 |
 |
- Search
| Korean J Fam Med > Volume 45(3); 2024 > Article |
|
Abstract
Background
Methods
Results
Notes
FUNDING
This study received support from a Korea Evaluation Institute of Industrial Technology (KEIT) grant funded by the Korean government’s Ministry of Trade, Industry, and Energy (MOTIE) (grant no., 20018384) awarded to the author (J.W.L.). It’s important to emphasize that the funding source not been involved in shaping the study design, data collection, analysis, decisions regarding publication, or preparation of the manuscript.
ACKNOWLEDGMENTS
Figure. 1.

Figure. 2.
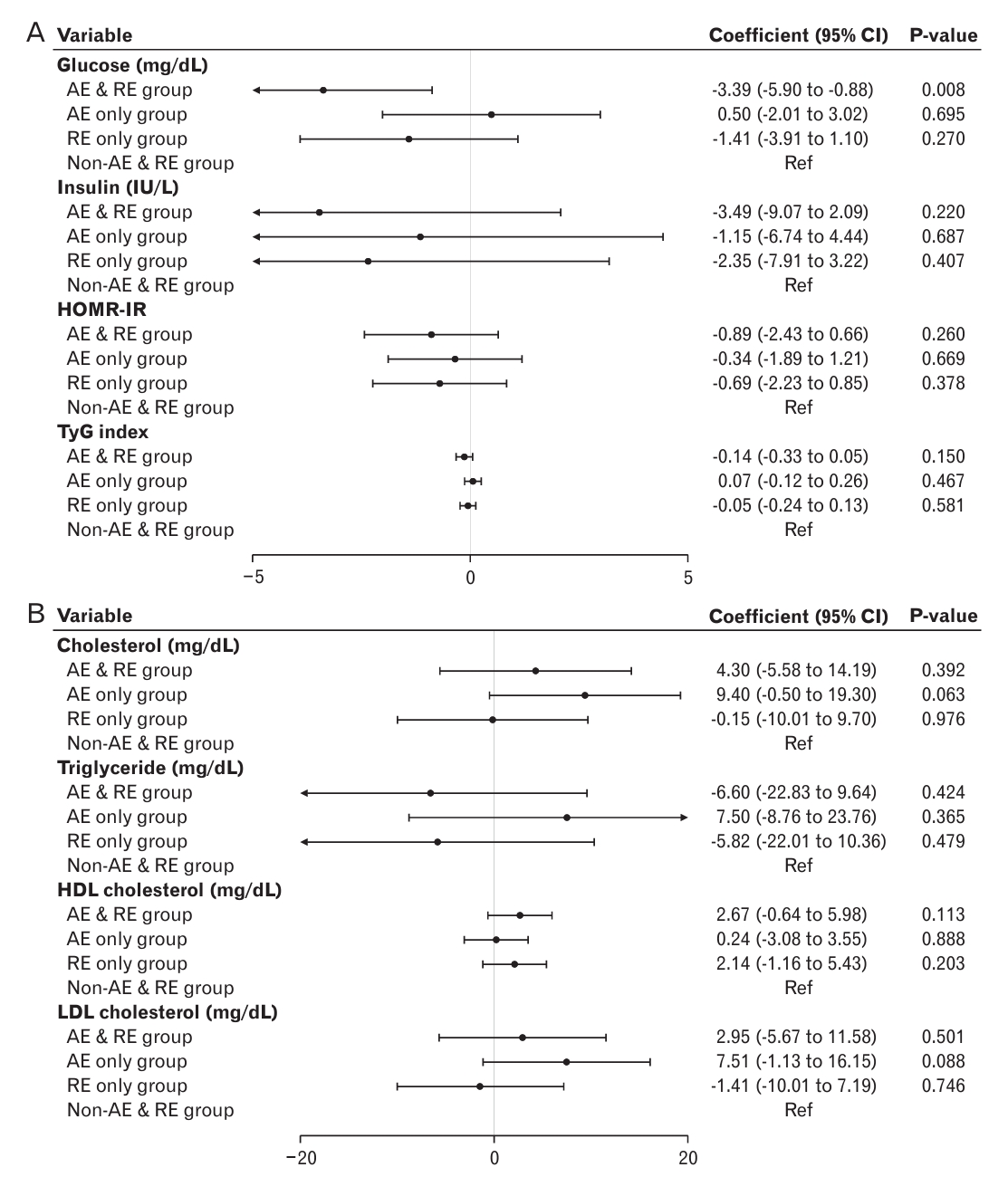
Figure. 3.
