INTRODUCTION
1. Epidemiology
Approximately 31% of the global population aged ≥15 years engages in insufficient physical activity, and it is known to contribute to the death of approximately 3.2 million people every year [1]. In South Korea, the physical activity rate is on the decline among adults aged ≥19 years, irrespective of the type of activity, including aerobic exercise, walking, and muscle training. Therefore, in 2017, the rates of aerobic exercise, walking, and muscle training in the Korean adult population were 48.5%, 39.0%, and 21.6%, respectively, with the majority of the Korean population engaging in physical inactivity [2]. In addition to physical inactivity, sedentary behavior is also a serious problem, and a substantial number of people engage in it for prolonged periods. For instance, Americans spend 55% of their waking time (7.7 hours a day) engaged in sedentary behaviors whereas Europeans spend 40% of their leisure time (2.7 hours a day) watching television [3]. Similar patterns have been observed in Koreans, who have been reported to demonstrate long sedentary times. According to Korea Health Statistics of 2018, adults in Korea aged ≥19 years engage in 8.3 hours of sedentary time. Only 8.9% of the adult population engaged in <4 hours of sedentary time whereas 20.6% of the adults were involved in >12 hours of sedentary time [4].
2. Causes of Physical Inactivity and Sedentary Lifestyles
A poor participation in physical activity is speculated to be influenced by multiple factors. Some environmental factors include traffic congestion, air pollution, shortage of parks or pedestrian walkways, and a lack of sports or leisure facilities [1]. Television viewing, video viewing, and cell phone usage are positively correlated with an increasingly sedentary lifestyle [5]. Sedentary behaviors are projected to continue to rise on the basis of this socio-cultural background.
Sedentary lifestyles have a major impact on the overall health of the global population. Many people worldwide engage in sedentary lifestyles, and the prevalence of relevant non-communicable diseases is on the rise. It is well known that insufficient physical activity, that is, physical inactivity, has a detrimental effect on health. Physical inactivity is the fourth leading risk factor for global mortality, accounting for 6% of global mortality [6]. Despite the fact that sedentary behavior poses a comparable risk to health and contributes to the prevalence of various diseases, most physical activity-related education in clinical practice is focused on improving the physical activity levels, with less emphasis on lowering the sedentary behavior. In addition to understanding and informing patients about the health impact of a sedentary lifestyle, healthcare providers of various fields, including clinicians, should reflect upon its significance in policies. This study examined the effects of a sedentary lifestyle on health and the lifestyle-related improvements to be made to promote healthy living.
OVERVIEW OF SEDENTARY LIFESTYLE
1. The Concept of a Sedentary Lifestyle
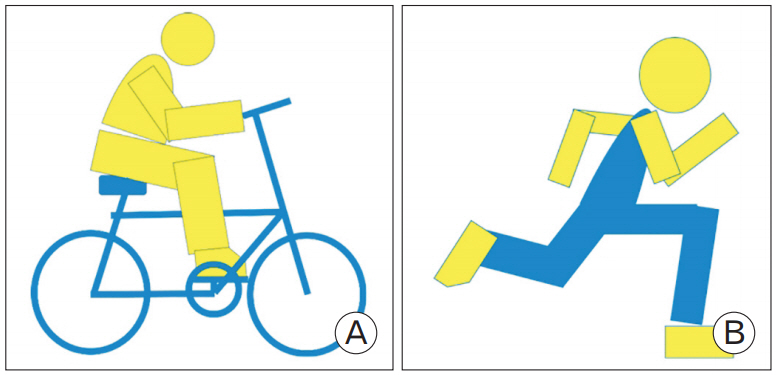
Sedentary behavior is defined as any waking behavior such as sitting or leaning with an energy expenditure of 1.5 metabolic equivalent task (MET) or less [7]. This definition, proposed by the Sedentary Behavior Research Network in 2012, is currently the most widely used definition of sedentary behavior. Some examples of sedentary behavior include television viewing, playing video games, using a computer, sitting at school or work, and sitting while commuting (Figure 1) [8]. According to the 2011 Compendium of Physical Activities, MET is defined as the ratio of work metabolic rate to the standard resting metabolic rate (RMR) of 1 kcal/(kg/h). One MET is the RMR or energy cost for a person at rest. When classified quantitatively based on their intensities, physical activities can be classified into 1.0–1.5 METs (sedentary behavior), 1.6–2.9 METs (light intensity), 3–5.9 (moderate intensity), and ≥6 METs (vigorous intensity) (Figure 2) [9].
