|
 |
- Search
| Korean J Fam Med > Volume 45(3); 2024 > Article |
|
This article has been corrected. See "Erratum: The Impact of Pharmacist Medication Reviews on Geriatric Patients: A Scoping Review" in Volume 45 on page 235.
Abstract
Medication review is an intervention with the potential to reduce drug-related problems (DRPs) in the elderly. This study aimed to determine the effect of pharmacistsŌĆÖ medication reviews on geriatric patients. This study accessed two online databases, MEDLINE Complete and Scopus, and examined all studies published in English between 2019 and 2023, except for reviews. The studies included (1) participants over 65 years of age and (2) medication reviews conducted by pharmacists. The titles, abstracts, and full texts were reviewed for data extraction to determine whether the studies satisfied the inclusion and exclusion criteria. Forty-four of the initial 709 articles were included in this study. The articles included discussions on the incidence rates of DRPs and potentially inappropriate medications (PIMs) (n=21), hospitalization (n=14), medication adherence (n=9), quality of life (QoL) (n=8), and falls (n=7). Pharmacist medication reviews were associated with a reduced incidence of DRPs and PIMs, and improved adherence to medications. PatientsŌĆÖ overall QoL is also increasing. However, pharmacist medication reviews were not strongly associated with decreased hospitalization or falls. A pharmacistŌĆÖs medication review may be a feasible intervention for reducing the incidence rates of DRPs and PIMs, regardless of whether it is performed as a sole intervention or supplemented with other interventions. The intervention was also effective in increasing medication adherence and QoL.
The United Nations World Population Aging Report stated that there were approximately 703 million people aged over 65 years worldwide in 2019. Better healthcare and hygiene, healthier lifestyles, sufficient resources, and lower child mortality mean in recent years have contributed significantly to better life expectancy in the current generation [1]. Similarly, the Africa Aging: 2020 International Population Reports estimated that there are 1.05 billion people over 60 years of age in the global population. This number is projected to increase by over 8% to over 2 billion, accounting for 21.6% of the global population in the near future [2]. However, the increase in morbidity may be risking the general population to age-related issues such as impaired physical and mental abilities, thus increasing the need for elderly care in clinical settings. Studies have shown a link between increasing age in the general population and decreasing quality of life (QoL), including decreasing mobility, increasing difficulty in conducting daily activities, and deteriorating health [3].
Individuals of advanced age are also susceptible to falls. Three million older adults are treated in emergency rooms for falls every year. Most cases of falls do not pose a further risk of injury. However, it was found that one in every five cases of falls may lead to serious injury, such as broken bones or head injury [4]. The elderly population is generally at risk of more than one concurrent medical condition that defines multimorbidity, and may require adherence to several medication regimens, known as polypharmacy. Therefore, polypharmacy may not always be harmful. However, brain changes may alter the way people think and behave [5], which may later influence inappropriate drug consumption. Medication errors and drug-related problems (DRPs) were more apparent in elderly patients than in any other age group. Noncompliance with medical treatment and lack of cooperation in patients over 65 years old are also associated with numerous age-related issues, including cognitive impairment [6].
All issues of polypharmacy among elderly patients can be overcome with proper interventions by medical professionals such as proper medication reviews and follow-ups. DRPs can often be discerned and followed by other interventions such as withdrawing unnecessary drugs or drugs with no valid clinical indications. In clinical practice, pharmacists are not as actively involved in medication reviews as physicians. Therefore, this study aimed to review the impact of medication reviews made explicitly by pharmacists on geriatric patients with DRPs in previously published studies to explore the efficacy of such interventions in addressing DRPs, potentially inappropriate medications (PIMs), hospitalization, falls, medication adherence, and QoL.
This scoping review aimed to help healthcare providers investigate a summary that includes a comprehensive yet reliable source of information on the impact of pharmacistsŌĆÖ medication reviews on geriatric patients. This review is also essential for identifying gaps in current studies and highlighting areas that need further inquiry for future reference. Additionally, this study contributes to the field of knowledge on this topic.
This scoping review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) Protocols. The Population, Intervention, Comparison, Outcomes and Study (PICOS) framework used in this study is outlined in the inclusion criteria. The scoping review was performed successively according to the critically-acclaimed research framework suggested in the paper ŌĆ£Scoping studies: towards a methodological framework.ŌĆØ [7]
In this review article, the research question was constructed using the PICOS framework, focusing on geriatric patients aged 65 years and older. The intervention of interest was a medication review, whereas the comparison group consisted of geriatric patients who did not undergo any medication review. The outcomes were categorized into primary and secondary outcomes, as detailed in the inclusion criteria. The following research questions guided this study: (1) What are the effects of pharmacistsŌĆÖ medication reviews on DRPs and PIM use in geriatric patients? (2) What is the effect of pharmacist-conducted medication reviews on the occurrence of falls among geriatric patients? (3) What is the influence of pharmacist-conducted medication reviews on hospitalization rates among geriatric patients? (4) What are the effects of pharmacist-conducted medication reviews on adherence among geriatric patients? (5) How do pharmacist-conducted medication reviews affect the QoL of geriatric patients?
