The Impact of Pharmacist Medication Reviews on Geriatric Patients: A Scoping Review
Article information
Abstract
Medication review is an intervention with the potential to reduce drug-related problems (DRPs) in the elderly. This study aimed to determine the effect of pharmacists’ medication reviews on geriatric patients. This study accessed two online databases, MEDLINE Complete and Scopus, and examined all studies published in English between 2019 and 2023, except for reviews. The studies included (1) participants over 65 years of age and (2) medication reviews conducted by pharmacists. The titles, abstracts, and full texts were reviewed for data extraction to determine whether the studies satisfied the inclusion and exclusion criteria. Forty-four of the initial 709 articles were included in this study. The articles included discussions on the incidence rates of DRPs and potentially inappropriate medications (PIMs) (n=21), hospitalization (n=14), medication adherence (n=9), quality of life (QoL) (n=8), and falls (n=7). Pharmacist medication reviews were associated with a reduced incidence of DRPs and PIMs, and improved adherence to medications. Patients’ overall QoL is also increasing. However, pharmacist medication reviews were not strongly associated with decreased hospitalization or falls. A pharmacist’s medication review may be a feasible intervention for reducing the incidence rates of DRPs and PIMs, regardless of whether it is performed as a sole intervention or supplemented with other interventions. The intervention was also effective in increasing medication adherence and QoL.
INTRODUCTION
The United Nations World Population Aging Report stated that there were approximately 703 million people aged over 65 years worldwide in 2019. Better healthcare and hygiene, healthier lifestyles, sufficient resources, and lower child mortality mean in recent years have contributed significantly to better life expectancy in the current generation [1]. Similarly, the Africa Aging: 2020 International Population Reports estimated that there are 1.05 billion people over 60 years of age in the global population. This number is projected to increase by over 8% to over 2 billion, accounting for 21.6% of the global population in the near future [2]. However, the increase in morbidity may be risking the general population to age-related issues such as impaired physical and mental abilities, thus increasing the need for elderly care in clinical settings. Studies have shown a link between increasing age in the general population and decreasing quality of life (QoL), including decreasing mobility, increasing difficulty in conducting daily activities, and deteriorating health [3].
Individuals of advanced age are also susceptible to falls. Three million older adults are treated in emergency rooms for falls every year. Most cases of falls do not pose a further risk of injury. However, it was found that one in every five cases of falls may lead to serious injury, such as broken bones or head injury [4]. The elderly population is generally at risk of more than one concurrent medical condition that defines multimorbidity, and may require adherence to several medication regimens, known as polypharmacy. Therefore, polypharmacy may not always be harmful. However, brain changes may alter the way people think and behave [5], which may later influence inappropriate drug consumption. Medication errors and drug-related problems (DRPs) were more apparent in elderly patients than in any other age group. Noncompliance with medical treatment and lack of cooperation in patients over 65 years old are also associated with numerous age-related issues, including cognitive impairment [6].
All issues of polypharmacy among elderly patients can be overcome with proper interventions by medical professionals such as proper medication reviews and follow-ups. DRPs can often be discerned and followed by other interventions such as withdrawing unnecessary drugs or drugs with no valid clinical indications. In clinical practice, pharmacists are not as actively involved in medication reviews as physicians. Therefore, this study aimed to review the impact of medication reviews made explicitly by pharmacists on geriatric patients with DRPs in previously published studies to explore the efficacy of such interventions in addressing DRPs, potentially inappropriate medications (PIMs), hospitalization, falls, medication adherence, and QoL.
This scoping review aimed to help healthcare providers investigate a summary that includes a comprehensive yet reliable source of information on the impact of pharmacists’ medication reviews on geriatric patients. This review is also essential for identifying gaps in current studies and highlighting areas that need further inquiry for future reference. Additionally, this study contributes to the field of knowledge on this topic.
METHODOLOGY
This scoping review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) Protocols. The Population, Intervention, Comparison, Outcomes and Study (PICOS) framework used in this study is outlined in the inclusion criteria. The scoping review was performed successively according to the critically-acclaimed research framework suggested in the paper “Scoping studies: towards a methodological framework.” [7]
1. Research Question
In this review article, the research question was constructed using the PICOS framework, focusing on geriatric patients aged 65 years and older. The intervention of interest was a medication review, whereas the comparison group consisted of geriatric patients who did not undergo any medication review. The outcomes were categorized into primary and secondary outcomes, as detailed in the inclusion criteria. The following research questions guided this study: (1) What are the effects of pharmacists’ medication reviews on DRPs and PIM use in geriatric patients? (2) What is the effect of pharmacist-conducted medication reviews on the occurrence of falls among geriatric patients? (3) What is the influence of pharmacist-conducted medication reviews on hospitalization rates among geriatric patients? (4) What are the effects of pharmacist-conducted medication reviews on adherence among geriatric patients? (5) How do pharmacist-conducted medication reviews affect the QoL of geriatric patients?