A sedentary lifestyle increases all-cause mortality and the risks for cardiovascular diseases (CVD), diabetes mellitus (DM), hypertension (HTN), and cancers (breast, colon, colorectal, endometrial, and epithelial ovarian cancer). This has been consistently documented in the literature [3,10,11]. There is no disagreement on the fact that prolonged total sedentary behavior times are associated with poor disease outcomes. However, the patterns of sedentary time may differ even within the same total amount of time, and not much is known about the particular patterns of prolonged sedentary time that pose more significant health hazards (for example, continuous sedentary behavior without a break or intermittent sedentary behavior) [12]. One study reported that even if the total sedentary time was equal, having short sedentary bouts and engaging in physical activities intermittently can have relative health benefits. The total sedentary time and moderate-to-vigorous physical activity (MVPA) have been reported to be negatively correlated, where the waist circumference (standardized β, -0.16; 95% confidence interval [CI], -0.31 to -0.02; P=0.026), body mass index (β, -0.19; 95% CI, -0.35 to -0.02; P=0.026), triglyceride level (β, -0.18; 95% CI, -0.34 to -0.02; P=0.029), and 2-hour postprandial plasma glucose level (β, -0.18; 95% CI, -0.34 to -0.02; P=0.025) decreased with increasing the number of breaks in the sedentary time [13]. Furthermore, when the sedentary time was interrupted with light- or moderate-intensity physical activity, the systolic and diastolic blood pressures dropped by 2–3 mm Hg whereas interrupting the sedentary time with light-intensity physical activity (LIPA) or simple muscle training in patients with diabetes (88% of the population had HTN) decreased the systolic pressure by 14–16 mm Hg and the diastolic pressure by 8–10 mm Hg [14].
2. Physiological Features
The exact mechanisms of the various adverse effects of sedentary behavior on the human body are currently unknown. However, several hypotheses have been proposed for the overall understanding of the impact of sedentary behavior on the human body, which are described below.
Sedentary lifestyles are associated with metabolic dysfunctions, such as elevated plasma triglycerides and high-density lipoprotein (HDL) cholesterol and reduced insulin sensitivity [15,16]. Lipoprotein lipase (LPL) is a protein that interacts at the cellular level, and a low LPL concentration is known to decrease the plasma HDL cholesterol level, while affecting the prevalence of severe HTN, diabetes-induced dyslipidemia, metabolic disorders caused by aging, metabolic syndrome, and coronary artery diseases. Moreover, LPL activity is diminished by physical inactivity. Additionally, physical inactivity inhibits LPL activity in skeletal muscles and rapidly signals for impaired lipid metabolism. In an experiment based on a rat model, the reduction of LPL activity in rats that engaged in light walking was only about 10% of the LPL activity in rats that were only placed in their cages [17]. The fact that muscle LPL activity is highly sensitive to physical inactivity and low-intensity muscular contractile activity can serve as evidence supporting the theory that sedentary behavior is a risk factor for various metabolic disorders [18].
Physical inactivity reduces bone mineral density [19]. In a study on healthy adult men and women, 12 weeks of bed rest decreased the mineral density of the lumbar spine, femoral neck, and greater trochanter by 1%–4% [19]. The balance between bone resorption and bone deposition mediates the relationship between sedentary behavior and the reduction of bone mineral density. According to some studies, bed rest elevates bone resorption markers and does not influence bone formation markers [20-22].