The inclusion criteria for this review encompassed studies involving participants aged 65 years and older situated across diverse care settings such as home care, hospitals, clinics, homes, and community pharmacies. They included studies that focused on medication reviews, which encompassed a range of activities including prescription reviews, adherence support reviews, clinical reviews, clinical reviews with prescriptions, and home medication reviews. These interventions can be participatory, led by pharmacists, or performed entirely by pharmacists. The primary outcome of interest was the assessment of DRPs and PIMs in the target population. Additionally, the review considered studies exploring secondary outcomes, including medication adherence, incidence of falls, hospitalization rates, and the impact of these interventions on participantsŌĆÖ QoL. The temporal scope of this review was limited to studies published between 2019 and 2023.
The exclusion criteria encompassed studies focusing exclusively on participants under the age of 65 years or those conducted in care settings that were not specified in the inclusion criteria. Studies unrelated to medication reviews or interventions that lacked pharmacist involvement were also excluded. Furthermore, studies that failed to report DRPs, PIM, or any of the specified secondary outcomes were excluded. Studies not available in English or without an English translation were excluded from this review. Finally, scoping reviews, systematic reviews, meta-analyses, and other review studies that deviated from the primary research focus of this review were also excluded.
This study systematically examined global research papers published between 2019 and 2023 focusing on the effects of pharmacist-conducted medication reviews on geriatric patients. The literature search was conducted on March 1, 2023, using two prominent databases: MEDLINE Complete and Scopus. The search strategy aimed to identify studies reporting improvements in drug-related issues and PIM usage among geriatric patients while also assessing outcomes such as falls, hospitalization rates, medication adherence, and QoL. To capture relevant articles, specific search terms were employed, and the detailed search strings for Scopus and MEDLINE can be found in Table 1, outlining the amalgamation of keywords such as ŌĆ£Medication review,ŌĆØ ŌĆ£Pharmacist,ŌĆØ ŌĆ£Geriatric,ŌĆØ and related terms using Boolean operators ŌĆ£ORŌĆØ and ŌĆ£AND.ŌĆØ
The study selection process involved two primary reviewers (A.H. and H.K.) who initially screened the study titles and abstracts based on established inclusion and exclusion criteria. Subsequently, the full texts of the relevant studies were obtained and independently evaluated. To ensure comprehensiveness, the references of the selected publications were meticulously examined to identify any additional research that may have been missed during the initial database search. In cases in which two primary reviewers (A.H. and H.K.) encountered discrepancies or disagreements during their assessments, the input of a third reviewer (C.Y.) was sought for resolution. The data extracted from these selected studies were carefully documented and organized into evidence tables, including critical information such as the authors, publication year, country of origin, study design, research objectives, methods, interventions, and key findings from each study (Supplement 1).
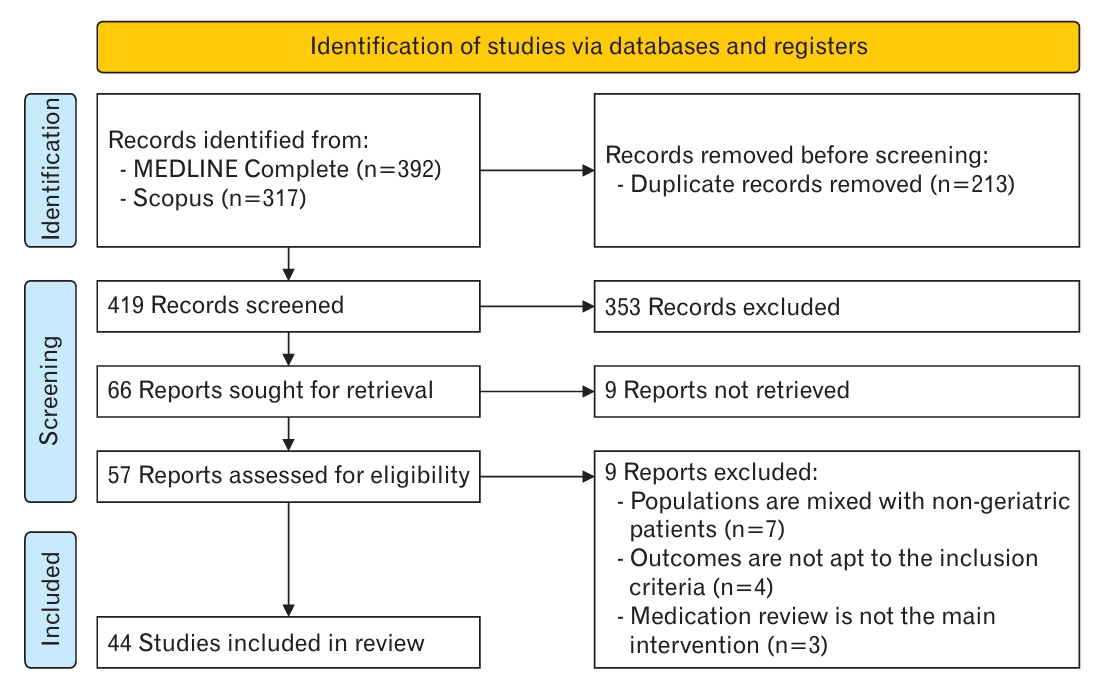
In Figure 1, a PRISMA flowchart is shown to visually depict the selection process at each study stage. The initial identification phase yielded 392 and 317 articles from MEDLINE Complete and Scopus, respectively. During this phase, all relevant articles were identified. Subsequently, 213 duplicate articles were removed to streamline the datasets for further analysis. As we progressed, 353 of the initial 419 articles were excluded. These exclusions were primarily due to irrelevance to the primary objectives of the study, non-alignment with the specified outcomes, focus on populations unrelated to the target demographics, or classification as review articles.
Subsequently, the remaining 66 reports were retrieved. Unfortunately, despite earnest attempts to contact the authors, nine articles remained inaccessible in full-text format, prompting their exclusion. Finally, 57 studies were meticulously assessed for eligibility. During this process, seven papers were excluded because they encompassed mixed populations, including non-geriatric patients. Additionally, four articles did not meet the predefined inclusion criteria, and three others did not focus primarily on medication reviews as the core intervention. Consequently, 44 eligible articles were selected for inclusion in this comprehensive review.
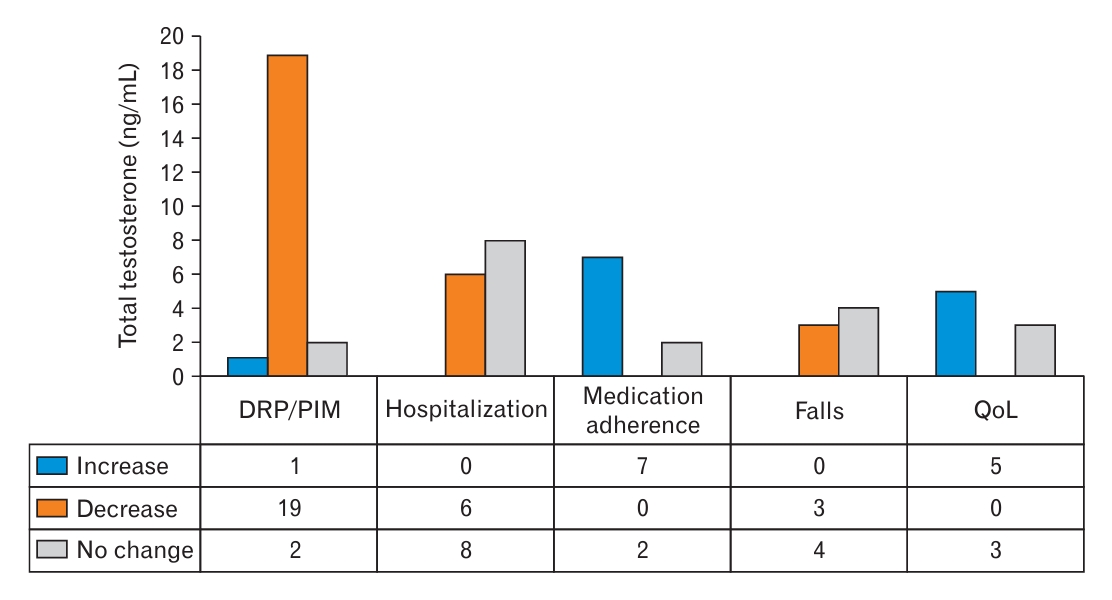
The primary outcomes indicated that 90% of the studies agreed on the positive impact of pharmacist medication reviews on the rates of DRPs and PIMs. In this review, DRPs and PIMs were combined into a single category as the primary outcomes. However, the number of studies explicitly addressing DRPs is smaller than those focusing on PIMs based on this categorization. Six of the 21 articles discussed DRPs, whereas the remaining articles focused on PIMs (Table 2) [8-28].
