INTRODUCTION
The legs with pain and paresthesia are frequently reported problems of patients who visit a clinical office of family physician. One of the highly possible diseases is an acute lower limb ischemia from inappropriate blood flow. Prompt diagnosis and revascularization can lead to limb salvage, whereas delayed recognition can place patient at high risk of significant morbidity including limb loss and potentially mortality. Proper management of acute lower limb ischemia is determined by the underlying etiology(embolic or thrombotic). Correct diagnosis of variable clinical clues can prevent unproper surgical intervention and repeated events.1)
In primary care, atrial fibrillation (AF) is the most common cardiac rhythm disturbance observed increasingly at the elderly population and has numerous potential complications such as stroke, thromboembolism, and heart failure. In a large cohort study of AF, the stroke rate in patients with paroxysmal AF (PAF) is same with that in patients with permanent AF.2) These results imply that the patients with PAF should be treated likewise to persistent or permanent AF.3)
Beside the studies on the association of the stroke risk with AF including PAF, it is hard to find the studies or case reports on the arterial embolism on the lower limb with PAF. While investigating the cause of embolism on popliteal artery after initial treatment, we successfully documented PAF after several trials of Holter monitoring and repeated electrocardiography (EKG) during palpitation. Here, we report a case of popliteal artery embolism due to PAF in a 69-year-old woman with sudden onset of right calf muscle pain and paresthesia.
CASE REPORT
A 69-year-old woman was admitted to the Department of Family Medicine at our hospital with sudden onset of right calf muscle pain and paresthesia that started 6 days ago. At the moment, she had one episode of dizziness with black out vision of 2-3 seconds. Additionally, she had complained of pain at the low back and bilateral knee.
Her medical history showed significant diabetes with retinopathy of 35 years and hypertension of 15 years. But she had no history of peripheral vascular disease, intermittent claudication, valvular heart disease, AF, hypercoagulable disorder, or smoking. Family history did not yield any remarkable findings.
On physical examination, the patient's blood pressure was 130/90 mm Hg; pulse, 76 beats per minute; temperature, 36.8Ōäā; and respiratory rate, 20 breaths per minute. Her weight was 57.2 kg, and her body mass index was 25.4 kg/m2. She had normal heart sound with no murmurs. Her right feet had weak pulsation on popliteal artery and dorsalis pedis, cold mottled skin and smaller circumference of calf muscle than left one.
A normal complete blood cell was obtained during further examination. The levels of lipid profile and blood chemical panel except blood sugar were also in reference scale. Thyroid function was normal and HbA1c was 7.3%. The most of profiles of coagulation test were in reference range except that D-dimer level showed small elevation and that antithrombin III and protein-S activity in serum was low with 0.55 ┬Ąg/mL, 32.7%, and 54%, respectively. The lupus anticoagulant and anticardiolipin antibody (IgM and IgG) were negative. The chest X-ray revealed mild cardiomegaly without active lung lesions. The sinus bradycardia was documented initially and the heart rate was 56 beats per minutes. The finding on echocardiography was normal that left atrial diameter was 32 mm, left ventricular systolic diameter 26 mm, left ventricular diastolic diameter 47 mm, left ventricular ejection fraction 69%, normal valvular morphology and function.
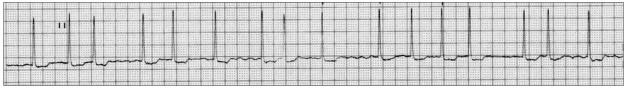
At the department of family medicine, the ankle and brachial systolic pressure index (ABI) doppler test was done and ABI of the right ankle was lower (0.56) than ABI of the left one (1.1). In order to find vascular lesions of the affected limb, we performed the contrast-enhanced computer tomographic angiography, which showed acute embolic occlusion of right popliteal artery (Figure 1). We decided to refer to cardiovascular division of the internal medicine department for removing her thrombus. And then, femoral arteriogram confirmed the total occlusion of popliteal artery on the right side (Figure 2). The thrombi were successfully removed by thombosuction at the same time. After procedure, blood flow of the right popliteal artery had been normally restored (Figure 2). Anticoagulation was started immediately after eliminating emboli and transitioned to oral vitamin K antagonist. ABI follow up showed normal result (right, 1.04; left, 1.02) at 4th days after procedure. The myocardial thallium spect was performed to reveal the cause of acute embolic episode, and the result was within a normal range. When palpitating, she was tested with several times of the Holter monitorings and EKG. The PAF was recorded on the sixth holter monitoring and the EKG was performed on seven o'clock in the morning (Figure 3) and the rhythm was restored to normal sinus rhythm on seven o'clock in the evening (Figure 4), when she visited an emergency room with palpitation. The cause of ischemic foot of the patient proved an embolic episode by PAF. The patient has been treated with oral vitamin K antagonist to prevent embolic episodes from recurring.