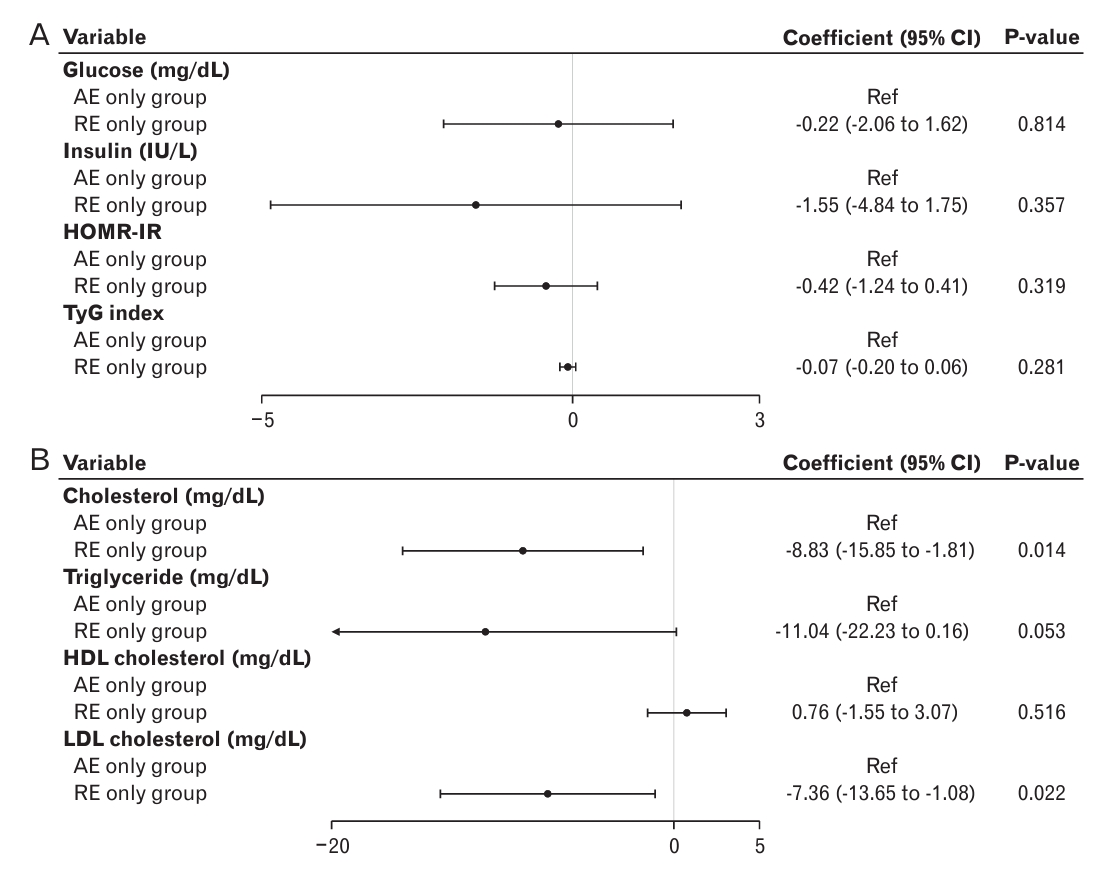
Table 1.
Values are presented as unweighted number, mean±standard error, or % unless otherwise stated.
CE, complex exercise; AE, aerobic exercise; RE, resistance exercise; HDL, high-density lipoprotein; LDL, low-density lipoprotein; HOMA-IR, homeostasis model assessment-estimated insulin resistance; TyG, triglyceride and glucose; AST, aspartate aminotransferase; ALT, alanine aminotransferase; WBC, white blood cell.