A significant number of studies supporting a decrease in the rates of DRPs and PIMs were of particular interest, thus prompting this study to examine the characteristics of the included articles. There was no substantial variation in sample sizes across the selected articles, except for the study by Sluggett et al. [8] which was conducted with a large sample size of 11,309 participants. This variation is attributed to the cohort study design employed in the study. Most articles included medication reviews as the sole intervention. However, the studies conducted by Dumlu et al. [9] and Liou et al. [10] supplemented medication reviews with additional interventions, such as patient education or the distribution of administration aids, such as pill cutters.
The articles included in this study shared one similarity: the investigation of the interventions applied to PIMs and DRPs. This similarity may explain the high degree of agreement, with 90.47% of the studies reporting a positive impact of pharmacistsŌĆÖ medication reviews on the rates of DRPs and PIMs. These findings suggest that medication reviews, implemented alone or in combination with other interventions, are effective in reducing the incidence of DRPs and PIMs in geriatric patients.
It is important to acknowledge that the positive impact observed in these studies supports the value of pharmacist medication reviews in optimizing medication therapy and reducing the risks associated with inappropriate medications. However, future studies should explore the specific factors and mechanisms underlying the success of medication reviews in addressing DRPs and PIMs. Additionally, future studies are recommended to investigate the long-term effects of medication reviews on patient outcomes, as well as the potential cost-effectiveness of implementing this intervention in different healthcare settings.
The hospitalization category in this study included various measures, such as 30-day readmission, medication-related admission, all-cause admission, and emergency department (ED) visits. Most articles included in this review indicated that pharmacistsŌĆÖ medication reviews did not significantly affect the rate of hospitalization (Table 3) [8,11,12,17,18,21,28-49].
Most articles discussing hospitalization focused on medication reviews without any additional interventions. However, three studies by Kua et al. [29] in 2020, Santolaya-Perr├Łn et al. [30], and Zwietering et al. [31] included other healthcare professionals such as geriatricians and nurses as part of the medication review process. No other supplementary interventions were used in the articles, despite the presence of a multidisciplinary medication review.
Nevertheless, heterogeneity in study designs was reflected in the widely varying sample sizes across studies. The first study by Zwietering et al. [31], for instance, is a before-and-after study involving 200 participants, which concluded that there is no significant difference in the rate of hospitalization. However, another study conducted by Lapointe-Shaw et al. [32] is a cohort study that analyzed data from 879,497 patients and reported a significant decrease in hospitalization rates following a community pharmacist medication review. One notable difference between these two studies was the substantial disparity in sample size. This variation in sample size may have influenced the level of significance observed in the analyzed outcomes. Additionally, the before-and-after study by Zwietering et al. [31] involved a pharmacist and geriatrician in the intervention, whereas the cohort study by Lapointe-Shaw et al. [32] relied solely on community pharmacist medication reviews.
It is essential to interpret these findings with caution because of the differences in study design, sample size, and involvement of other healthcare professionals. Further research is needed to explore the potential benefits and limitations of pharmacist medication reviews in reducing hospitalization rates among geriatric patients. Considering the complex nature of hospitalization, future studies should investigate the effectiveness of pharmacist-led interventions complemented by other interventions, such as care coordination, patient education, and transitional care services. In addition, the fact that this study grouped 30-day readmission, medication-related admission, all-cause admission, and ED visits into one category may also have contributed to the inconclusive results.
More than 70% of the articles included in this review agreed that pharmacistsŌĆÖ medication reviews lead to increased medication adherence among geriatric patients (Table 3). Only two studies reported no significant differences in medication adherence, and none suggested a decrease after the medication review intervention. These findings indicated a strong association between medication reviews and improved medication adherence.
Medication adherence has been assessed using various methods in different studies. The most commonly utilized tools include the Morisky Medication Adherence Scale and MedAdhiR, as well as non-tool-related methods such as pill counting and comparing prescription fill data. However, it is essential to highlight the need for established and validated tools to ensure accurate results when assessing medication adherence. One study that reported no significant difference in medication adherence did not employ any standardized tools and relied solely on hospital prescription data [33]. This raises concerns regarding potential data bias and highlights the importance of using appropriate measurement tools.
Furthermore, it is noteworthy that the study reporting no significant differences in medication adherence was the only one conducted within a multidisciplinary team setting rather than being solely pharmacist-led. Pharmacists and other healthcare providers commonly undergo training before conducting medication reviews. This training aspect was evident in several studies such as those conducted by Meyer et al. [34], Okuyan et al. [35], and Bosch-Lenders et al. [33]. Based on this observation, it can be inferred that training healthcare providers before they engage in medication reviews plays a crucial role in determining the success of the intervention in increasing medication adherence among patients.