Some studies have provided limited evidence that sedentary behavior has a negative impact on vascular health. A study on healthy women reported that 56 days of head-down bed rest decreased the endothelium-dependent vasodilation while increasing the endothelial cell damage. Such alterations in vascular function were prevented through aerobic exercise and muscle training [23].
SEDENTARY LIFESTYLES AND HEALTH RISKS
1. Sedentary Lifestyles, Mortality, and Morbidity (Cardiovascular Diseases and Other Causes)
A sedentary lifestyle is strongly associated with CVD, DM, cancer, and premature mortality. The total daily sedentary time and television viewing time were correlated with an increased all-cause mortality risk [24]. In a study analyzing the mortality rates of people with >10 hours and <5 hours of sitting times a day, the sitting time was significantly correlated with all-cause mortality (odds ratio [OR], 1.16; 95% CI, 1.04– 1.29; P<0.05) [25]. In a study that examined the correlation between the television viewing time and all-cause mortality, the people who watched television for ≥6 hours a day had a two-fold higher all-cause mortality risk compared to the people who watched television for <2 hours a day (hazard ratio [HR], 1.98; 95% CI, 1.25–3.15) [26] whereas the people who watched television for ≥4 hours a day had a 1.5 times higher all-cause mortality risk compared to the people who watched TV for <2 hours a day (HR, 1.48; 95% CI, 1.19–1.83) [27].
Sedentary time (sitting time, television or screen viewing time, leisure time while sitting in a day) is independently associated with allcause mortality, CVD incidence or mortality, incidence or mortality of certain cancers (breast, colon, colorectal, endometrial, and epithelial ovarian cancer), and type 2 DM. In particular, the adverse effect of sedentary time was more evident among people who engaged in little physical activity compared to those who engaged in frequent physical activity. The relative risk (RR) for all-cause mortality was 30% higher with high physical activity (HR, 1.16; 95% CI, 0.84–1.59) compared to that with low physical activity (HR, 1.46; 95% CI, 1.22–1.75) [28].
2. Sedentary Lifestyles and Metabolic Diseases
1) Diabetes mellitus
The fact that the prevalence of type 2 DM increases with increasing sedentary time has been consistently documented in various studies (HR, 1.91; 95% CI, 1.64–2.22) [28].
In an assessment of DM risk considering both sedentary time and physical activity, the DM risk increased with the increasing daily sedentary time (HR, 1.13; 95% CI, 1.04–1.22; P<0.001), and the effect was not offset by the level of physical activity (HR, 1.11; 95% CI, 1.01–1.19; P<0.001). The risk for CVD also increased with the increasing daily sedentary time (HR, 1.29; 95% CI, 1.27–1.30; P<0.001), and although the physical activity level slightly offset this effect, sedentary time still significantly increased the risk (HR, 1.11; 95% CI, 1.01–1.19; P<0.001). This shows that the level of physical activity does not influence the impact of prolonged sedentary time on the risk for CVD and DM.
A few biological mechanisms can explain the impact of the total daily sedentary time on CVD and DM risk. Prolonged sitting is known to affect the content and activity of muscle glucose transporter proteins. An animal study observed that prolonged muscle inactivity reduces the LPL activity, which regulates blood lipid concentration and carbohydrate metabolism through cellular pathways that differ from the normal motor response; however, additional verification is required by human studies [29].
2) Hypertension
A sedentary lifestyle affects blood pressure through various mechanisms, and subsequently changes the blood pressure by altering the cardiac output and total peripheral vascular resistance. A prolonged sedentary time reduces the metabolic demands and systemic blood flow, and by stimulating the sympathetic nervous system, it decreases insulin sensitivity and vascular function while increasing the oxidative stress and promoting the low-grade inflammatory cascade [14]. A study reported a direct association between sedentary behavior and a high risk of HTN (HR, 1.48; 95% CI, 1.01–2.18; P for trend=0.03). Among sedentary behaviors, non-interactive sedentary behaviors (watching television, sleeping) have been reported to further escalate the risk for HTN compared to interactive sedentary behaviors (driving, using a computer) [30].