Table 2.
| Variable |
CE group |
AE only group |
RE only group |
Non-AE & RE group |
P-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient (95% CI) | P-value | Coefficient (95% CI) | P-value | Coefficient (95% CI) | P-value | Coefficient (95% CI) | P-value | ||
| Body mass index (kg/m2) | -0.323 (-1.161 to 0.516) | 0.449 | 0.471 (-0.590 to 1.531) | 0.383 | -0.275 (-1.132 to 0.581) | 0.528 | Ref | Ref | 0.624 |
| Waist circumference (cm) | -1.139 (-3.437 to 1.159) | 0.33 | 0.172 (-2.379 to 2.722) | 0.895 | -1.197 (-3.525 to 1.131) | 0.313 | Ref | Ref | 0.666 |
| Mean BP (mm Hg) | -1.172 (-3.235 to 0.891) | 0.265 | 0.122 (-1.756 to 2.000) | 0.898 | -2.069 (-3.528 to -0.610) | 0.006 | Ref | Ref | 0.026 |
| Cholesterol (mg/dL) | 1.573 (-5.212 to 8.358) | 0.649 | 7.579 (1.248 to 13.911) | 0.019 | -0.323 (-5.153 to 4.507) | 0.895 | Ref | Ref | 0.121 |
| Triglyceride (mg/dL) | -9.982 (-23.495 to 3.531) | 0.147 | -1.491 (-11.731 to 8.749) | 0.775 | -13.329 (-21.635 to -5.023) | 0.002 | Ref | Ref | 0.009 |
| HDL cholesterol (mg/dL) | 2.937 (0.175 to 5.699) | 0.037 | 2.874 (1.085 to 4.662) | 0.002 | 2.688 (1.045 to 4.331) | 0.001 | Ref | Ref | <0.001 |
| LDL cholesterol (mg/dL) | 0.772 (-5.262 to 6.806) | 0.801 | 4.407 (-1.300 to 10.114) | 0.13 | -1.068 (-5.297 to 3.162) | 0.62 | Ref | Ref | 0.413 |
| Glucose (mg/dL) | -3.167 (-5.136 to -1.197) | 0.002 | 0.428 (-1.484 to 2.341) | 0.66 | -0.719 (-2.082 to 0.644) | 0.3 | Ref | Ref | 0.015 |
| Insulin (IU/L) | -2.378 (-7.528 to 2.773) | 0.365 | 0.572 (-2.689 to 3.832) | 0.731 | -2.368 (-4.580 to -0.155) | 0.036 | Ref | Ref | 0.166 |
| HOMR-IR | -0.547 (-1.954 to 0.859) | 0.445 | 0.186 (-0.621 to 0.992) | 0.651 | -0.589 (-1.126 to -0.053) | 0.031 | Ref | Ref | 0.145 |
| Hemoglobin A1c (%) | 0.046 (-0.021 to 0.113) | 0.177 | 0.017 (-0.043 to 0.078) | 0.573 | -0.014 (-0.067 to 0.040) | 0.618 | Ref | Ref | 0.416 |
| TyG index | -0.169 (-0.315 to -0.022) | 0.024 | -0.027 (-0.148 to 0.094) | 0.662 | -0.120 (-0.218 to -0.022) | 0.016 | Ref | Ref | 0.012 |
| AST (IU/L) | 3.672 (-0.783 to 8.128) | 0.106 | 0.654 (-1.338 to 2.646) | 0.519 | 0.579 (-1.360 to 2.518) | 0.557 | Ref | Ref | 0.366 |
| ALT (IU/L) | -2.419 (-5.880 to 1.042) | 0.17 | -1.181 (-5.074 to 2.713) | 0.551 | -2.189 (-5.490 to 1.112) | 0.193 | Ref | Ref | 0.423 |
| WBC (thousand/μL) | -0.427 (-0.820 to -0.033) | 0.034 | 0.019 (-0.384 to 0.421) | 0.927 | -0.287 (-0.599 to 0.025) | 0.072 | Ref | Ref | 0.047 |
| Metabolic syndrome (yes) | 0.547* (0.139 to 2.153) | 0.387 | 0.685* (0.269 to 1.745) | 0.427 | 0.228* (0.069 to 0.756) | 0.016 | Ref | Ref | 0.088 |
CE, complex exercise; AE, aerobic exercise; RE, resistance exercise; CI, confidence interval; Ref, reference; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; HOMA-IR, homeostasis model assessmentestimated insulin resistance; TyG, triglyceride and glucose; AST, aspartate aminotransferase; ALT, alanine aminotransferase; WBC, white blood cell.
Table 3.
Values are presented as unweighted number, mean±standard error, or % unless otherwise stated.
AE, aerobic exercise; RE, resistance exercise; HDL, high-density lipoprotein; LDL, low-density lipoprotein; HOMA-IR, homeostasis model assessment-estimated insulin resistance; TyG, triglyceride and glucose; AST, aspartate aminotransferase; ALT, alanine aminotransferase; WBC, white blood cell.