One of the studies conducted by Okuyan et al. [35] did not rely solely on pharmacistsŌĆÖ medication reviews as an intervention. It also incorporates patient counselling and education. This combination of interventions may have contributed to increased medication adherence.
Seven articles were further examined to analyze falls as an outcome (Table 3). The findings indicated that the intervention did not have a significant impact on falls. Four of the reviewed articles concluded that falls were not significantly affected, whereas the remaining three studies reported a decrease in falls after the clinical intervention. The intervention across these studies was relatively homogeneous, with pharmacists being the primary healthcare providers involved in medication reviews. However, the study by Kua et al. [29] implemented a multidisciplinary team approach to medication review.
One aspect that varied significantly among studies was the methods and tools used to assess falls. Some examples include the study conducted by Wuyts et al. [11], which used a self-report questionnaire. In contrast, the study conducted by Blalock et al. [36] relied on claims records from the ED to assess the number of fall episodes. This heterogeneity in fall assessment may have contributed to the inconsistency in the overall findings regarding the impact of pharmacistsŌĆÖ medication reviews on falls.
The similarity in the interventions described in the articles implies that a medication review alone may not be the most effective intervention for reducing falls. Supplementing medication reviews with other interventions, such as home risk assessment and modification, education, and counselling, may be beneficial. These additional components can address factors beyond medication management that contribute to falls, such as environmental hazards and patient education regarding fall prevention strategies.
Further studies are required to make firmer conclusions about the contribution of pharmacistsŌĆÖ medication reviews to fall reduction. Future research should aim to develop standardized techniques for assessing fall events to enable better comparisons between therapies. Furthermore, investigating the efficacy of integrated interventions that include medication reviews and other fall prevention techniques may provide a more thorough picture of optimizing outcomes to decrease falls among older patients.
Five of the eight articles that discussed QoL found evidence supporting the positive impact of pharmacistsŌĆÖ medication reviews on this outcome (Table 3). However, the remaining three studies concluded that this intervention did not result in any significant changes in the QoL. Unlike other outcomes, QoL is a more easily quantifiable measure owing to the widespread use of standardized tools such as the EuroQoL 5-Dimension and Short-Form 12-item version 2 (assessing physical and mental aspects). Notably, within the study pool, all three studies reporting no significant impact were randomized controlled trials (RCTs), while the studies supporting a positive impact on QoL employed different study designs, including quasi-experimental and observational designs.
Various study designs may have led to conflicting findings. Although RCTs are often regarded as the gold standard for evaluating treatments, they may have certain drawbacks when researching complicated interventions such as pharmacist medication reviews. Issues with blinding, practical applications, and unique patient preferences and characteristics may impact RCT results. Quasi-experimental and observational studies provide essential information regarding the efficacy of these therapies. They frequently mirror common clinical practices and include a variety of patient demographics, giving them a higher level of external validity. However, they may be subject to bias and confounding variables, which may affect the findings. It is crucial to interpret these contradictory findings with caution. Further studies are required to better understand the connection between pharmacistsŌĆÖ medication reviews and QoL. Future studies may help solve the gaps in the existing literature by using solid study designs, more significant sample sizes, and extended follow-up periods. A more profound understanding of patientsŌĆÖ experiences and opinions regarding the influence of pharmacistsŌĆÖ medication reviews on their QoL may also be achieved by adding patient-centered outcomes and qualitative research techniques, such as in-depth interviews or focus groups.
Although most articles in this review highlight the beneficial effects of pharmacist medication reviews on geriatric patientsŌĆÖ QoL, conflicting results from RCTs point to the need for more thorough research to reach a more definitive conclusion on this issue. The articles written by Okuyan et al. [35] and Bonnerup et al. [37] further discussed this point. In the first study, a significant increase was detected, whereas in the second study, no significant change was observed. The first was a pilot study with 52 participants, whereas the second was an RCT with 369 participants. In addition, the first study did not use medication review as the sole intervention but was supplemented by patientsŌĆÖ education, counselling services, medicine bag check-ups, and so forth. The second study used medication reviews as the sole intervention. Hence, it is assumed that the difference in outcomes is due to the difference in the interventions applied as well as the sample sizes.
This scoping review has several limitations that should be addressed in future studies. First, it was limited to studies published explicitly in English, which may have led to the exclusion of relevant studies published in other languages. This is heavily due to the researchersŌĆÖ monolingual limitations in comprehending studies in other languages. Additionally, only two databases were accessed, MEDLINE Complete and Scopus; thus, excluding relevant studies that may have been published in different databases. Furthermore, the risk of bias or further assessment of the articles included in the studies were not included in this review because the scoping review did not involve a critical appraisal. Another limitation is that scoping reviews generally prioritize breadth over depth, frequently focusing on discovering and categorizing the existing literature rather than comprehensively synthesizing findings. Therefore, the results of this scoping review may be tentative and less conclusive than those of a systematic review. Despite these limitations, the results are said to be agreeable and of high quality because this study assessed only peer-reviewed articles from a trusted database.