2. Inclusion and Exclusion Criteria
The inclusion criteria for this review encompassed studies involving participants aged 65 years and older situated across diverse care settings such as home care, hospitals, clinics, homes, and community pharmacies. They included studies that focused on medication reviews, which encompassed a range of activities including prescription reviews, adherence support reviews, clinical reviews, clinical reviews with prescriptions, and home medication reviews. These interventions can be participatory, led by pharmacists, or performed entirely by pharmacists. The primary outcome of interest was the assessment of DRPs and PIMs in the target population. Additionally, the review considered studies exploring secondary outcomes, including medication adherence, incidence of falls, hospitalization rates, and the impact of these interventions on participants’ QoL. The temporal scope of this review was limited to studies published between 2019 and 2023.
The exclusion criteria encompassed studies focusing exclusively on participants under the age of 65 years or those conducted in care settings that were not specified in the inclusion criteria. Studies unrelated to medication reviews or interventions that lacked pharmacist involvement were also excluded. Furthermore, studies that failed to report DRPs, PIM, or any of the specified secondary outcomes were excluded. Studies not available in English or without an English translation were excluded from this review. Finally, scoping reviews, systematic reviews, meta-analyses, and other review studies that deviated from the primary research focus of this review were also excluded.
3. Search Strategies
This study systematically examined global research papers published between 2019 and 2023 focusing on the effects of pharmacist-conducted medication reviews on geriatric patients. The literature search was conducted on March 1, 2023, using two prominent databases: MEDLINE Complete and Scopus. The search strategy aimed to identify studies reporting improvements in drug-related issues and PIM usage among geriatric patients while also assessing outcomes such as falls, hospitalization rates, medication adherence, and QoL. To capture relevant articles, specific search terms were employed, and the detailed search strings for Scopus and MEDLINE can be found in Table 1, outlining the amalgamation of keywords such as “Medication review,” “Pharmacist,” “Geriatric,” and related terms using Boolean operators “OR” and “AND.”
4. Study Selection and Extraction