Table 4.
| Variable | AE only group |
RE only group |
|
|---|---|---|---|
| Coefficient (95% CI) | P-value | ||
| Body mass index (kg/m2) | Ref | -0.670 (-1.806 to 0.466) | 0.247 |
| Waist circumference (cm) | Ref | -1.378 (-4.316 to 1.560) | 0.357 |
| Mean blood pressure (mm Hg) | Ref | -2.041 (-3.957 to -0.125) | 0.037 |
| Cholesterol (mg/dL) | Ref | -8.831 (-15.855 to -1.807) | 0.014 |
| Triglyceride (mg/dL) | Ref | -11.035 (-22.231 to 0.160) | 0.053 |
| High-density lipoprotein cholesterol (mg/dL) | Ref | 0.762 (-1.547 to 3.071) | 0.516 |
| Low-density lipoprotein cholesterol (mg/dL) | Ref | -7.363 (-13.646 to -1.081) | 0.022 |
| Glucose (mg/dL) | Ref | -0.220 (-2.061 to 1.622) | 0.814 |
| Insulin (IU/L) | Ref | -1.546 (-4.844 to 1.752) | 0.357 |
| Homeostasis model assessment-estimated insulin resistance | Ref | -0.418 (-1.244 to 0.407) | 0.319 |
| Hemoglobin A1c (%) | Ref | -0.006 (-0.072 to 0.060) | 0.861 |
| Triglyceride and glucose index | Ref | -0.071 (-0.200 to 0.058) | 0.281 |
| Aspartate aminotransferase (IU/L) | Ref | 0.730 (-1.954 to 3.414) | 0.593 |
| Alanine aminotransferase (IU/L) | Ref | 0.427 (-4.378 to 5.232) | 0.861 |
| White blood cell (thousand/μL) | Ref | -0.159 (-0.567 to 0.250) | 0.446 |
| Metabolic syndrome (yes) | Ref | 0.315* (0.058 to 1.372) | 0.14 |
REFERENCES
Appendices
Appendix 1.
Comparison of clinical characteristics among the AE-only, RE-only, and non-AE and RE, and CE groups, after matching
| Variable |
CE group |
AE only group |
RE only group |
Non-AE & RE group |
P-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient (95% CI) | P-value | Coefficient (95% CI) | P-value | Coefficient (95% CI) | P-value | Coefficient (95% CI) | P-value | ||
| Body mass index (kg/m2) | -0.337 (-1.700 to 1.027) | 0.627 | 0.415 (-0.951 to 1.781) | 0.55 | -0.102 (-1.462 to 1.257) | 0.882 | Ref | Ref | 0.747 |
| Waist circumference (cm) | -1.661 (-5.328 to 2.005) | 0.373 | 0.463 (-3.210 to 4.136) | 0.804 | -1.005 (-4.660 to 2.651) | 0.589 | Ref | Ref | 0.662 |
| Mean BP (mm Hg) | -0.622 (-3.058 to 1.815) | 0.616 | 0.644 (-1.797 to 3.085) | 0.604 | -0.903 (-3.332 to 1.527) | 0.465 | Ref | Ref | 0.606 |
| Cholesterol (mg/dL) | 4.301 (-5.584 to 14.186) | 0.392 | 9.400 (-0.502 to 19.303) | 0.063 | -0.151 (-10.006 to 9.704) | 0.976 | Ref | Ref | 0.19 |
| Triglyceride (mg/dL) | -6.595 (-22.828 to 9.638) | 0.424 | 7.502 (-8.760 to 23.764) | 0.365 | -5.823 (-22.007 to 10.361) | 0.479 | Ref | Ref | 0.295 |
| HDL cholesterol (mg/dL) | 2.671 (-0.638 to 5.979) | 0.113 | 0.237 (-3.077 to 3.551) | 0.888 | 2.136 (-1.162 to 5.434) | 0.203 | Ref | Ref | 0.285 |
| LDL cholesterol (mg/dL) | 2.951 (-5.674 to 11.577) | 0.501 | 7.507 (-1.135 to 16.148) | 0.088 | -1.414 (-10.013 to 7.186) | 0.746 | Ref | Ref | 0.189 |
| Glucose (mg/dL) | -3.389 (-5.900 to -0.878) | 0.008 | 0.501 (-2.015 to 3.016) | 0.695 | -1.405 (-3.909 to 1.098) | 0.27 | Ref | Ref | 0.012 |