Future researchers should broaden the language inclusion criteria beyond English to include relevant studies published in other languages, thereby reducing language bias. Searching beyond MEDLINE Complete and Scopus ensures a more thorough coverage of relevant studies. Future researchers can integrate a risk of bias assessment or quality review of the included papers to improve rigor. Additionally, future researchers could consider various subtypes of outcomes, such as unintentional and intentional non-adherence [50]. In addition, future researchers could consider conducting a systematic review that involves a more rigorous methodology that would provide a more conclusive analysis of the topic. Furthermore, collaboration with experts and diverse research teams can bring valuable insights and expertise, and add even more value to the study.
The data from the analyzed articles indicate that pharmacistsŌĆÖ medication reviews have a positive impact on various geriatric patient outcomes. Many studies have reported a considerable reduction in the rate of DRPs and use of PIMs. Furthermore, studies have shown that pharmacistsŌĆÖ medication reviews improve adherence and QoL in elderly patients.
However, the evidence is less conclusive regarding other outcomes such as falls and hospitalization. While some studies have reported decreased fall episodes, the impact on hospitalization rates remains inconclusive with mixed results across studies. Heterogeneity in the study designs, interventions, and assessment methods for these outcomes may have contributed to the varied findings.
The articles included in this review primarily focused on pharmacist-led medication reviews, which are often conducted as standalone interventions. These findings suggest that supplementing medication reviews with other interventions, such as home risk assessment, education, and counselling, may enhance its effectiveness in reducing falls and hospitalizations.
ACKNOWLEDGMENTS
We thank the Faculty of Pharmacy UiTM, Faculty of Pharmacy UniSZA, Faculty of Health Sciences UiTM, College of Pharmacy, Qatar University, and Faculty of Pharmacy, Quest University, for their support in performing and reporting this scoping review.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4082/kjfm.23.0220.
Figure.┬Ā2.
Number of articles according to outcomes. DRP, drug-related problem; PIM, potentially inappropriate medication; QoL, quality of life.
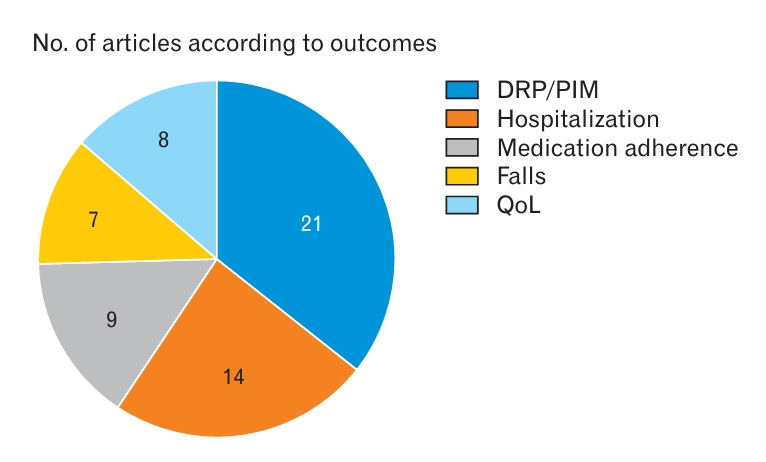
Figure.┬Ā3.
Graph of the impact of pharmacist medication reviews on geriatric patients. DRP, drug-related problem; PIM, potentially inappropriate medication; QoL, quality of life.
Table┬Ā1.
Search strings
Table┬Ā2.
The impact of intervention on DRPs and PIMs
| No. | Author (year) | Primary outcomes (DRP, PIM) |
|---|---|---|
| 1. | Wuyts et al. [11] (2020) | ŌĆĀ |
| 2. | Hashimoto et al. [12] (2020) | * |
| 3. | Stuhec et al. [18] (2019) | * |
| 4. | Garland et al. [26] (2021) | * |
| 5. | Wuyts et al. [11] (2020) | * |
| 6. | Van der Linden et al. [25] (2019) | * |
| 7. | Chen et al. [24] (2019) | ŌĆĀ |
| 8. | Molist-Brunet et al. [23] (2022) | * |
| 9. | Ponjee et al. [22] (2022) | * |
| 10. | Zhang et al. [21] (2022) | * |
| 11. | Gutierrez-Valencia et al. [20] (2019) | * |
| 12. | Pearson et al. [19] (2021) | ŌĆĀ |
| 13. | Stuhec et al. [27] (2019) | * |
| 14. | Liou et al. [10] (2021) | * |
| 15. | Stuhec and Zorjan [17] (2022) | * |
| 16. | Leguelinel-Blache et al. [16] (2020) | * |
| 17. | Dumlu et al. [9] (2021) | * |
| 18. | Choukroun et al. [15] (2021) | * |
| 19. | Mekdad and Elsayed [14] (2019) | * |
| 20. | Khera et al. [13] (2019) | * |
| 21. | Slugget et al. [8] (2022) | * |
| 22. | Desborough et al. [28] (2020) | * |
Table┬Ā3.
Summary of the secondary outcomes following intervention
| No. | Author (year) | Hospitalization | Medication adherence | Falls | Quality of life |
|---|---|---|---|---|---|
| 1. | Meyer et al. [34] (2021) | * | |||
| 2. | Wuyts et al. [11] (2020) | ŌĆĀ | ŌĆĀ | ŌĆĀ | |
| 3. | Okuyan et al. [35] (2021) | * | * | ||
| 4. | Faton et al. [39] (2022) | * | |||
| 5. | Mart├Łnez-Mardone et al. [38] (2023) | * | |||
| 6. | Bosch-Lenders et al. [33] (2021) | ŌĆĀ | ŌĆĀ | ||
| 7. | Bonnerup et al. [37] (2022) | ŌĆĀ | ŌĆĀ | ||
| 8. | Ramsbottom et al. [41] (2022) | * | * | ||
| 9. | Kari et al. [40] (2022) | ŌĆĀ | |||
| 10. | Hashimoto et al. [12] (2020) | ŌĆĪ | |||
| 11. | Gross et al. [44] (2021) | ŌĆĪ | |||
| 12. | Lexow et al. [43] (2022) | ŌĆĀ | ŌĆĀ | ||
| 13. | Blalock et al. [36] (2020) | ŌĆĀ | |||
| 14. | Kua et al. [29] (2020) | ŌĆĪ | ŌĆĀ | ||
| 15. | Gemmeke et al. [42] (2023) | ŌĆĪ | |||
| 16. | Stuhec et al. [18] (2019) | * | |||
| 17. | Zhang et al. [21] (2022) | * | * | ||
| 18. | Stuhec and Zorjan [17] (2022) | * | |||
| 19. | Lapointe-Shaw et al. [32] (2019) | ŌĆĪ | |||
| 20. | Desborough et al. [28] (2020) | ŌĆĪ | * | ||
| 21. | Graab├”k et al. [49] (2019) | ŌĆĀ | |||
| 22. | Johansen et al. [48] (2022) | ŌĆĀ | |||
| 23. | Sloeserwij et al. [47] (2019) | ŌĆĪ | |||
| 24. | Slugget et al. [8] (2022) | ŌĆĪ | |||
| 25. | Santolaya-Perrin et al. [30] (2019) | ŌĆĀ | |||
| 26. | Kempen et al. [46] (2022) | ŌĆĀ | |||
| 27. | Visade et al. [45] (2022) | ŌĆĀ | |||
| 28. | Zwietering et al. [31] (2022) | ŌĆĪ |
REFERENCES
1. Brown GC. Living too long: the current focus of medical research on increasing the quantity, rather than the quality, of life is damaging our health and harming the economy. EMBO Rep 2015;16:137-41.