3) Dyslipidemia
Sedentary behaviors induce metabolic dysfunction characterized by elevated blood triglyceride levels, reduced HDL-cholesterol levels, and diminished insulin sensitivity [17]. A study reported that sedentary behaviors increased the rate of newly diagnosed dyslipidemias in women (OR, 1.17; 95% CI, 1.00–1.36) and increased the risk for dyslipidemia in both men and women (men: OR, 1.21; 95% CI, 1.02–1.44) (women: OR, 1.24; 95% CI, 1.04–1.48) [31]. In contrast, MVPA was negatively associated with blood triglyceride levels (β, -0.18; 95% CI, -0.36 to -0.01; P=0.038) [32].
4) Obesity
Sedentary time is known to have significant correlations with waist circumference and clustered metabolic risk scores independent of MVPA. The waist circumference increased by 3.1 cm with a 10% increase in the sedentary time [32]. Obese patients tend to move less; therefore, increasing the activity levels can be utilized as a strategy in obesity treatment [33]. While this is a widely known fact, the underlying mechanism remains unknown. A study in 2020 reported that the reason for weight gain is a prolonged sedentary time [34]. According to a Swedish study that compared an experimental group which wore a heavy 11-kg vest for 8 hours a day and the control group which wore a light 1-kg vest for 8 hours a day, the experimental group had a weight loss of 1.6 kg whereas the control group lost 0.3 kg three weeks later. An animal study shed light on an energy balance system known as the “gravitostat” that maintains a consistent body weight [35]. This regulation occurs partially due to an influence on appetite where the system requires a personal weighing machine for the proper functioning of this regulation. This Swedish study found that humans also feature a similar built-in scale. An individual’s scale measures lower values with prolonged sitting, which explains why sitting is associated with obesity and poor health. A heavy vest can increase the score on this, thereby inducing weight loss [34].
3. Sedentary Lifestyles and Cancer Risk
Sedentary behavior is also closely related to the prevalence of cancer. According to a study that investigated the correlation between sedentary behavior and cancer prevalence, the cancer risk was 13% higher in the group with the longest sedentary time compared to that with the shortest sedentary time [28], and another study reported that sedentary time increased the overall cancer risk by 20% [36].
Prolonged sitting increases colorectal, endometrial, ovarian, and prostate cancer risks, and it has been reported to increase cancer mortality particularly in women [37]. There was a significant correlation between cancer mortality and the incidences of breast, colorectal, endometrial, and epithelial ovarian cancers [28]. An increased total sitting time was positively correlated with colon cancer (RR, 1.24; 95% CI, 1.03–1.50) and endometrial cancer (RR, 1.32; 95% CI, 1.08–1.61) [36]. Additionally, television viewing time was also positively correlated with colon cancer (RR, 1.54; 95% CI, 1.19–1.98) and endometrial cancer (RR, 1.66; 95% CI, 1.21–2.28) [36]. Occupational sitting time was positively correlated with only colon cancer (RR, 1.24; 95% CI, 1.09–1.41) [36].
Sedentary behavior leads to metabolic dysfunctions such as hyperglycemia, hyperinsulinemia, insulin resistance, perturbation of insulin-like growth factor axis, and changes in the circulation levels of sex hormones. Altered circulation levels of sex hormones can be linked to hormone-related cancers such as breast and endometrial cancers [38]. Additionally, sedentary behavior induces low-grade chronic systemic inflammation, and sedentary time is associated with inflammation-related markers such as C-reactive protein (β, 0.18±0.06; P=0.002), interleukin 6 (β, 0.24±0.06; P<0.001), leptin (β, 0.15±0.04; P<0.001), and the leptin: adiponectin ratio (β, 0.21±0.05; P<0.001) [39]. Chronic inflammation can trigger cancer growth [40]. Adiposity can also mediate the relationship between sedentary behavior and cancer, and obesity is a risk factor for several cancers [8].