The study selection process involved two primary reviewers (A.H. and H.K.) who initially screened the study titles and abstracts based on established inclusion and exclusion criteria. Subsequently, the full texts of the relevant studies were obtained and independently evaluated. To ensure comprehensiveness, the references of the selected publications were meticulously examined to identify any additional research that may have been missed during the initial database search. In cases in which two primary reviewers (A.H. and H.K.) encountered discrepancies or disagreements during their assessments, the input of a third reviewer (C.Y.) was sought for resolution. The data extracted from these selected studies were carefully documented and organized into evidence tables, including critical information such as the authors, publication year, country of origin, study design, research objectives, methods, interventions, and key findings from each study (Supplement 1).
RESULTS
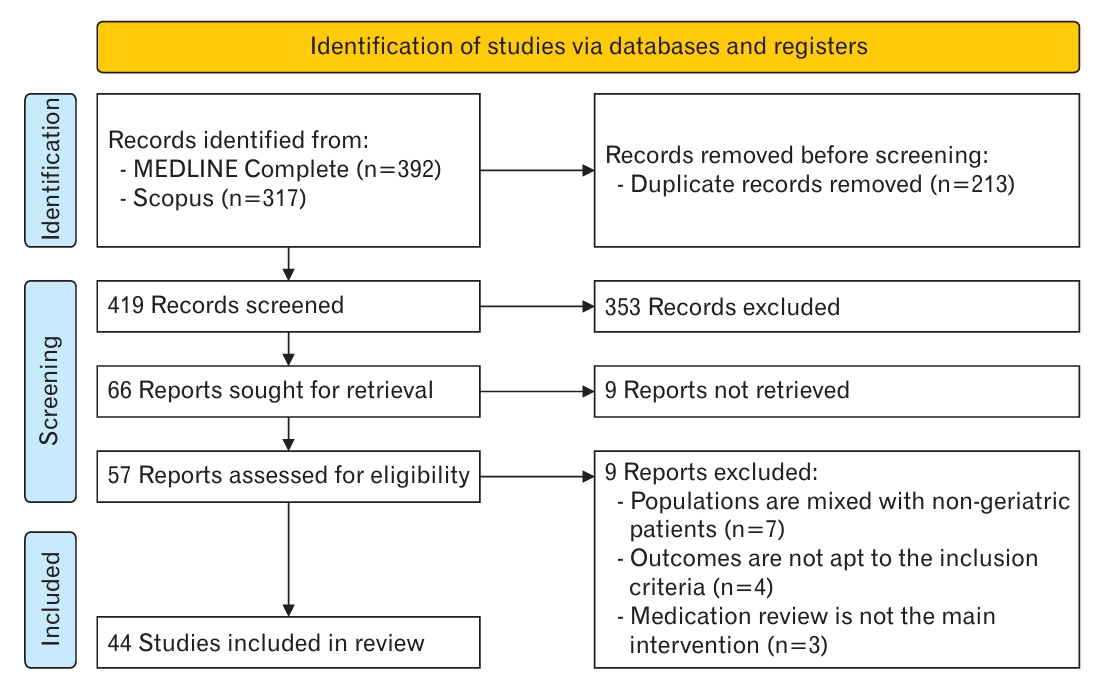
In Figure 1, a PRISMA flowchart is shown to visually depict the selection process at each study stage. The initial identification phase yielded 392 and 317 articles from MEDLINE Complete and Scopus, respectively. During this phase, all relevant articles were identified. Subsequently, 213 duplicate articles were removed to streamline the datasets for further analysis. As we progressed, 353 of the initial 419 articles were excluded. These exclusions were primarily due to irrelevance to the primary objectives of the study, non-alignment with the specified outcomes, focus on populations unrelated to the target demographics, or classification as review articles.
Subsequently, the remaining 66 reports were retrieved. Unfortunately, despite earnest attempts to contact the authors, nine articles remained inaccessible in full-text format, prompting their exclusion. Finally, 57 studies were meticulously assessed for eligibility. During this process, seven papers were excluded because they encompassed mixed populations, including non-geriatric patients. Additionally, four articles did not meet the predefined inclusion criteria, and three others did not focus primarily on medication reviews as the core intervention. Consequently, 44 eligible articles were selected for inclusion in this comprehensive review.
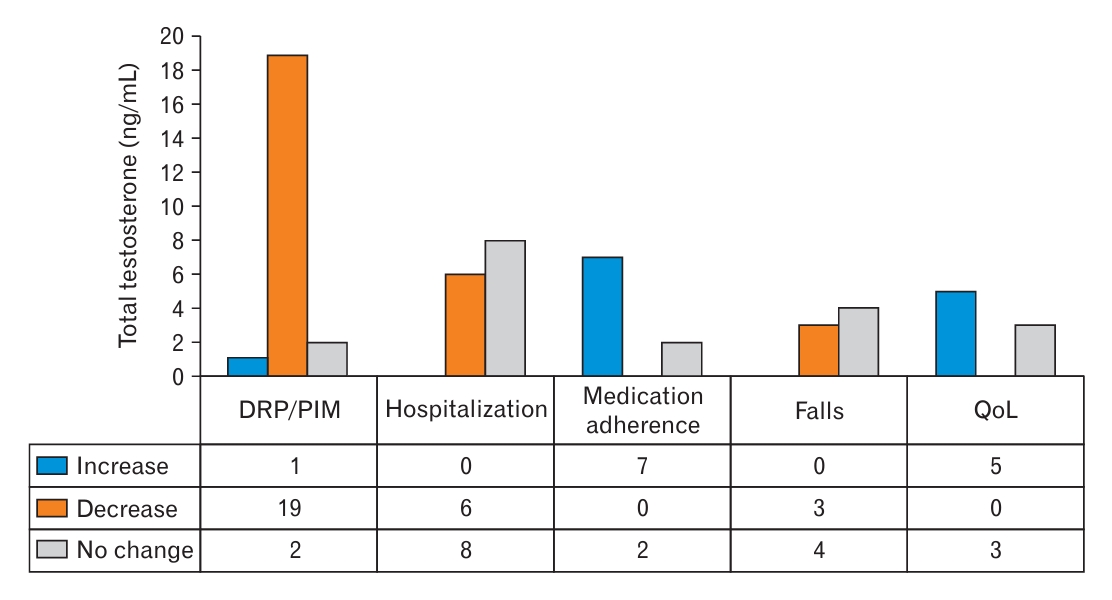
Figure 2 provides an illustrative overview of the diverse study designs that constitute the corpus of this review. Figure 3 presents a visual representation of the impact of pharmacist-conducted medication reviews on geriatric patients, providing valuable insights into the investigation outcomes.