2. He W, Aboderin I, Adjaye-Gbewonyo D. Africa Aging: 2020 International Population Reports. U.S Census Bureau; 2020.
3. Netuveli G, Wiggins RD, Hildon Z, Montgomery SM, Blane D. Quality of life at older ages: evidence from the English longitudinal study of aging (wave 1). J Epidemiol Community Health 2006;60:357-63.



4. Centers for Disease Control and Prevention. Older adult fall prevention [Internet]. Atlanta (GA): National Center for Injury Prevention and Control; 2021 [cited 2024 Jan 2]. Available from: https://www.cdc.gov/falls/index.html
5. Woodford HJ, George J. Cognitive assessment in the elderly: a review of clinical methods. QJM 2007;100:469-84.


6. Arlt S, Lindner R, Rosler A, von Renteln-Kruse W. Adherence to medication in patients with dementia: predictors and strategies for improvement. Drugs Aging 2008;25:1033-47.

7. Arksey H, OŌĆÖMalley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32.

8. Sluggett JK, Caughey GE, Air T, Moldovan M, Lang C, Martin G, et al. Medicines use before and after comprehensive medicines review among residents of long-term care facilities: a retrospective cohort study. BMC Geriatr 2022;22:493.




9. Dumlu HI, Sancar M, Ozdemir A, Okuyan B. Impact of a clinical pharmacist-led stewardship program for the appropriate use of acid suppression therapy in older hospitalized patients: a non-randomized controlled study. Int J Clin Pharm 2022;44:914-21.