4. Sedentary Lifestyles and Osteoporosis
Sedentary behavior is known to show a negative association with the bone mineral density of the total femur and all hip sub-regions irrespective of MVPA, and the bone mineral density (g/cm2) of the total femur had a marked negative correlation with the sedentary time (β, -0.16; 95% CI, -0.24 to -0.08) in adult women [41]. Bone mineral density was correlated with the duration and not the frequency of sedentary behavior. In men, sedentary behavior was not markedly correlated with the bone mineral density of the hip and spine [41].
5. Sedentary Lifestyles and Musculoskeletal Diseases
A prolonged sedentary time was correlated with chronic knee pain. In an analysis of the correlation between chronic knee pain and the total daily sedentary time (<5, 5–7, 8–10, >10 hours), the results claimed that the incidence of chronic knee pain was higher in individuals with longer sedentary times (P for trend=0.02) [42]. In particular, a sedentary time >10 hours a day was markedly correlated with chronic knee pain (adjusted OR, 1.28; 95% CI, 1.02–1.61; P=0.03) [42]. People who engaged in greater physical activity had less chronic knee pain (adjusted OR, 0.78; 95% CI, 0.67–0.91; P=0.00), but women with >10 hours of sedentary time while engaging in greater physical activity were highly likely to experience chronic knee pain (adjusted OR, 1.19; 95% CI, 1.02–1.39; P=0.03). The study recommends individuals to shorten their sedentary times to <10 hours a day [42].
6. Sedentary Lifestyles and Other Diseases
1) Depression
Mentally passive sedentary behaviors such as television viewing (RR, 1.18; 95% CI, 1.07–1.30), sitting, listening to music, and talking while sitting were positively correlated with depression risks (RR, 1.17; 95% CI, 1.08–1.27). In contrast, mentally active sedentary behaviors such as reading books or newspapers, driving, attending a meeting, or knitting or sewing were not markedly correlated with depression risk (RR, 0.98; 95% CI, 0.83–1.15) [43]. Using a computer, which is a mentally active sedentary behavior, was not correlated with depression risk in one study (RR, 0.99; 95% CI, 0.79–1.23) [43] but was positively correlated with depression risk in another study (RR, 1.22; 95% CI, 1.10–1.34) [44], and thus its correlation with depression remains controversial. The mechanism underlying the correlation between sedentary behavior and depression may involve the following: sedentary behaviors may increase the risk for depression by blocking direct communication and lowering social interactions, or by reducing the available time to engage in physical activities that help to prevent and treat depression [43].
2) Cognitive function
The relationship between sedentary behavior and cognitive function is uncertain. A systematic review found marked alterations of cognition (improved in two studies45,46) and impaired in two studies47,48)) in some studies but no changes in cognitive function in some studies.49) However, the only long-term study included in that systematic review suggested that a less-sedentary lifestyle and less sedentary work have benefits related to cognitive function.46) It is believed that replacing the sedentary time with physical activity can help improve the cognitive function. In a randomized clinical trial that analyzed the cognitive changes after 30 minutes of sedentary behavior with other activities for 6 months in older adults with little physical activity, replacing the sedentary time with MVPA and sleep significantly improved cognitive functions, and replacing it with LIPA did not lead to statistically significant changes [46].
SEDENTARY LIFESTYLES AND PHYSICAL ACTIVITY
1. Discrepant Health Effects of Sedentary Lifestyle and Physical Activity
Past studies have observed that a prolonged sedentary lifestyle leads to poor health outcomes irrespective of physical activity. A sedentary lifestyle was independently correlated with mortality and was not compensated for by physical activity [10]. The time spent in front of a screen was positively correlated with the presence of metabolic syndrome, independent of the level of physical activity (OR, 3.30; 95% CI, 2.04–5.34) [50].
2. The Attenuative Effect of Physical Activity on Sedentary Lifestyles
A few recent studies have reported that increasing physical activity can offset the adverse impacts of sedentary behavior. In particular, the offset effect was more evident in people with little physical activity.