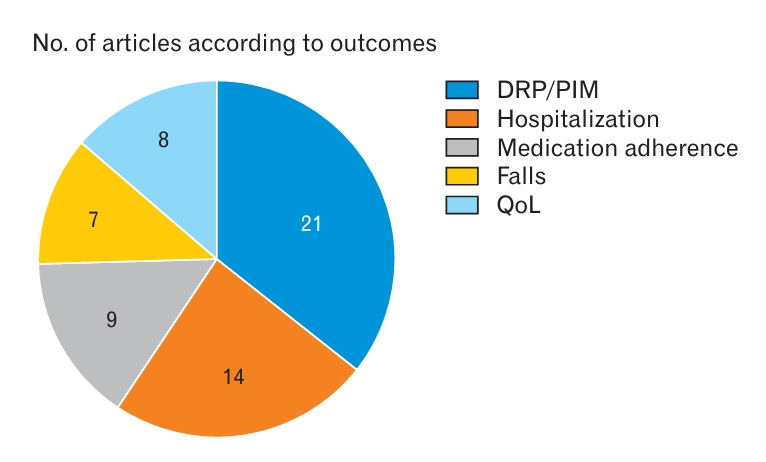
Number of articles according to outcomes. DRP, drug-related problem; PIM, potentially inappropriate medication; QoL, quality of life.
DISCUSSION
1. Rate of Incidence of Drug-Related Problems and Potentially Inappropriate Medication
The primary outcomes indicated that 90% of the studies agreed on the positive impact of pharmacist medication reviews on the rates of DRPs and PIMs. In this review, DRPs and PIMs were combined into a single category as the primary outcomes. However, the number of studies explicitly addressing DRPs is smaller than those focusing on PIMs based on this categorization. Six of the 21 articles discussed DRPs, whereas the remaining articles focused on PIMs (Table 2) [8-28].
A significant number of studies supporting a decrease in the rates of DRPs and PIMs were of particular interest, thus prompting this study to examine the characteristics of the included articles. There was no substantial variation in sample sizes across the selected articles, except for the study by Sluggett et al. [8] which was conducted with a large sample size of 11,309 participants. This variation is attributed to the cohort study design employed in the study. Most articles included medication reviews as the sole intervention. However, the studies conducted by Dumlu et al. [9] and Liou et al. [10] supplemented medication reviews with additional interventions, such as patient education or the distribution of administration aids, such as pill cutters.
The articles included in this study shared one similarity: the investigation of the interventions applied to PIMs and DRPs. This similarity may explain the high degree of agreement, with 90.47% of the studies reporting a positive impact of pharmacists’ medication reviews on the rates of DRPs and PIMs. These findings suggest that medication reviews, implemented alone or in combination with other interventions, are effective in reducing the incidence of DRPs and PIMs in geriatric patients.
It is important to acknowledge that the positive impact observed in these studies supports the value of pharmacist medication reviews in optimizing medication therapy and reducing the risks associated with inappropriate medications. However, future studies should explore the specific factors and mechanisms underlying the success of medication reviews in addressing DRPs and PIMs. Additionally, future studies are recommended to investigate the long-term effects of medication reviews on patient outcomes, as well as the potential cost-effectiveness of implementing this intervention in different healthcare settings.
2. Hospitalization
The hospitalization category in this study included various measures, such as 30-day readmission, medication-related admission, all-cause admission, and emergency department (ED) visits. Most articles included in this review indicated that pharmacists’ medication reviews did not significantly affect the rate of hospitalization (Table 3) [8,11,12,17,18,21,28-49].
Most articles discussing hospitalization focused on medication reviews without any additional interventions. However, three studies by Kua et al. [29] in 2020, Santolaya-Perrín et al. [30], and Zwietering et al. [31] included other healthcare professionals such as geriatricians and nurses as part of the medication review process. No other supplementary interventions were used in the articles, despite the presence of a multidisciplinary medication review.
Nevertheless, heterogeneity in study designs was reflected in the widely varying sample sizes across studies. The first study by Zwietering et al. [31], for instance, is a before-and-after study involving 200 participants, which concluded that there is no significant difference in the rate of hospitalization. However, another study conducted by Lapointe-Shaw et al. [32] is a cohort study that analyzed data from 879,497 patients and reported a significant decrease in hospitalization rates following a community pharmacist medication review. One notable difference between these two studies was the substantial disparity in sample size. This variation in sample size may have influenced the level of significance observed in the analyzed outcomes. Additionally, the before-and-after study by Zwietering et al. [31] involved a pharmacist and geriatrician in the intervention, whereas the cohort study by Lapointe-Shaw et al. [32] relied solely on community pharmacist medication reviews.