10. Liou WS, Huang SM, Lee WH, Chang YL, Wu MF. The effects of a pharmacist-led medication review in a nursing home: a randomized controlled trial. Medicine (Baltimore) 2021;100:e28023.


11. Wuyts J, Maesschalck J, De Wulf I, De Lepeleire J, Foulon V. Studying the impact of a medication use evaluation by the community pharmacist (Simenon): patient-reported outcome measures. Res Social Adm Pharm 2020;16:1760-7.


12. Hashimoto R, Fujii K, Shimoji S, Utsumi A, Hosokawa K, Tochino H, et al. Study of pharmacist intervention in polypharmacy among older patients: non-randomized, controlled trial. Geriatr Gerontol Int 2020;20:229-37.



13. Khera S, Abbasi M, Dabravolskaj J, Sadowski CA, Yua H, Chevalier B. Appropriateness of medications in older adults living with frailty: impact of a pharmacist-led structured medication review process in primary care. J Prim Care Community Health 2019;10:2150132719890227.




14. Mekdad SS, Alsayed AA. Quality improvement project to reduce drug-related problems (DRPs) and potentially inappropriate medications (PIMs) in geriatrics cardiac clinic in Saudi Arabia. Can Geriatr J 2019;22:49-54.




15. Choukroun C, Leguelinel-Blache G, Roux-Marson C, Jamet C, Martin-Allier A, Kinowski JM, et al. Impact of a pharmacist and geriatrician medication review on drug-related problems in older outpatients with cancer. J Geriatr Oncol 2021;12:57-63.


16. Leguelinel-Blache G, Castelli C, Rolain J, Bouvet S, Chkair S, Kabani S, et al. Impact of pharmacist-led multidisciplinary medication review on the safety and medication cost of the elderly people living in a nursing home: a before-after study. Expert Rev Pharmacoecon Outcomes Res 2020;20:481-90.


17. Stuhec M, Zorjan K. Clinical pharmacist interventions in ambulatory psychogeriatric patients with excessive polypharmacy. Sci Rep 2022;12:11387.




18. Stuhec M, Gorenc K, Zelko E. Evaluation of a collaborative care approach between general practitioners and clinical pharmacists in primary care community settings in elderly patients on polypharmacy in Slovenia: a cohort retrospective study reveals positive evidence for implementation. BMC Health Serv Res 2019;19:118.




19. Pearson SM, Osbaugh NA, Linnebur SA, Fixen DR, Brungardt A, Marcus AM, et al. Implementation of pharmacist reviews to screen for potentially inappropriate medications in patients with cognitive impairment. Sr Care Pharm 2021;36:508-22.


20. Gutierrez-Valencia M, Izquierdo M, Beobide-Telleria I, Ferro-Uriguen A, Alonso-Renedo J, Casas-Herrero A, et al. Medicine optimization strategy in an acute geriatric unit: The pharmacist in the geriatric team. Geriatr Gerontol Int 2019;19:530-6.



21. Zhang S, Zhu D, Qi Z, Tian L, Qian S, Song D, et al. Effects of home medication review on drug-related problems and health-related quality of life among community-dwelling older adults in China. J Am Pharm Assoc (2003) 2022;62:481-6.


22. Ponjee GH, van de Meerendonk HW, Janssen MJ, Karapinar-Carkit F. The effect of an inpatient geriatric stewardship on drug-related problems reported by patients after discharge. Int J Clin Pharm 2021;43:191-202.



23. Molist-Brunet N, Sevilla-Sanchez D, Puigoriol-Juvanteny E, Bajo-Penas L, Cantizano-Baldo I, Cabanas-Collell L, et al. Individualized medication review in older people with multimorbidity: a comparative analysis between patients living at home and in a nursing home. Int J Environ Res Public Health 2022;19:3423.



24. Chen J, Sena K, Nawarskas AD, Smith CA, Ward K. Impact of pharmacy medication reviews on the prescribing of potentially inappropriate medications for older veterans in primary care. Sr Care Pharm 2019;34:464-72.


25. Van Der Linden L, Hias J, Walgraeve K, Loyens S, Flamaing J, Spriet I, et al. Factors associated with the number of clinical pharmacy recommendations: findings from an observational study in geriatric inpatients. Acta Clin Belg 2021;76:119-26.


26. Garland CT, Guenette L, Kroger E, Carmichael PH, Rouleau R, Sirois C. A new care model reduces polypharmacy and potentially inappropriate medications in long-term care. J Am Med Dir Assoc 2021;22:141-7.


27. Stuhec M, Bratovic N, Mrhar A. Impact of clinical pharmacistŌĆÖs interventions on pharmacotherapy management in elderly patients on polypharmacy with mental health problems including quality of life: a prospective non-randomized study. Sci Rep 2019;9:16856.




28. Desborough JA, Clark A, Houghton J, Sach T, Shaw V, Kirthisingha V, et al. Clinical and cost effectiveness of a multi-professional medication reviews in care homes (CAREMED). Int J Pharm Pract 2020;28:626-34.



29. Kua CH, Yeo CY, Tan PC, Char CW, Tan CW, Mak V, et al. Association of deprescribing with reduction in mortality and hospitalization: a pragmatic stepped-wedge cluster-randomized controlled trial. J Am Med Dir Assoc 2021;22:82-9.