DISCUSSION
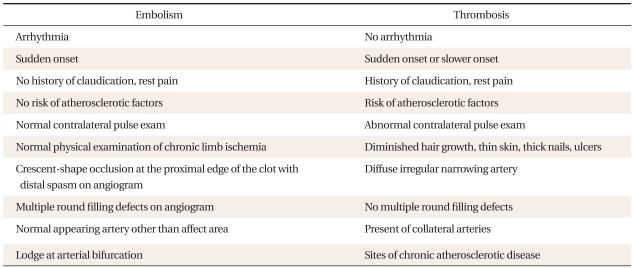
During family medical practice, physicians have the chances to interview the patients with pain, pallor, and paresthesia. For primary care physicians to diagnose acute ischemic foot, they need to check the initial critical cardinal signs, which are referred as "six Ps": pain, pallor, poikilothermia, pulselessness, paresthesia, and paralysis. The affected leg and foot will have no pulse and look pale initially. When the patient's history, symptoms and clinical findings (Table 1) strongly suggest ischemic foot such as an arterial embolism of lower extremities, an immediate diagnostic work-up like ABI and initiation of treatment or the consultation to specialists are necessary. If patient has the risk factors of ischemic foot like patients older than 70 years, smoker or diabetes patients older than 50 years, thrombotic occlusion generally occurs in the setting of atherosclerotic vascular disease.1)
The primary care physician should examine pulses of femoral artery, popliteal artery, dorsal plantar artery, and posterior tibial artery on patient's both legs with supine position. Pulse examination is a very important step that should be done by family physician in order to determine the level of arterial occlusion, initial proper differential diagnosis and the direction of treatment and evaluation. Spinal stenosis and lumbar radiculopathy present symptoms similar to those of the ischemic foot and may confuse physicians. But they are distinguishable by careful history taking and examination. ABI objectively quantifies the severity and extent of the ischemia.
Before consulting a vascular specialist, the primary care physician should determine which methods are proper for each clinical case. Gold standard of diagnosis is arteriography. Alternative imaging modalities that may be employed to evaluate an acute ischemic limb include duplex ultrasound, computed tomographic angiography, and magnetic resonance angiography.4)
Acute limb ischemia occurs from abrupt interruption of blood flow to an extremity usually because of either embolic or thrombotic vascular occlusion. When profound ischemia developed, this manifest as an emergent episode in which restoration of perfusion through early intervention can lead to limb salvage, whereas delay may result in significant morbidity, including limb loss and, potentially, death. These are the reasons why initial proper evaluation and diagnosis by family physicians are critical in saving limbs when patients with the symptoms of acute limb ischemia come to the family physician initially.
Embolic arterial occlusion is the etiology of the acute ischemia in 15% of the patients while arterial thrombosis is such in 85% of patients, most of whom have atherosclerotic disease. With embolic occlusion, a cardiac origin is the source of emboli in 80-90% of cases, usually in the setting of AF or acute myocardial infarction. Embolic occlusion brings dramatic limb ischemia and is the most frequent cause of acute limb ischemia4) while thrombotic occlusion may be less severe and show slower progress than embolic occlusion due to having sufficient collateral blood supply. The treatments for acute limb ischemia are clot removal by catheter-directed thrombolysis with or without percutaneous mechanical thrombectomy, surgical thromboembolectomy followed by correction of underlying arterial lesions, and anticoagulation with continued observation.5)
After successful surgical or endovascular intervention, the physician should make an effort to find a cause of embolus or thrombosis on lower extremities arteries and prevent repetitive events in each clinical case including decision regarding anticoagulation and modifying of atherosclerotic risk factors. Embolic occlusion occurred recurrently in 9% of patients who were appropriately anticoagulated compared with 31% of patients who were not anticoagulated.6)
Among cardiac arrhythmias, AF is detected incidentally by the physician because AF can often be intermittent or lacking in overt symptoms.7) PAF is diagnosed if the episodes stop spontaneously within 7 days. Arterial thromboembolism is the most serious complication of AF, especially ischemic strokes. Stroke rates are similar among paroxysmal, persistent, and permanent AF.2,3) AF is one of causes of the arterial embolism on lower limb. In AF, the annual incidence of acute limb ischemia is 0.4% (lethality 16%).8) Thus PAF is thought to be the cause of popliteal artery embolism on this reported case.
There are several points that the family physician should mull over with each patient's clinical cases. In AF, the treatment of thromboembolic complications generally aims to limit tissue infarction and to restore perfusion to the tissue-at-risk. The AF Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W) showed that oral anticoagulation with warfarin is superior to the combination of clopidogrel plus aspirin for the prevention of vascular events.9) In AF, warfarin reduces the risk of thromboembolic stroke by <50%, also halves the risk of systemic thromboembolism.10)
Yi et al.11) reported that only one out of seven patients had a cardiac structural problem as a cause of an acute thromboemolism of upper limbs on his study in Korea. After performing a number of EKG and Holter monitoring at the symptomatic moments, the underlying etiology of embolic episode in this patient proved PAF. For preventive purpose, the patient has undergone the anticoagulation therapy at the department of family medicine.