 |
 |
- Search
| Korean J Fam Med > Epub ahead of print |
|
Abstract
Background
Methods
Results
SUPPLEMENTARY MATERIALS
Supplement 1.
Supplement 2.
Figure. 1.
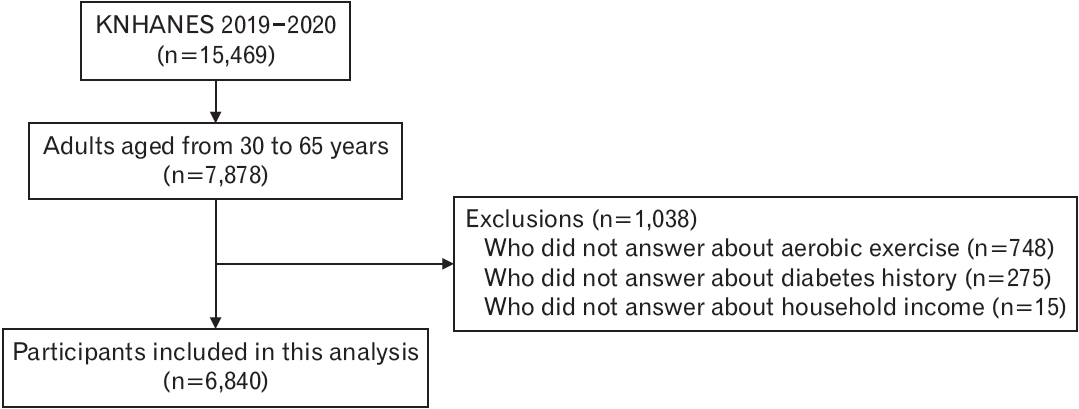
Figure. 2.
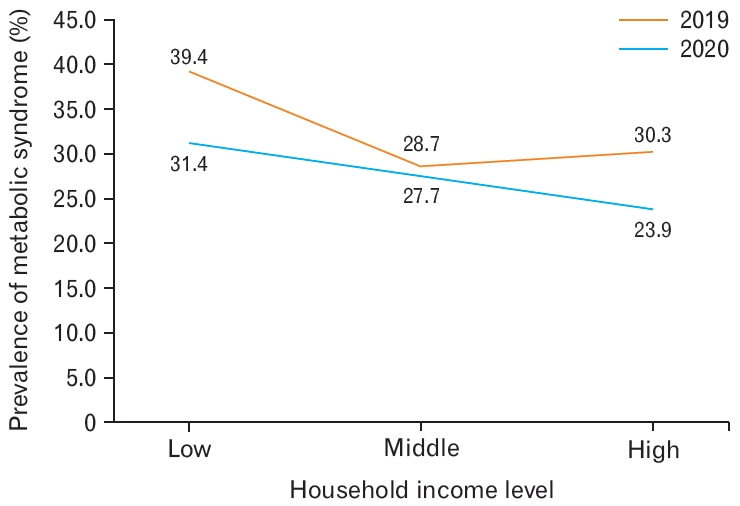
Table 1.
Values are presented as mean±standard error for continuous variables or number (%) for categorical variables. Log substitution was performed with non-normal distribution.
P-values are from a t-test for continuous variables and chi-square test for categorical variables, respectively.
COVID-19, coronavirus disease 2019; WC, waist circumference; FBS, fasting blood sugar; TG, triglyceride; HDL, high-density lipoprotein.
Table 2.
Values are presented as mean±standard error for continuous variables or number (%) for categorical variables. Log substitution was performed with non-normal distribution. P-values are from a t-test for continuous variables and chisquare test for categorical variables, respectively.
COVID-19, coronavirus disease 2019; WC, waist circumference; FBS, fasting blood sugar; TG, triglyceride; HDL, high-density lipoprotein.
Table 3.
Adjusted for sex, age (year, continuous), education levels (less than middle school education, high school education, more than college education), smoking (non-smoker, current smoker), current alcohol (more than twice a week), and aerobic exercise. Calculated using logistic regression analysis.
OR, odds ratio; CI, confidence interval.
REFERENCES
- TOOLS