It is essential to interpret these findings with caution because of the differences in study design, sample size, and involvement of other healthcare professionals. Further research is needed to explore the potential benefits and limitations of pharmacist medication reviews in reducing hospitalization rates among geriatric patients. Considering the complex nature of hospitalization, future studies should investigate the effectiveness of pharmacist-led interventions complemented by other interventions, such as care coordination, patient education, and transitional care services. In addition, the fact that this study grouped 30-day readmission, medication-related admission, all-cause admission, and ED visits into one category may also have contributed to the inconclusive results.
3. Medication Adherence
More than 70% of the articles included in this review agreed that pharmacists’ medication reviews lead to increased medication adherence among geriatric patients (Table 3). Only two studies reported no significant differences in medication adherence, and none suggested a decrease after the medication review intervention. These findings indicated a strong association between medication reviews and improved medication adherence.
Medication adherence has been assessed using various methods in different studies. The most commonly utilized tools include the Morisky Medication Adherence Scale and MedAdhiR, as well as non-tool-related methods such as pill counting and comparing prescription fill data. However, it is essential to highlight the need for established and validated tools to ensure accurate results when assessing medication adherence. One study that reported no significant difference in medication adherence did not employ any standardized tools and relied solely on hospital prescription data [33]. This raises concerns regarding potential data bias and highlights the importance of using appropriate measurement tools.
Furthermore, it is noteworthy that the study reporting no significant differences in medication adherence was the only one conducted within a multidisciplinary team setting rather than being solely pharmacist-led. Pharmacists and other healthcare providers commonly undergo training before conducting medication reviews. This training aspect was evident in several studies such as those conducted by Meyer et al. [34], Okuyan et al. [35], and Bosch-Lenders et al. [33]. Based on this observation, it can be inferred that training healthcare providers before they engage in medication reviews plays a crucial role in determining the success of the intervention in increasing medication adherence among patients.
One of the studies conducted by Okuyan et al. [35] did not rely solely on pharmacists’ medication reviews as an intervention. It also incorporates patient counselling and education. This combination of interventions may have contributed to increased medication adherence.
4. Falls
Seven articles were further examined to analyze falls as an outcome (Table 3). The findings indicated that the intervention did not have a significant impact on falls. Four of the reviewed articles concluded that falls were not significantly affected, whereas the remaining three studies reported a decrease in falls after the clinical intervention. The intervention across these studies was relatively homogeneous, with pharmacists being the primary healthcare providers involved in medication reviews. However, the study by Kua et al. [29] implemented a multidisciplinary team approach to medication review.
One aspect that varied significantly among studies was the methods and tools used to assess falls. Some examples include the study conducted by Wuyts et al. [11], which used a self-report questionnaire. In contrast, the study conducted by Blalock et al. [36] relied on claims records from the ED to assess the number of fall episodes. This heterogeneity in fall assessment may have contributed to the inconsistency in the overall findings regarding the impact of pharmacists’ medication reviews on falls.
The similarity in the interventions described in the articles implies that a medication review alone may not be the most effective intervention for reducing falls. Supplementing medication reviews with other interventions, such as home risk assessment and modification, education, and counselling, may be beneficial. These additional components can address factors beyond medication management that contribute to falls, such as environmental hazards and patient education regarding fall prevention strategies.
Further studies are required to make firmer conclusions about the contribution of pharmacists’ medication reviews to fall reduction. Future research should aim to develop standardized techniques for assessing fall events to enable better comparisons between therapies. Furthermore, investigating the efficacy of integrated interventions that include medication reviews and other fall prevention techniques may provide a more thorough picture of optimizing outcomes to decrease falls among older patients.
5. Quality of Life
Five of the eight articles that discussed QoL found evidence supporting the positive impact of pharmacists’ medication reviews on this outcome (Table 3). However, the remaining three studies concluded that this intervention did not result in any significant changes in the QoL. Unlike other outcomes, QoL is a more easily quantifiable measure owing to the widespread use of standardized tools such as the EuroQoL 5-Dimension and Short-Form 12-item version 2 (assessing physical and mental aspects). Notably, within the study pool, all three studies reporting no significant impact were randomized controlled trials (RCTs), while the studies supporting a positive impact on QoL employed different study designs, including quasi-experimental and observational designs.