| Insulin (IU/L) | -3.486 (-9.065 to 2.093) | 0.22 | -1.146 (-6.735 to 4.443) | 0.687 | -2.345 (-7.908 to 3.217) | 0.407 | Ref | Ref | 0.639 |
| HOMR-IR | -0.886 (-2.432 to 0.660) | 0.26 | -0.337 (-1.885 to 1.212) | 0.669 | -0.692 (-2.233 to 0.849) | 0.378 | Ref | Ref | 0.684 |
| Hemoglobin A1c (%) | 0.015 (-0.069 to 0.098) | 0.731 | -0.020 (-0.103 to 0.063) | 0.637 | -0.055 (-0.138 to 0.028) | 0.192 | Ref | Ref | 0.382 |
| TyG index | -0.138 (-0.326 to 0.050) | 0.15 | 0.070 (-0.119 to 0.258) | 0.467 | -0.053 (-0.240 to 0.135) | 0.581 | Ref | Ref | 0.174 |
| AST (IU/L) | 3.207 (-2.656 to 9.070) | 0.282 | 0.690 (-5.183 to 6.564) | 0.817 | 1.866 (-3.979 to 7.712) | 0.53 | Ref | Ref | 0.72 |
| ALT (IU/L) | -1.101 (-7.046 to 4.844) | 0.716 | -0.770 (-6.725 to 5.186) | 0.799 | 0.911 (-5.016 to 6.838) | 0.762 | Ref | Ref | 0.913 |
| WBC (thousand/μL) | -0.371 (-0.917 to 0.175) | 0.182 | 0.050 (-0.497 to 0.597) | 0.858 | -0.013 (-0.558 to 0.531) | 0.962 | Ref | Ref | 0.407 |
| Metabolic syndrome (yes) | 1.094* (0.124 to 9.611) | 0.931 | 1.505* (0.231 to 12.148) | 0.668 | 0.536* (0.024 to 5.958) | 0.62 | Ref | Ref | 0.834 |
AE, aerobic exercise; RE, resistance exercise; CE, complex exercise; CI, confidence interval; Ref, reference; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; HOMA-IR, homeostasis model assessmentestimated insulin resistance; TyG, triglyceride and glucose; AST, aspartate aminotransferase; ALT, alanine aminotransferase; WBC, white blood cell.
Appendix 2.
Comparison between AE and RE groups, before matching
| Variable | AE only group |
RE only group |
|
|---|---|---|---|
| Coefficient (95% CI) | P-value | ||
| Body mass index (kg/m2) | Ref | -1.027 (-2.355 to 0.302) | 0.129 |
| Waist circumference (cm) | Ref | -2.263 (-5.723 to 1.196) | 0.198 |
| Mean blood pressure (mm Hg) | Ref | -1.777 (-3.951 to 0.396) | 0.108 |
| Cholesterol (mg/dL) | Ref | -10.369 (-18.628 to -2.110) | 0.014 |
| Triglyceride (mg/dL) | Ref | -16.895 (-30.309 to -3.482) | 0.014 |
| High-density lipoprotein cholesterol (mg/dL) | Ref | 1.152 (-1.465 to 3.769) | 0.386 |
| Low-density lipoprotein cholesterol (mg/dL) | Ref | -8.222 (-15.711 to -0.733) | 0.032 |
| Glucose (mg/dL) | Ref | -1.343 (-3.482 to 0.795) | 0.217 |
| Insulin (IU/L) | Ref | -2.889 (-6.475 to 0.697) | 0.114 |
| Homeostasis model assessment-estimated insulin resistance | Ref | -0.760 (-1.650 to 0.129) | 0.093 |
| Hemoglobin A1c (%) | Ref | 0.030 (-0.046 to 0.107) | 0.432 |
| Triglyceride and glucose index | Ref | -0.158 (-0.313 to -0.002) | 0.046 |
| Aspartate aminotransferase (IU/L) | Ref | -0.277 (-3.295 to 2.742) | 0.857 |
| Alanine aminotransferase (IU/L) | Ref | -0.376 (-6.626 to 5.874) | 0.906 |
| White blood cell (thousand/μL) | Ref | -0.305 (-0.773 to 0.162) | 0.199 |
| Metabolic syndrome (yes) | Ref | 0.197* (0.025 to 1.058) | 0.075 |
- TOOLS