A meta-analysis reported that mortality was not elevated in the people engaging in high levels of moderate-intensity physical activity (60– 75 minutes of moderate-intensity physical activity a day) even when they had >8 hours of sedentary time a day. There was no difference in mortality between the most active people (>35.5 MET-h/wk) with <4 hours of sedentary time a day and equally active people (>35.5 MET-h/wk) with >8 hours of sedentary time a day (HR, 1.04; 95% CI, 0.99–1.10). However, television viewing for >3 hours a day increased the mortality regardless of physical activity, and the people who watched television for ≥5 hours a day showed markedly high mortalities (HR, 1.16; 95% CI, 1.05–1.28) [51].
In one study, sitting time showed a dose-response with all-cause mortality and CVD mortality risk in the least active group (<150 MVPA min/wk) [51]. In contrast, the group with at least 8 hours of sedentary time a day showed a higher mortality than the group with less than 4 hours of sedentary time a day (HR, 1.52; 95% CI, 1.13–2.03). However, the group who met the essential MVPA criterion (150–299 MVPA min/ wk) or engaged in more physical activity did not show a consistent trend in the relationship between increased sitting time and CVD and all-cause mortalities.
Similarly, a study showed that a sedentary time of over 9 hours per day in the low physical activity group (<600 METs-min/wk) had a significant association with an increased CVD risk (OR, 1.29; 95% CI, 1.04–1.62). In the group with more physical activity, sedentary time was not significantly associated with CVD risk [52].
In other words, while increased sedentary time increases the mortality among people who engage in little physical activity, adequate physical activity seems to offset the impact of increased sedentary time on mortality [53].
A study analyzed the correlation between all-cause mortality and net uncompensated sedentary behavior metabolic equivalent hours (USMh=MET/h [sedentary time]–MET/h [MVPA time]), which was computed by subtracting METs for MVPA from METs for sedentary behavior throughout a day. USMh was independently associated with all-cause mortality when it was greater than 7 MET/h, and for television viewing, when it was greater than 3 MET/h. The mean increase in mortality per USMh was 1% (RR, 1.01; 95% CI, 1.00–1.02; P=0.01), and the mean increase in mortality per USMh for TV watching was 7% (RR, 1.07; 95% CI, 1.04–1.10; P<0.001). In other words, physical activity as well as sedentary time should be assessed, and therefore, USMh was revealed to be a more practical index for assessing sedentary behavior [54].
In the people with the least daily activity (≤17 min/d MVPA), replacing 30 minutes of the sitting time each day with light physical activity reduced the mortality risk by 14% (HR, 0.86; 95% CI, 0.81–0.89), and replacing it with MVPA reduced the mortality risk by 45% (HR, 0.55; 95% CI, 0.47–0.62). However, in the people with the highest daily activity (MVPA >38 min/d), replacing the sitting time with LIPA or MVPA was not linked with a reduced mortality risk [55].
Replacing the sedentary behavior with physical activity also has an impact on cancer-related mortality. A recently published study showed that sedentary behavior was independently associated with cancer mortality risk, where a higher sedentary time led to a greater cancer mortality risk. In this study, the individuals in the top 1/3 of the sedentary group showed a substantially higher cancer mortality risk than those in the bottom 1/3 (adjusted HR, 1.52; 95% CI, 1.01–2.27) [56]. However, replacing 30 minutes of sedentary time with LIPA reduced the cancer mortality by 8% (HR, 0.92; 95% CI, 0.86–0.97) and replacing it with MVPA reduced it by 31% (HR, 0.69; 95% CI, 0.48–0.97) [56].
CLINICAL PEARLS FOR SEDENTARY INDIVIDUALS
While the various countries have their own guidelines for physical activity and sedentary behavior, overall, the recommendations are similar.
1. Recommendations in the United States
Although the 2018 Advisory Committee revealed that sedentary behavior is strongly correlated with all-cause and CVD mortalities in adults, the evidence was insufficient to offer advice on the recommended daily sedentary time and duration of physical activity. It could not determine the recommended daily sedentary time and frequency of physical activity for adults or adolescents because the risks associated with sedentary behavior are related to the amount of MVPA.
