blood pressure in cases of prostatic obstruction. Arch Surg 1920;1:359-367.

2. Talaat M. Afferent impulses in the nerves supplying the urinary bladder. J Physiol 1937;89:1-13. PMID: 16994840.



3. Watkins AL. Reflex responses of the nictitating membrane and the blood pressure to distention of the bladder and rectum. Am J Physiol 1937;121:32-39.

4. Guttmann L, Whitteridge D. Effects of bladder distension on autonomic mechanisms after spinal cord injuries. Brain 1947;70:361-404. PMID: 18903252.


5. Szasz JJ, Whyte HM. Effect of distension of the bladder and of contraction of sphincters on blood pressure. Br Med J 1967;2:208-210. PMID: 6023104.



6. Scultety S, Varga B, Szabo D. Effect of bladder distension on blood pressure. Int Urol Nephrol 1971;3:11-19. PMID: 5155006.


7. Rappelli A. Hypertension and obesity after the menopause. J Hypertens Suppl 2002;20:S26-S28. PMID: 12183846.

8. Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005;111:697-716. PMID: 15699287.


9. Weatherall M, Harwood M. The accuracy of clinical assessment of bladder volume. Arch Phys Med Rehabil 2002;83:1300-1302. PMID: 12235612.


10. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003;289:2560-2572. PMID: 12748199.


11. Liang WW. Seasonal changes in preprandial glucose, A1C, and blood pressure in diabetic patients. Diabetes Care 2007;30:2501-2502. PMID: 17586743.


12. Asai Y, Ishikawa S, Kayaba K, Goto T, Nago N, Kario K, et al. Prevalence, awareness, treatment, and control of hypertension in Japanese rural communities. Nippon Koshu Eisei Zasshi 2001;48:827-836. PMID: 11725526.

13. Lawes CM, Vander Hoorn S, Law MR, Elliott P, MacMahon S, Rodgers A. Blood pressure and the global burden of disease 2000. Part II: estimates of attributable burden. J Hypertens 2006;24:423-430. PMID: 16467640.


14. Lee K. Cardiovascular risk prevalence, awareness, treatment, and control from 1998 to 2007 in Koreans. Asia Pac J Clin Nutr 2010;19:261-265. PMID: 20460242.

15. Vaughan CW, Satchell PM. Urine storage mechanisms. Prog Neurobiol 1995;46:215-237. PMID: 7568914.


16. Funke PJ, Prabhakar NR, Hertle L, Runkel N, Dahlheim H. Plasma renin activity and cardiovascular changes in patients with chronic bladder distension. Urol Int 1982;37:363-368. PMID: 6760517.


17. Hogenson KD. Acute postoperative hypertension in the hypertensive patient. J Post Anesth Nurs 1992;7:38-44. PMID: 1735870.

Figure┬Ā2
Changes in classification of blood pressure before and after urination. 1. normal: <120/80 mm Hg, 2: prehypertension, 120-139 or 80-89 mm Hg, 3: hypertension, stage 1, 140-159 or 90-99 mm Hg, 4: hypertension, stage 2, Ōēź160 or Ōēź100 mm Hg.
- TOOLS