Various study designs may have led to conflicting findings. Although RCTs are often regarded as the gold standard for evaluating treatments, they may have certain drawbacks when researching complicated interventions such as pharmacist medication reviews. Issues with blinding, practical applications, and unique patient preferences and characteristics may impact RCT results. Quasi-experimental and observational studies provide essential information regarding the efficacy of these therapies. They frequently mirror common clinical practices and include a variety of patient demographics, giving them a higher level of external validity. However, they may be subject to bias and confounding variables, which may affect the findings. It is crucial to interpret these contradictory findings with caution. Further studies are required to better understand the connection between pharmacists’ medication reviews and QoL. Future studies may help solve the gaps in the existing literature by using solid study designs, more significant sample sizes, and extended follow-up periods. A more profound understanding of patients’ experiences and opinions regarding the influence of pharmacists’ medication reviews on their QoL may also be achieved by adding patient-centered outcomes and qualitative research techniques, such as in-depth interviews or focus groups.
Although most articles in this review highlight the beneficial effects of pharmacist medication reviews on geriatric patients’ QoL, conflicting results from RCTs point to the need for more thorough research to reach a more definitive conclusion on this issue. The articles written by Okuyan et al. [35] and Bonnerup et al. [37] further discussed this point. In the first study, a significant increase was detected, whereas in the second study, no significant change was observed. The first was a pilot study with 52 participants, whereas the second was an RCT with 369 participants. In addition, the first study did not use medication review as the sole intervention but was supplemented by patients’ education, counselling services, medicine bag check-ups, and so forth. The second study used medication reviews as the sole intervention. Hence, it is assumed that the difference in outcomes is due to the difference in the interventions applied as well as the sample sizes.
6. Limitations
This scoping review has several limitations that should be addressed in future studies. First, it was limited to studies published explicitly in English, which may have led to the exclusion of relevant studies published in other languages. This is heavily due to the researchers’ monolingual limitations in comprehending studies in other languages. Additionally, only two databases were accessed, MEDLINE Complete and Scopus; thus, excluding relevant studies that may have been published in different databases. Furthermore, the risk of bias or further assessment of the articles included in the studies were not included in this review because the scoping review did not involve a critical appraisal. Another limitation is that scoping reviews generally prioritize breadth over depth, frequently focusing on discovering and categorizing the existing literature rather than comprehensively synthesizing findings. Therefore, the results of this scoping review may be tentative and less conclusive than those of a systematic review. Despite these limitations, the results are said to be agreeable and of high quality because this study assessed only peer-reviewed articles from a trusted database.
Future researchers should broaden the language inclusion criteria beyond English to include relevant studies published in other languages, thereby reducing language bias. Searching beyond MEDLINE Complete and Scopus ensures a more thorough coverage of relevant studies. Future researchers can integrate a risk of bias assessment or quality review of the included papers to improve rigor. Additionally, future researchers could consider various subtypes of outcomes, such as unintentional and intentional non-adherence [50]. In addition, future researchers could consider conducting a systematic review that involves a more rigorous methodology that would provide a more conclusive analysis of the topic. Furthermore, collaboration with experts and diverse research teams can bring valuable insights and expertise, and add even more value to the study.
CONCLUSION
The data from the analyzed articles indicate that pharmacists’ medication reviews have a positive impact on various geriatric patient outcomes. Many studies have reported a considerable reduction in the rate of DRPs and use of PIMs. Furthermore, studies have shown that pharmacists’ medication reviews improve adherence and QoL in elderly patients.
However, the evidence is less conclusive regarding other outcomes such as falls and hospitalization. While some studies have reported decreased fall episodes, the impact on hospitalization rates remains inconclusive with mixed results across studies. Heterogeneity in the study designs, interventions, and assessment methods for these outcomes may have contributed to the varied findings.
The articles included in this review primarily focused on pharmacist-led medication reviews, which are often conducted as standalone interventions. These findings suggest that supplementing medication reviews with other interventions, such as home risk assessment, education, and counselling, may enhance its effectiveness in reducing falls and hospitalizations.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
We thank the Faculty of Pharmacy UiTM, Faculty of Pharmacy UniSZA, Faculty of Health Sciences UiTM, College of Pharmacy, Qatar University, and Faculty of Pharmacy, Quest University, for their support in performing and reporting this scoping review.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4082/kjfm.23.0220.
Table of evidence on included studies