It is advisable for inactive people not engaging in moderate physical activity (MPA) to lower their sedentary behavior and replace their sedentary behavior with LIPA. However, LIPA alone is insufficient to obtain health benefits; they will be able to reduce their health risk by gradually increasing their physical activities to MPA or beyond. Inactive people who engage in insufficient physical activity that does not meet the criterion of 150–300 minutes of MPA per week would be able to obtain health benefits by increasing their MPA slightly and reap even greater health benefits by reducing their sedentary behaviors. Active people who engage in sufficient physical activity (150–300 minutes of MPA per week) would gain more benefits by lowering their sedentary behaviors. Highly active people who engage in more than 300 minutes of MPA per week are recommended to maintain or improve their levels of physical activity by participating in a variety of activities [57].
2. Recommendations in Australia
The Australian Government Department of Health presented age-specific recommendations for physical activity and sedentary behavior. According to the Australian physical activity-sedentary behavior guidelines, individuals are recommended to minimize their sitting times, including sitting during work, commuting, and breaks, and to avoid sitting for prolonged periods as much as possible [58]. Infants and children aged less than 5 years are advised to not be bound in a stroller, car seat, or high chair for more than 1 hour at a time. While they engage in sedentary behaviors, they are recommended to spend time reading books, singing, solving puzzles, and talking with their caregivers as compared to watching television or a DVD (digital video disc), playing on the computer, or playing other video games [59]. For children between the ages of 5 and 17, the sedentary recreational screen time should be limited to 2 hours a day, and they are advised to engage in positive social interactions and experiences. Older adults aged 65 years and more are advised to remain active as much as possible every day [60]. The recommended amount of physical activity for adults is 150–300 minutes of MPA or 75–150 minutes of vigorous physical activity or an equivalent MVPA per week.
3. Recommendations in Korea
The guidelines for physical activity for the Korean population published by the Department of Health Promotion at the Ministry of Health and Welfare in October 2013 recommend that people limit their sedentary leisure time (e.g., computer, smartphone, and television) to 2 hours a day and engage in a low level of physical activity. Children and adolescents are recommended to develop an active lifestyle overall, including sports, physical education, walking, and cycling at home and school. If older adults and people with chronic diseases are unable to engage in the recommended physical activities, these groups of people are advised to engage in physical activities to the extents permitted by their situations [61].
CONCLUSION
Since the beginning of the coronavirus pandemic, social distancing has become important, and engaging in physical activity in the postcorona era is difficult. Therefore, a study of the problems of sedentary lifestyle is considered more valuable at this point.
A sedentary lifestyle has an array of adverse health effects, including elevated all-cause mortality, CVD mortality, cancer risk, risks for metabolic diseases such as DM, HTN, dyslipidemia, and musculoskeletal diseases such as knee pain and osteoporosis.
It is indisputable that the negative health impacts intensify with increases in the total daily sedentary times. For this reason, it is important to reduce the sedentary time as much as possible.
The findings of studies determining the worst type of sedentary behavior varied across studies. Studies observed better health outcomes with a short sedentary bout with intermittent physical activity, with light physical activity or simple muscle training, intermittent interruptions of sedentary behavior during work, and rest with physical activity.
Health outcomes also vary depending on the type of sedentary behavior and watching television led to the worst outcomes. This may be attributable to the fact that television watching is a passive sedentary behavior and that people often consume snacks while watching television. Therefore, among the various types of sedentary behaviors, individuals should refrain from watching television as much as possible, and snacking should be minimized while watching television.
Even if the total daily sedentary time cannot be reduced for unavoidable reasons, it is advisable to engage in sufficient exercise equivalent to or more than 150–300 minutes of MPA per week, as studies found that physical activity could offset the adverse effects of sedentary behavior. If sufficient exercise cannot be performed, individuals should at least perform light physical activity, as opposed to not engaging in physical activity at all as health benefits can be obtained even with light physical activity, albeit insufficient; they should further try to increase their physical activity levels as their situations permit.