30. Santolaya-Perrin R, Calderon-Hernanz B, Jimenez-Diaz G, Galan-Ramos N, Moreno-Carvajal MT, Rodriguez-Camacho JM, et al. The efficacy of a medication review programme conducted in an emergency department. Int J Clin Pharm 2019;41:757-66.



31. Zwietering NA, Linkens AE, van der Kuy PH, Cremers H, van Nie-Visser N, Hurkens KP, et al. Evaluation of a multifaceted medication review in older patients in the outpatient setting: a before-and-after study. Int J Clin Pharm 2023;45:483-90.




32. Lapointe-Shaw L, Bell CM, Austin PC, Abrahamyan L, Ivers NM, Li P, et al. Community pharmacy medication review, death and re-admission after hospital discharge: a propensity score-matched cohort study. BMJ Qual Saf 2020;29:41-51.


33. Bosch-Lenders D, Jansen J, Stoffers HE, Winkens B, Aretz K, Twellaar M, et al. The effect of a comprehensive, interdisciplinary medication review on quality of life and medication use in community dwelling older people with polypharmacy. J Clin Med 2021;10:600.



34. Meyer M, Enguidanos S, Zhu Y, Likar D, Batra R. Community medication education, data, & safety (C-MEDS): findings from a pilot project. J Am Geriatr Soc 2021;69:813-21.

35. Okuyan B, Ozcan V, Balta E, Durak-Albayrak O, Turker M, Sancar M, et al. The impact of community pharmacists on older adults in Turkey. J Am Pharm Assoc (2003) 2021;61:e83-92.

36. Blalock SJ, Ferreri SP, Renfro CP, Robinson JM, Farley JF, Ray N, et al. Impact of STEADI-Rx: a community pharmacy-based fall prevention intervention. J Am Geriatr Soc 2020;68:1778-86.

37. Bonnerup DK, Lisby M, S├”dder EA, Brock B, Truelshoj T, Sorensen CA, et al. Effects of stratified medication review in high-risk patients at admission to hospital: a randomised controlled trial. Ther Adv Drug Saf 2020;11:2042098620957142.




38. Martinez-Mardones F, Benrimoj SI, Ahumada-Canale A, Plaza-Plaza JC, Garcia-Cardenas V. BC clinical impact of medication reviews with follow-up in cardiovascular older patients in primary care: a cluster-randomized controlled trial. Br J Clin Pharmacol 2023;89:2131-43.



39. Faton G, Drubay PA, Vergez G, Faure S. Impact of pharmacist-led shared medication reviews on adherence among polymedicated older patients: an observational retrospective French study. J Am Pharm Assoc (2003) 2022;62:150-6.


40. Kari H, Aijo-Jensen N, Kortejarvi H, Ronkainen J, Yliperttula M, Laaksonen R, et al. Effectiveness and cost-effectiveness of a people-centred care model for community-living older people versus usual care: a randomised controlled trial. Res Social Adm Pharm 2022;18:3004-12.


41. Ramsbottom H, Rutter P, Fitzpatrick R. Post discharge medicines use review (dMUR) service for older patients: cost-savings from community pharmacist interventions. Res Social Adm Pharm 2018;14:203-6.


42. Gemmeke M, Koster ES, van der Velde N, Taxis K, Bouvy ML. Establishing a community pharmacy-based fall prevention service: an implementation study. Res Social Adm Pharm 2023;19:155-66.


43. Lexow M, Wernecke K, Sultzer R, Bertsche T, Schiek S. Determine the impact of a structured pharmacist-led medication review: a controlled intervention study to optimise medication safety for residents in long-term care facilities. BMC Geriatr 2022;22:307.




44. Gross K, King AN, Steadman E. Impact of a pharmacy-led fall prevention program for institutionalized older people. Sr Care Pharm 2021;36:217-22.


45. Visade F, Lambeaux D, Delecluse C, Decaudin B, Puisieux F, Floret E, et al. Implementation of a multi-interventional approach to improve medication safety in older hospitalized patients: feasibility and impact on 30-day rehospitalization rate. Ann Pharm Fr 2022;80:543-53.

46. Kempen TG, Bertilsson M, Hadziosmanovic N, Lindner KJ, Melhus H, Nielsen EI, et al. Effects of hospital-based comprehensive medication reviews including postdischarge follow-up on older patientsŌĆÖ use of health care: a cluster randomized clinical trial. JAMA Netw Open 2021;4:e216303.



47. Sloeserwij VM, Hazen AC, Zwart DL, Leendertse AJ, Poldervaart JM, de Bont AA, et al. Effects of non-dispensing pharmacists integrated in general practice on medication-related hospitalisations. Br J Clin Pharmacol 2019;85:2321-31.




48. Johansen JS, Halvorsen KH, Svendsen K, Havnes K, Robinson EG, Wetting HL, et al. Interdisciplinary collaboration across secondary and primary care to improve medication safety in the elderly (The IMMENSE study): a randomized controlled trial. BMC Health Serv Res 2022;22:1290.




- TOOLS
-
METRICS

-
- 1 Crossref
- Scopus
- 1,848 View
- 54 Download
- Related articles in KJFM
-
The Effect of Trigger Point Injections on Pain in Patients with Advanced Cancer2019 September;40(5)
Effect of physician's antismoking education on patient's amoking behavior.1992 June;13(6)
The impact of physician's brief counseling on the patients' smokinghabit.1992 July;13(7)
The Effect of Brief Intervention on Heavy Drinking Patients in Primary Care.2005 February;26(2)